In modern medicine, steatohepatitis means an inflammatory disease of the liver, which consists of its fatty degeneration. Depending on the factor that caused the inflammation, chronic alcoholic, metabolic non-alcoholic and drug-induced steatohepatitis are distinguished.
Often different forms of steatohepatitis can be combined, but each of them is characterized by specific causes of development, symptoms and treatment methods.
Chronic alcoholic steatohepatitis
in 30% of cases of chronic alcoholism, patients develop steatohepatitis
Chronic alcoholic hepatitis develops gradually as the body's alcohol intoxication increases. Statistics show that in 30% of cases of chronic alcoholism, patients develop steatohepatitis.
The pattern of development of the disease is quite simple. Since almost all alcohol (from 90% to 98%) is metabolized in the liver through oxidation, excessive consumption leads to increased stress on the organ, which can no longer cope with its functions normally.
As a result, various inflammatory processes begin to develop in the liver, which over time, under the influence of constant alcohol intoxication, become chronic and can lead to fatty degeneration of the liver and give rise to steatohepatitis.
Recent studies have shown that acetaldehyde, which is one of the metabolites of alcohol, plays a crucial role in the development of steatohepatitis. Accumulating in the liver, it gradually destroys its cells and tissues, making the normal functioning of the organ impossible.
The following symptoms indicate the development of chronic alcoholic steatohepatitis:
- enlargement of the liver and its significant thickening
- aching pain in the right hypochondrium
- dyspeptic disorders (diarrhea or constipation)
- excessive sweating and thirst
- general weakness
- loss or complete absence of appetite, rapid weight loss
- nausea and vomiting
- development of jaundice and yellowing of the skin
If not treated promptly, chronic alcoholic steatohepatitis can lead to the development of fibrosis or cirrhosis of the liver.
Symptoms
Most often, steatohepatitis is asymptomatic. Sometimes in the later stages of the disease, when the liver cells are almost completely filled with fat, dyspeptic symptoms appear: loss of appetite, nausea, abdominal discomfort. General weakness and malaise are possible.
Asymptomatic enlargement of the liver is often observed. Approximately 15% of patients hospitalized for steatohepatitis develop jaundice3. At the stage of liver cirrhosis, symptoms of impaired synthetic function of the organ appear - a tendency to bleeding, edema, ascites.
Metabolic non-alcoholic steatohepatitis
Despite the fact that for a long period of time in official medicine fatty degeneration of the liver was considered exclusively as a result of alcohol abuse, in the 20th century it was found that steatohepatitis can develop in patients who do not suffer from alcoholism and do not even drink alcohol.
Inflammatory processes in the liver in many cases develop against the background of metabolic disorders in the body
In particular, it turned out that inflammatory processes in the liver in many cases develop against the background of metabolic disorders in the body. Failures in carbohydrate and fat metabolism are of particular importance for the occurrence of the disease.
Impaired functioning of the latter can become a factor in the development of metabolic steatohepatitis, also known as “fatty liver.”
The main causes of the development of metabolic non-alcoholic hepatitis are:
- eating disorder
- chronic diseases of the digestive system (most notably pancreatitis, colitis, etc.)
- obesity
- diabetes
- hyperlipidemia
Medical statistics indicate the highest incidence of steatohepatitis due to obesity. Impaired fat metabolism, which leads to obesity, provokes fatty degeneration of the liver - a condition in which most of the liver cells are “protected” by the so-called neutral fat and for this reason cannot perform their functions.
The more cells that are turned off from the liver, the less power and efficiency of the organ itself becomes, which can have very negative consequences for the body. A specific feature of the clinical picture of metabolic steatohepatitis is the absence of characteristic symptoms indicating liver dysfunction.
Only in cases where fatty degeneration of the liver is accompanied by extensive inflammation can specific liver pain occur. In most cases, the disease is diagnosed accidentally during a medical examination for other health problems.
If symptoms of the disease appear, they look like this:
Drug-induced steatohepatitis
Yellowness of the sclera in liver disease
In addition to metabolic disorders, the development of steatohepatitis, not caused by alcohol intoxication, can be triggered by taking certain medications. The following groups of medications can be considered potentially dangerous to the liver:
- tetracycline antibiotics (Tetracycline, Terramycin, Biomycin)
- synthetic hormonal drugs (especially estrogens, including oral contraceptives)
- calcium antagonists (Verapamil, Diltiazem, Nifedipine)
- aminoquinolones (Plaquenil, Delagil)
- ARV drugs (almost all drugs used to treat HIV)
- antifungal drugs (Amphotericin, Ketoconazole, Fluorocytosine)
- other medications (Amiodarone, Aspirin, Halothane, Nicotinic acid, etc.)
Some people experience liver problems with long-term use of these medications. Most often, the oxidation of fatty acids is disrupted, which leads to the development of steatohepatitis or even cirrhosis of the liver. In the most severe cases, liver tissue necrosis of varying degrees may develop.
The following symptoms indicate the negative effect of drugs on the liver:
- frequent sharp pain in the liver area
- development of cholestatic syndrome (difficulty functioning of the gallbladder)
- development of jaundice and yellowing of the skin
- unpleasant sensations in the skin (itching, irritation, etc.)
The above drugs pose a particular danger to persons with already diagnosed liver disorders (risk group). Under prolonged exposure to hepatic-dangerous drugs, even minor problems in the functioning of the liver can develop into functional disorders, including fatty degeneration. The use of such drugs by persons at risk is only possible under the supervision of a doctor and with the simultaneous use of individually selected hepatoprotectors.
4.Treatment
A generally accepted and universally effective treatment protocol for NASH has not been developed to date. However, in this case, etiopathogenetic therapy (aimed at eliminating the root causes of the disease) most often involves eliminating the above risk factors.
Thus, an individually developed diet is prescribed and other measures are taken to gradually normalize body weight. The intake is canceled or, if necessary, an alternative to medications that are potentially harmful to the liver, which are objectively indicated for the patient, is selected. Hepatoprotectors are prescribed, and according to indications - antibiotics, statins and other drugs.
Diagnosis of steatohepatitis
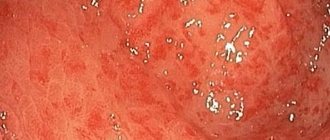
The difficulty of diagnosing steatohepatitis is due to the fact that quite often the disease develops slowly and does not have a clearly defined clinical picture. In many cases, the only symptom that can be a signal for a thorough diagnosis of the liver is an increase in the size of the organ and pain on palpation.
In modern medicine, there are different methods for diagnosing various forms of steatohepatitis. Considering the relatively high frequency of development of the disease against the background of alcoholism, in most cases, a medical examination begins with examining the patient for alcohol abuse.
People with liver disease will have to forget about fatty foods!
Diagnosis of chronic alcoholic steatohepatitis involves the following mandatory steps:
- Ultrasound examination of the liver. Of great importance is the assessment of the degree of enlargement of the organ and changes in its external parameters.
- Laboratory research. High values of some parameters (cholesterol, alkaline phosphatase, immunoglobulin A, bilirubin, triglycerides, etc.) are a direct indication of the development of inflammatory processes in the liver.
If alcoholism has been excluded in the patient, a diagnosis is made for metabolic steatohepatitis:
Prevention and traditional treatment of steatohepatitis
The main prevention of steatohepatitis is aimed at eliminating the factors of their development:
- moderate alcohol consumption
- balanced diet
- timely treatment of diseases that can provoke the development of steatohepatitis
- careful use of medications toxic to the liver with simultaneous use of hepatoprotectors
Treatment of steatohepatitis with timely consultation with specialists in most cases gives a positive prognosis. Only in cases of advanced disease, treatment is associated with certain difficulties and, which is the greatest danger, the risk of developing cirrhosis of the liver.
Diagnostics. Liver palpation
Modern treatment of steatohepatitis involves influencing the body in several directions at once:
- organization of rational nutrition according to a specially selected diet
- normalization of general metabolism in the body and energy metabolism of the liver
- protection of liver cells and stabilization of their condition through drug therapy
- Diet therapy makes it possible to stabilize the condition of the liver as safely as possible and reduce the degree of tissue inflammation. In this regard, it is fundamentally important to organize nutrition in such a way that the body receives a sufficient amount of proteins, which are directly involved in the renewal of the liver.
If steatohepatitis was caused by other diseases, treatment should be aimed at eliminating the manifestations of these particular diseases. Chronic pancreatitis is especially dangerous from the point of view of liver dysfunction and fatty degeneration.
More than 30% of patients suffering from this disease are eventually diagnosed with steatohepatitis or fatty degeneration. In such cases, patients are prescribed drugs that have a positive effect on the functioning of the pancreas: Pancreatin, Creon, Panzinorm, Festal, etc.
Drug therapy is a mandatory component of the treatment of any form of steatohepatitis.
The most commonly used groups of drugs are:
- Drugs that have an antioxidant effect and protect liver cells. Essentiale, Heptral, Berlition, vitamins C and E have proven themselves best.
- Drugs that normalize liver fat metabolism. Most often, patients are prescribed Lipostabil and Lipopharm.
- Combination drugs. The greatest effectiveness in the treatment of various forms of steatohepatitis is demonstrated by Pentoxifylin, Alpha-lipoic acid, Hepabene, Ursodeoxycholic acid, Hepa-merz.
The use of modern drugs makes it possible to cure steatohepatitis in a period of 2 weeks to several months, depending on the degree of development of the disease and the level of damage to liver tissue.
2. Reasons
The causes and mechanisms of development of non-alcoholic fatty degeneration in combination with hepatocyte necrosis (which is the essence of NASH) have not been sufficiently studied. Here, too, epidemiological analysis still provides more accurate information than theoretical or laboratory studies. It has been proven with a high level of significance that NASH most often occurs against the background of the risk factors listed below, which suggests the presence of not only statistical, but also cause-and-effect relationships, which, however, have yet to be substantiated and proven.
The main risk factors for NASH (in addition to age and gender) include:
- excess body weight;
- the presence of type II diabetes mellitus (insulin-resistant, caused by the “blindness” of insulin receptors to this hormone specific to them);
- increased concentration of fatty compounds in the blood (hyperlipidemia);
- prolonged fasting, exhaustion and rapid loss of body weight due to other reasons;
- metabolic disorders (metabolism);
- surgical correction of the structures of the gastrointestinal tract and biliary (bile) system;
- long-term use of certain medications from antibiotic or hormonal groups;
- some congenital anatomical anomalies and diseases (Weber-Christian, Wilson-Konovalov diseases, intestinal diverticulosis, etc.).
Visit our Hepatology page