Introduction
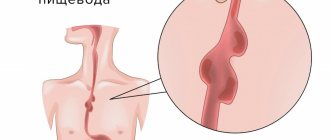
A diverticulum is a sac-like protrusion of the wall of an organ that communicates with it. The prevalence of Zenker's diverticulum, or diverticulum of the pharyngoesophageal junction, is 2 cases per 100,000 patients [1]. This condition was first described in 1769 by A. Ludlow, and in the 19th century. German pathologist Friedrich Albert von Zenker, who gave a detailed description of this condition [2].
The presence of Zenker's diverticulum is usually accompanied by a variety of clinical symptoms of varying severity, which often requires surgical intervention. The main treatment method for patients with Zenker's diverticulum is surgery aimed at removing the diverticulum or eliminating spasm of the cricopharyngeal muscle as one of the causes of diverticulum [3-7]. A large number of surgical treatment options have been proposed, both in the “open” and endoscopic versions, such as excision of the diverticulum, cricopharyngeal myotomy, diverticulopexy or its inversion, endoscopic stapler myotomy, myotomy using a CO2 laser, harmonic scalpel, flexible endoscope [1 , 3-11]. There are publications on the use of robotic technologies to treat patients in this category [12]. In the absence of symptoms of the disease and/or when the diverticulum is small (less than 1 cm), some authors consider the possibility of conservative treatment [1, 6, 10].
Currently, publications on the use of endoscopic interventions for this pathology are increasingly appearing in the literature [2—4, 6, 8, 9, 11]. However, there is no consensus on the choice of treatment for patients with Zenker’s diverticulum [3, 4, 13].
The purpose of the study was to evaluate the capabilities of flexible endoscopy in the treatment of patients with Zenker's diverticulum.
Recommendations
- sind / 2461
in Who named it? - Zenker, F.A.; von Ziemssen, H. W. (1867). Krankheiten des Esophagus
. Leipzig: FCW Vogel. - van Overbeek, JJ (July 2003). "Pathogenesis and treatment methods for Zenc's diverticulum." Anna.
Otol. Rinol. Laryngol .
112
(7):583–93. Doi:10.1177/000348940311200703. PMID 12903677. - Bencini L., Moraldi L., Bartolini I., Coratti A. (January 2016). "Esophageal surgery in the minimally invasive era." World J Gastrointest Surg
.
8
(1):52–64. Doi:10.4240/wjgs.v8.i1.52. PMC 4724588. PMID 26843913. - Sen, P; Bhattacharya, AK (August 2004). "Endoscopic suturing of the pharyngeal pouch." J Laryngol Otol
.
118
(8):601–6. Doi:10.1258/0022215041917817. PMID 15453934. - Chang, C. Y.; Payyapilli, R. J.; Sher, R.L. (June 2003). "Endoscopic staple diverticulostomy for Zenker's diverticulum: a review of the literature and experience in 159 consecutive cases." Laryngoscope
.
113
(6):957–65. Doi:10.1097/00005537-200306000-00009. PMID 12782805. - Altman, JI; Genden, E.M.; Moche, J (May 2005). "Fiberoptic diverticulotomy with endoscopic support: a new method for the treatment of Zenker's diverticulum." Anna.
Otol. Rinol. Laryngol .
114
(5):347–51. Doi:10.1177/000348940511400503. PMID 15966520. - Miller, France; Bartley, J; Otto, R. A. (September 2006). "Endoscopic treatment of Zenker's diverticulum: CO2 laser versus endoscopic stapling." Laryngoscope
.
116
(9):1608–11. Doi:10.1097/01.mlg.0000233508.06499.41. PMID 16954989. - Siddique, M.A.; Court, S; Strachan, D. (August 2001). "Pharynx pouch (Zenker's diverticulum)." Postgraduate Medical Journal
.
77
(910): 506–11. Doi:10.1136/pmj.77.910.506. PMC 1742115. PMID 11470929.
Material and methods
During the period 2016-2018, in the department of thoracic surgery of the State Budgetary Institution of Healthcare NSO "GNOKB", the clinic of the Department of Hospital and Pediatric Surgery of the Faculty of Medicine, intraluminal interventions for Zenker's diverticulum were performed on 31 patients (15 men and 16 women) aged from 36 to 83 years (average - 45.7 years).
All patients were hospitalized in the department with a previously established diagnosis and complaints characteristic of this disease. The duration of complaints ranged from 1 to 8 years. The frequency of detection of complaints is presented in table. 1 .
Table 1. Frequency of complaints in patients with Zenker's diverticulum.
All patients complained of dysphagia. Moreover, the degree of its severity did not depend on the size of the diverticulum and the age of its appearance. More often, patients with small diverticula had more complaints than with large diverticula. This may be due to the patient’s “getting used to” these conditions.
In all cases, patients were forced to limit their diet, in 4 cases - down to semi-liquid and liquid meals, which led to a significant decrease in quality of life.
Before surgery, fluoroscopy of the esophagus, stomach and endoscopic examination were performed to assess the size of the diverticulum and the condition of the mucous membrane of the diverticulum. The sizes of diverticula according to fluoroscopy varied from 15 to 50 mm (median 30 mm). The distribution of patients according to the size of the diverticulum during endoscopic examination is presented in Table. 2 .
Table 2. Characteristics of patients by diverticulum size (endoscopic data).
All interventions were performed in the operating room under general anesthesia with tracheal intubation. Olympus endoscopes (Japan; 180 series) were used using an Olympus CO2 insufflator (Japan). An Olympus needle-knife (Japan) was used to dissect the mucous membrane and cricopharyngeal muscle. Hemostasis was carried out using coagrasper Olympus (Japan). For dissection and hemostasis, an electrosurgical unit “FOTEK” (Russia) was used: dissection in blend cut mode; hemostasis in soft coagulation mode. In 28 (90.3%) patients, surgery was performed using a flexible diverticuloscope (Fig. 1) . The surgical technique consisted of installing a flexible diverticuloscope along an endoscope inserted into the esophagus (Fig. 2, a) and performing a septotomy with myotomy of the cricopharyngeus muscle (m. cricopharyngeus), taking into account the individual anatomical situation in each patient (Fig. 2, b, c ) .
Rice. 1. Flexible diverticuloscope.
Rice. 2. Intraoperative photo: a diverticuloscope is installed and the septum (a) is identified; using a knife-needle, the septum and cricopharyngeal muscle are dissected (b); the cricopharyngeal muscle was dissected (c); the bottom of the wound is clipped (d).
In all cases, the use of a flexible diverticuloscope made it possible to ensure safe stabilization and good visibility of the intervention area by positioning it on the “septum” between the lumen of the esophagus and the diverticulum cavity.
In 3 patients, the intervention was performed using a standard straight translucent cap for dissection at the distal end of the endoscope with a nasogastric tube passed through the esophagus due to the impossibility of installing a flexible diverticuloscope due to the small size of the diverticulum.
Upon completion of the intervention, in 28 (90.3%) patients, a standard endoscopic clip was applied centrally to the wound after septomyotomy (from 1 to 3; Olympus or Endostars; Fig. 2, d ). In 3 (9.7%) patients, clipping was not performed (in 2 cases with small diverticula - less than 15 mm in depth, in 1 case with a large diverticulum). In these situations, a nasogastric tube was inserted to provide nutrition for up to 3 days. Residual depth after myotomy ranged from 5 to 20 mm (mean 1.0 cm).
results
The duration of the surgical intervention ranged from 30 to 90 minutes (average 54 minutes). No complications were noted during the intervention. During control fluoroscopy with a water-soluble contrast agent, performed one day after the intervention, no cases of extraorgan spread of the contrast agent were recorded (Fig. 3) .
Rice. 3. X-ray examination of the esophagus before surgery: a diverticulum with retention of the contrast agent in it is determined (a); patency is restored, the “delay” of the contrast agent is not determined (b).
In 1 (3.2%) patient, the appearance of subcutaneous emphysema was noted in the postoperative period, but fluoroscopy of the esophagus and stomach did not reveal any leakage of the contrast agent, which was regarded as diffusion of carbon dioxide into the cellular spaces of the neck during the intervention. No other complications were noted in the postoperative period.
From the 1st day after the operation, in the absence of “leakage” of the contrast agent beyond the walls, patients were allowed to take fluids; from the 2nd day of enteral nutrition and by the 3rd day after the operation, the patients were transferred to the general table. When transferred to the general table, the complaints that the patients had before the surgical intervention were absent. Discharge from the hospital occurred on the 4th—5th day after the intervention.
The effectiveness of this method of endoscopic treatment for Zenker's diverticula was monitored in 29 (93.5%) patients for more than 6 months. All patients were examined in the clinic, control esophagography and endoscopic examination were performed. 27 (93.1%) patients resumed normal, full oral nutrition and reported satisfaction with the results of endoscopic surgery.
Fluoroscopy in these patients confirmed unimpeded entry into the esophagus and further passage into the stomach of the contrast agent. Depending on the initial characteristics of the diverticula and the volume of septomyotomy performed, the area of surgical intervention was not differentiated (in 9 patients) or a slight contrast was determined along the contour of the bottom of the diverticulum in the shape of a crescent about 10 mm thick with easy evacuation of the contrast agent from it into the esophagus (in 17 patients).
In 1 case, in an 86-year-old patient with a large diverticulum, surgical intervention was undertaken as the first stage of treatment before endoscopic gastrostomy to relieve dysphagia. However, 3 months after surgery, the patient contacted the clinic with a request to remove the gastrostomy tube due to the beginning of oral intake without difficulty. Fluoroscopy revealed a 6 cm diverticulum with minimal delay (less than 10 s) of contrast agent.
During endoscopic examination performed 6 and 12 months after the intervention, in 27 (93.1%) patients the device was passed unhindered into the stomach. In the area of surgical intervention there was a small depression, the mucous membrane was pink and smooth. Retention of food masses and liquid was not detected.
In 2 (6.9%) cases, more than 1 year after the intervention, a relapse of complaints was noted. Endoscopic examination and fluoroscopy of the esophagus revealed a recurrence of the disease, which required repeated intervention without intra- and postoperative complications.
First successful experience of the Zenker's diverticulum endoscopic therapy in Kazakhstan
Kanat Batyrbekov1, Alexey Zelenyy2, Ainur Galiakbarova1 1 National Research Oncology Center, Nur-Sultan, Kazakhstan; 2 Multi-profile medical center, Nur-Sultan, Kazakhstan Abstract
Zenker's diverticulum tends to occur in the elderly and is generally a relatively rare disorder;
the prevalence of Zenker's diverticulum is 1.5–5% of all esophageal diverticula. Men are affected 2-3 times more frequently than women. To date, Zenker's diverticulum is treated mostly by surgery in Kazakhstan, however, with the development of endoscopy the minimally invasive method, endoscopic diverticuloesophagostomy, is being implemented. The transoral treatment is aimed at creating the common cavity between the esophagus and the diverticulum in order to prevent food accumulation in the diverticulum. The anterior wall between these two structures consists of the diverticular wall, m. сricopharyngeus and esophagus wall, the septum transsection automatically ensures myotomy. Both open surgery and endoscopic transoral treatment of Zenker's diverticulum result in reduced symptoms in 94–100% of patients. The paper reports the first successful experience of the Zenker's diverticulum treatment by endoscopic submucosal tunnel dissection in Kazakhstan. Key words
: Zenker's diverticulum, endoscopic therapy, septicotomy, tunnel dissection, diverticuloesophagostomy.
For citation
: Batyrbekov K., Zelenyy A., Galiakbarova A. First successful experience of the Zenker's diverticulum endoscopic therapy in Kazakhstan. Clinical review for general practice. 2020; 3:45–48. DOI: 10.47407/kr2020.1.3.00023
Discussion
Minimally invasive interventions are increasingly being performed in different groups of patients. The choice of surgical intervention for Zenker's diverticulum remains a subject of debate [3, 13].
Our data indicate the high effectiveness of the endoscopic intervention method for this condition based on an analysis of the results of treatment of 31 patients. The advantages of this intervention include its short duration, low frequency, low incidence of postoperative adverse events (subcutaneous emphysema in 1 patient), and the possibility of starting fluid and food intake on days 1 and 2 of the postoperative period.
Separately, we should dwell on the assessment of the long-term results of the operations performed, which were followed in 93.5%. At the same time, in 93.1% of patients, oral food intake was restored; X-ray and examinations revealed no obstructions in the patency of the contrast agent and endoscope.
Our data indicate the possibility of effective endoscopic correction of large Zenker diverticula, both to improve the quality of life and as an option for two-stage operations, which is especially important in elderly patients. However, one clinical case indicates the need for more observations.