Stomach neurosis (gastroneurosis) is a recurrent psychopathological condition of the digestive organs, manifested by a complex of symptoms of a functional dyspeptic disorder and arising due to a violation of nervous regulation. Gastroneurosis occurs to one degree or another in every fourth adult representative of the human population, but the occurrence and progression of pathology is also possible in children.
Subjectively, gastric neurosis has the same symptoms as other diseases of the gastrointestinal tract, which can make it difficult to make a correct diagnosis and delay treatment. Optimal correction of gastroneurosis at any age includes not only drug treatment, but also auxiliary physiotherapy, diet therapy, spa treatment and psychotherapy (in the case of a burdened neurotic history).
What is gastric neurosis
Gastroneurosis is an inorganic dysfunction of the stomach and the initial parts of the small intestine and, according to pathomorphological criteria, is a somatoform disorder of the autonomic nervous system.
With gastroneurosis, the morphological structure of the organ does not change
The main feature of neurotic gastric dysfunction is the absence of structural and organic changes in the epithelial lining of the stomach. This means that the patient experiences most of the symptoms characteristic of functional dyspeptic stomach disorders (epigastric pain, nausea, loss of appetite, stomach discomfort). Gastric neurosis is also called “pseudo-ulcer syndrome” and “non-ulcer functional dyspepsia.”
The mechanism of development of the pathogenetic reaction in response to stress factors (including physical stress) is usually represented by the following changes:
- Increased tone of the sympathetic nervous system.
- Slowing down parasympathetic transmission.
- Activation of the effects of the paired vagus nerve, which runs from the brain to the abdominal organs and is responsible for the functioning of the organs of the head, neck, chest and peritoneal space.
The main mediator of somatoform gastric dysfunction is stress. In response to the influence of stress factors (both emotional and physical, for example, prolonged fasting), the most important processes necessary to maintain human life are disrupted.
With gastroneurosis, the contractility of the muscles that move partially digested food (chyme) into the intestines for further processing is impaired. The secretion of the main components of gastric juice changes naturally: enzymes, pepsin, hydrochloric acid, etc. This leads to indigestion, retention of the food bolus in the stomach cavity and the emergence of a typical symptom complex of functional dyspepsia of inorganic origin.
Note!
A stress factor itself can provoke monofocal inflammation of the epithelial lining of the stomach, since in response to stress the body increases the synthesis of prostaglandins, mediators of inflammation.
Neurosis concept
Neurosis is a long-term psychogenic disorder that is reversible. The term was introduced into use back in the 18th century. In modern official medicine it is not used: it is replaced by a related concept - neurotic disorder.
The causes of neuroses, like any disorders of mental origin, are not fully understood. But most experts agree that the main role in this is played by a stress factor, some kind of traumatic situation. However, what is more important is not the strength or duration of influence of these factors, but the degree of perception and attitude of a person towards them. That is, the internal state of the individual and character traits play a role. For example, traits such as anxiety, suspiciousness, and sentimentality increase the risk of developing the condition.
The famous Russian performer, Irina Dubtsova, was admitted to a psychiatric clinic named after. Solovyova with this diagnosis. The reason for this was the difficult divorce process between her lover and his ex-wife, who annoyed the singer with threatening calls.
Many world psychologists have wondered about the origin of neurotic disorder. Sigmund Freud believed that illness develops when an internal conflict arises between the id and the superego of a person, that is, between her instincts and morality.
Karen Horney suggested that neurosis is a consequence of the conflict between the defensive reactions of the individual. She develops them under the influence of a traumatic factor, such as humiliation, aggression, etc. As a result of this, a person develops several models of attitude towards society: towards, against and away from people - the need for love, power or independence, respectively.
Another cause of the disorder may be a change in the level of neurotransmitters, which makes the human nervous system more vulnerable, or hormonal changes during puberty or menopause.
Symptoms of the disease include the following:
- lability of the emotional background, frequent mood swings;
- sleep problems – insomnia, waking up early or having difficulty waking up in the morning;
- anxiety and fears;
- panic attacks;
- sentimentality, tearfulness, vulnerability;
- increased irritability;
- decreased performance and cognitive-cognitive functions;
- fixation on the traumatic factor;
- light and sound sensitivity;
- increased or decreased appetite;
- pessimism, despair;
- when taking on any task, you stagnate in one place and don’t move anywhere;
- stuttering;
- physiological symptoms - headaches, dizziness, heart pain, digestive disorders, difficulty breathing, etc.
In a state of neurosis, a person maintains a critical attitude towards the symptoms of the disease. There are no psychotic signs in the form of delusions or hallucinations.
Causes and predisposing factors
Gastric neurosis, that is, inflammation of the gastric mucosa not associated with Helicobacter pylori bacteria, is considered by many experts to be a borderline somatoform disorder that requires complex gastroenterological and psychotherapeutic correction. The disease can occur at any age.
Groups of people most susceptible to gastroneurosis
The maximum risk group includes women, as the most vulnerable category of patients in terms of emotional lability. The second category at risk is children of primary preschool and school age, who often experience stress due to difficulties with social adaptation when entering kindergartens and schools.
Chronic neurotic dysfunctions of the stomach in most cases occur in individuals with various types of psychopathologies. Such patients often experience feelings of irritation, anger, and sudden attacks of aggression.
In children, risk factors include asthenic syndromes, autism, and various neurotic disorders. In infancy, possible manifestations of gastroneurosis can be provoked by the syndrome of traumatic shaking of the child.
Risk factors for the development of gastric neurosis
The following risk factors for the development of gastric neurosis are identified:
- Various neurotic conditions (neuroses) in the anamnesis.
- Severe emotional shock or stress, provoked by a change in the usual conditions of the environment and the team.
- Violation of the conditions of “comfort eating” (watching TV shows, sitting at the computer, using various electronic devices and gadgets, reading books and newspapers while eating).
- Eating immediately after sports or heavy physical work.
- Neurological and other diseases that significantly affect autonomic regulation and the balance of sympathetic and parasympathetic transmission.
- Taking psychoactive, psychotropic, sedative and hypnotic medications without a doctor’s prescription or in a dosage exceeding the maximum permissible dose.
The situation is aggravated if the patient suffers from eating disorders, smokes, or abuses alcohol.
Answers to frequently asked questions that arise for those who are faced with neuroses
Are neuroses inherited?
No, they are not transmitted. Character traits can be transmitted, such as impressionability, anxiety, suspiciousness, and so on, which, under unfavorable circumstances, facilitate the onset of neurosis.
Is it possible to recover from neurosis forever?
Yes, you can.
Could sexual dissatisfaction be the main cause of neurosis?
Yes, it can, but now, as the basis of neurosis, it practically does not occur. The role of sex is extremely overrated when it comes to the emergence of neurotic experiences. This is due to the contribution of Sigmund Freud to the development of the causes and mechanisms of neurosis.
Why is physical exercise useful for neuroses?
It is unlikely that it will be possible to cure neurosis with the help of physical education, but physical activity is very useful as an auxiliary component. Stress hormones (adrenaline, cortisol) are consumed and muscles relax, this will contribute to overall calm. You will seem to be letting off steam.
Does neurosis affect life expectancy?
More likely no than yes. But, if we exclude the fact that those suffering from neurosis take more care of themselves and lead a healthier lifestyle. This just contributes to longer life expectancy.
What will happen if I don’t treat my neurosis?
You won't die or go crazy. But your quality of life may decrease significantly. While remaining physically and mentally healthy, a person suffering from neurosis can fill his life with a huge number of restrictions, anxiety and depression.
What is the worst neurosis?
The one that is running. The longer a person suffers from neurosis, the harder and longer it takes to treat him. If a person fell ill, for example, less than 2 months ago, then 3-4 meetings may be enough for treatment. All other things being equal (age, intelligence, motivation, duration of illness, unfavorable background), panic disorder is the easiest to treat, and OCD is the hardest to treat. Social phobia may not poison life as much as panic attacks, but it is much more difficult to get rid of it completely, especially if it has been present since adolescence.
Is it possible to go crazy from neurosis?
No impossible. Read more
When should you start treating neurosis? When to finish? How long does it take to treat neurosis?
Start treating - the sooner the better. At a minimum, if symptoms become regular over two months, it is better to quickly consult a psychotherapist. When to end is a more difficult question. Let me give you an example of a situation: let’s take a person with a moderate degree of neurosis, who, for example, will need 8 meetings. The first two weeks - twice a week, then - once a week, that is, the general course will last one and a half to two months. Most often, by the fourth session, symptoms subside significantly. Gradually the symptoms go away in waves. After two months, they are either gone, or their echoes remain, which appear less and less often and become less intense. That is, when the symptoms have passed or there has been a persistent absence of them, you can think about ending the treatment. However, it happens that there are no symptoms, but a person continues to visit a psychotherapist for some time in order to optimize the quality of his life, make himself more stress-resistant and thereby prevent the recurrence of neurosis. To summarize: it is optimal to stop treatment when the symptoms have gone away completely or when there are so few of them that they no longer affect life, in addition, the issues that can support neurosis or provoke it have been resolved.
Is it better to treat neurosis in a hospital or on an outpatient basis?
From my point of view, in the vast majority of cases, neurosis is best treated on an outpatient basis. It makes sense to go to a hospital (for example, to a neurosis clinic) only if a person is completely unable to lead a normal life due to constant anxiety and severely depressed mood. Hospitals may prescribe drugs in IVs that will help you come to your senses a little. In a hospital setting, it is easier for a doctor to determine the effectiveness of drugs, since the patient is under constant supervision. In an outpatient setting, the doctor must be much more careful so as not to “overload” the patient. However, it is not always possible to receive full psychotherapeutic treatment in a hospital. However, for some it is a way out to get relief. Another reason to go to the hospital may be an unfavorable environment at home. If you find yourself in a hospital, avoid conversations on the topic of who got sick, otherwise you risk treating some fears and leaving with others. Outpatient treatment is preferable, since getting rid of neurosis requires mastering techniques that need to be practiced in real life. If the need arises, you will be prescribed sedatives anyway. Plus: you will be able to stay in your normal life for several weeks.
Is it possible to cure neurosis without pills?
In most cases, yes, if it is a pure neurosis, uncomplicated by anything (depression, organic brain damage, long-term course, and so on).
Are there pills for neurosis?
No. Drugs (tranquilizers, antidepressants, minor antipsychotics) that are used in the treatment of anxiety disorders are aimed at reducing symptoms, and not at the cause or mechanisms of neurosis.
What's the worst thing about neuroses?
Being a physically and mentally healthy person, you will not use your potential and realize your opportunities, and life will pass you by.
If I have a neurosis, is it worth talking about it, will they understand me?
Unfortunately, most likely you will not find understanding. People who have never experienced panic attacks, fear and anxiety in situations that seem ordinary to them (an airplane, a subway, a hairdresser, a concert hall, performances, standing in a traffic jam) are not able to understand how one can worry so much in completely safe situations and not being able to “pull yourself together.” Therefore, it makes sense to communicate what is happening to you only to those who are actively involved in your life or live nearby. So that they have the opportunity, if not to understand, then at least to accept the limitations that neurosis has brought into your life. So that they understand how they can help you and do not add even more anxiety with their worries, irritation or lectures. At the same time, you should not be afraid that someone will find out about your problems: your behavior may be incomprehensible to others, but since you will still control yourself, no one will decide that you are some kind of abnormal. Neuroses are quite common, so people often find understanding from those whom they would never have thought would find support.
Which specialist is best to treat neurosis?
See a psychotherapist. It was no coincidence that I clarified that I was seeing a doctor, because, unfortunately, psychologists often call themselves psychotherapists. You need a doctor who knows psychotherapeutic methods for treating neuroses. If you want to truly cure neurosis, and not just smooth out the symptoms, then a neurologist or psychiatrist is not suitable.
Can neurosis go away on its own?
Yes maybe. But if the symptoms increase and do not go away for more than one month, then it is unlikely.
Is it necessary to prevent neurosis?
I don’t think it’s necessary to specifically prevent any disease if your heredity is not burdened by this disease - there’s no point in thinking about what doesn’t exist. But it’s worth leading a healthy lifestyle, that’s all! Try not to give a damn about the quality of your life, don’t push yourself, don’t accumulate stress, try to balance your life so that it includes rest, healthy sleep, interesting activities, pleasant communication, and sufficient physical activity. Minimize the amount of conflict, alcohol and do not use drugs. Then the chances of neurosis appearing in your life will be significantly reduced.
Can mental trauma cause neurosis?
Yes maybe. Although often neurosis occurs when a difficult period is over.
Is it necessary to deal with childhood memories in order to recover from neurosis?
Not necessary. Information about childhood is needed to find out the personality traits that contributed to the onset of neurosis, and to determine habitual ways of reacting and thinking. That is, the mechanism “I remembered something from childhood, told a psychotherapist and the neurosis went away” does not work.
Is anorexia nervosa a neurosis?
No, with anorexia nervosa there is a completely different mechanism of occurrence and development. This diagnosis refers to eating disorders and is mechanically close to addiction.
Can alcoholism lead to neurosis and vice versa?
Yes maybe. Often the first panic attack in those suffering from alcoholism occurs during abstinence (the day after abuse). Sometimes after such an attack a person stops drinking. The situation is the opposite, when with the help of alcohol a person suffering from neurosis and social phobia relieves his constriction and fear, and begins to do this regularly.
What type of psychotherapy is most effective for neuroses?
From our point of view, the cognitive behavioral approach is the best. It began to be developed in the mid-20th century. A huge amount of research has been carried out on its effectiveness, techniques have been developed. The approach is based on a scientific basis, and in a short period of time it can help a person change a lot. But this does not mean that it is the only effective one; representatives of other psychotherapeutic schools also provide effective treatment. Here it’s like in surgery: scalpels can be of different shapes, the main thing is literacy, intelligence, experience, surgeon skills and the desire to help.
Read more about the treatment of neuroses
Neurosis of the stomach with irritable bowel syndrome
Gastric neurosis is the main clinical manifestation of IBS (irritable bowel syndrome) - a chronic intestinal disorder in the absence of visible organic causes. This type of intestinal pathology manifests itself as constant pain in various parts of the abdomen, flatulence, rumbling, discomfort, and stool disturbances. Histological examination reveals predominantly dystrophic changes; there is no objective clinical picture of inflammatory processes.
State of the intestines in the presence of the syndrome
The main reasons influencing the development of such symptoms are considered to be psychological and social factors. In 90% of cases, IBS is accompanied by somatoform neurotic digestive dysfunction (in some sources, neurosis of the stomach and intestines and IBS are even used as synonyms).
Objective clinical picture of gastric neurosis
With gastric neurosis, patients usually complain of epigastric pain, nausea, poor digestion of food, and stomach discomfort after eating. It is important that with gastroneurosis, such disorders occur after eating any food, even if it is prepared in compliance with all the principles of dietary sparing recommended for gastroenterological patients.
Gastroneuroses are divided into three groups:
- with a predominance of epigastric and distress syndrome;
- with a predominance of functional dyspeptic syndrome (after eating there is a feeling of fullness, bloating, heaviness, the amount of intestinal gas increases);
- with a predominance of intestinal disorders (constipation, diarrhea, various changes in the consistency, appearance and texture of stool).
In almost 80% of cases, gastric neurosis with a predominance of intestinal disorders manifests itself as constipation, the duration of which can last up to 3-4 days. This category also includes painful straining during bowel movements, imperative (false) urges that do not end with the release of feces, and the appearance of the so-called fragment-like “sheep” feces (hard spherical fecal lumps of dark brown or black color).
Psychotherapeutic techniques and other methods of therapy
Along with the treatment of neuroses with medications, herbal medicine and physiotherapy have proven themselves well.
When developing a therapeutic regimen, it is important to take into account that disorders of this type have “double” symptoms – somatic (physiological) and psychological. Only an experienced neuropathologist, psychiatrist or neurologist can solve mental problems. In some cases, the involvement of acupuncturists and massage therapists is required. To get rid of mental problems, homeopathic treatment is often used, which involves the use of products based on natural raw materials. Moreover, biologically active substances are used in microdoses.
The text was checked by medical experts: Head of the socio-psychological service of the Alkoklinik MC, psychiatrist-narcologist L.A. Serova.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!
Symptoms of gastric neurosis
Typical complaints of patients suffering from gastroneurosis are:
- pain in the epigastric region that occurs after a strong emotional experience or consumption of any foods;
- intestinal disorders;
- increased gas formation, bloating, release of large amounts of intestinal gas with an unpleasant odor, stomach discomfort;
- feeling of incomplete evacuation after defecation;
- nausea.
Neurotic gastric dysfunction is characterized by the appearance of all these symptoms after exposure to stress factors or consumption of food, even if it complies with the norms of healthy and dietary nutrition of patients with gastroenterological pathologies.
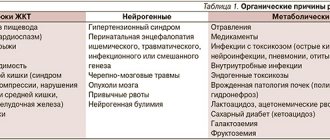
In addition to gastroenterological symptoms, extragastric symptoms (i.e. caused by other disorders) are distinguished. These include autonomic dysfunction, psychopathological condition and other associated syndromes. The table below provides examples of complaints for certain groups of symptoms.
Symptoms of the disease
Symptoms of gastric neurosis are often confused with a disease such as gastritis:
- The desire to eat even if the meal was very recent.
- Colic.
- Pain in the stomach area.
- Heartburn.
- Belching, which is accompanied by an unpleasant odor and sounds.
- Feeling of heaviness.
- Lack of appetite.
- Chewing reflex.
To make a correct diagnosis, you need to pay attention to accompanying symptoms such as:
- Migraine, dizziness, high blood pressure.
- Lack of healthy sleep.
- Arrhythmia.
- Panic attacks.
It is important to note that each of the above symptoms applies not only to gastric neurosis, but also to other diseases. It is necessary to first make a correct diagnosis, and only then begin treatment.
stomach neurosis: causes
Diagnosis of gastric neurosis
To carry out differential diagnosis, a set of measures is carried out. The patient is prescribed ultrasound of the abdominal organs, FGDS, electrogastrography, sonography (if necessary). Laboratory diagnostics include stool testing for occult blood (to exclude gastrointestinal bleeding), general urine and blood tests.
The table below provides a description of the differential diagnosis based on the study of the primary anamnesis.
Treatment of gastric neurosis
Gastroneurosis must be treated comprehensively (unlike infectious gastritis, which requires step-by-step therapy).
Psychotherapy
For neurotic gastric dysfunction, the basic treatment is psychotherapy (and not diet therapy, as with other forms of gastritis and gastroduodenitis). To work through the underlying cause of pseudoulcer syndrome, cognitive-behavioral and psychoanalytic therapy techniques are used.
Against the background of psychocorrection, it is important to ensure a sufficiently restrictive regime that allows you to eliminate as much as possible all sources of possible stress. The patient should take daily walks away from busy streets, highways, and large industrial facilities. It is useful to practice aromatherapy and audiotherapy techniques, and if there are no contraindications, regularly take relaxing baths with chamomile or lavender infusions.
Yoga or Pilates also have a good calming effect.
Drug treatment
Sedatives are used to correct the psycho-emotional state. For mild or moderately expressed disorders, it is preferable to use herbal remedies: valerian tincture and syrup, motherwort, hawthorn tincture, herbal preparations (Tenoten, Persen, Novo-PASSIT).
The standard treatment regimen for uncomplicated gastric neurosis is as follows:
- Anxiolytics and nootropics (“Phenazepam”, “Phenibut”, “Mexidol”, “Adaptol”).
- Antidepressants (Neuroplant, Fluoxetine, Velaxin) to combat depressive disorders, sleep disorders, irritability and anxiety.
- Antispasmodics (drotaverine, papaverine) for pain syndrome.
- Non-steroidal anti-inflammatory drugs (ibuprofen, diclofenac, ketorolac) and analgesics (metamizole sodium) - for severe pain that is poorly controlled by myotropic antispasmodics.
- Prokinetics (“Motilium”, “Motilak”) for nausea and vomiting.
To correct conditions associated with long-term deficiency of essential vitamins and micronutrients, vitamin-mineral complexes are selected (after a biochemical blood test).
Important!
For patients with severe forms of exhaustion and manifestations of anorexia, treatment begins with replacement infusion therapy and parenteral administration of nutritional mixtures.
Physiotherapy
Physiotherapy is a secondary treatment option for non-functional dyspeptic indigestion. Hydrotherapy, as well as procedures using alternating electromagnetic currents, have a good therapeutic effect. In the absence of contraindications, a course of relaxing massage is recommended: it has a positive effect on blood circulation and allows you to restore the motor-evacuation function of the digestive tract.
Diet
Diet for gastroneurosis is used as an auxiliary measure to prevent possible complications and prevent an acute inflammatory process. It is preferable to cook food using reactive, thermal and mechanical gentle methods.
Fried foods, smoked, canned and pickled foods, confectionery, sausages, and alcohol are limited or completely excluded.
Foods prohibited for consumption during gastroneurosis
Gastric neurosis is a serious psychopathological pathology in which the functioning of the autonomic nervous system, which is responsible for the functioning of the stomach and other digestive organs, is disrupted. The basic treatment for gastroneurosis (as opposed to infectious gastritis) is psychotherapy, which, depending on the clinical symptoms, is supplemented with medication, physiotherapeutic methods, and diet therapy. Once a year, sanatorium treatment at balneological resorts is recommended.
Treatment with nootropics
Many patients are shown the so-called. nootropics are drugs that improve microcirculation in the “brain pool” and improve the nutrition of cells of the central nervous system. Some of the most common nootropics are Piracetam and Phenibut. Most nootropics used improve mood and increase vitality. Side effects of these medications may include increased irritability and sleep disturbances. In some cases, these psychogenic disorders are an indication for starting to take weak antipsychotics, which include Eglonil and Sonapax.