Colonization of Helicobacter pylori on the surface and folds of the gastric mucosa significantly complicates antibacterial therapy. A successful treatment regimen is based on a combination of drugs that prevent the emergence of resistance and overtake the bacteria in different parts of the stomach. Therapy must ensure that even a small population of microorganisms does not remain viable.
Helicobacter pylori eradication therapy includes a complex of several drugs. A common mistake that often leads to unpredictable results is replacing even one well-studied drug from a standard regimen with another drug from the same group.
Proton pump inhibitors (PPIs)
PPI therapy has proven effective in various clinical studies. Although PPIs have a direct antibacterial effect on H. pylori in vitro, they do not play an important role in eradicating the infection.
The mechanism by which PPIs synergize when combined with antimicrobials to enhance the clinical efficacy of eradication therapy has not been fully established. It is assumed that antisecretory drugs of the PPI group may help increase the concentration of antimicrobial agents, in particular metronidazole and clarithromycin, in the gastric lumen. PPIs reduce the volume of gastric juice, as a result of which the leaching of antibiotics from the surface of the mucosa decreases, and the concentration, accordingly, increases. In addition, reducing the volume of hydrochloric acid maintains the stability of antimicrobials.
What happens in the body
As soon as Helicobacter enters the human body, it immediately descends into the stomach, where it lives for the rest of the time. In order not to die from gastric juice, the composition of which is quite aggressive, Helicobacter secretes special enzymes that surround it with a shell and neutralize the acid. The spiral-shaped antennae that Helicobacter has allow it to drill through the mucous layer and get to the cells of the parietal tissues, which are usually hidden from acid.
It is the parietal cells of tissues that become the main food for Helicobacter. The pathogenic microorganism eats them and poisons the environment with the products of its vital activity. At the same time, those blood cells that react to Helicobacter and strive to destroy them (neutrophils) wake up in the body. However, by destroying the pathogenic microorganism, neutrophils also destroy mucosal cells that have already been touched by Helicobacter.
After the layer of the mucous membrane is damaged, hydrochloric acid begins to actively affect the tissue. This is how the inflammatory process develops and an ulcer occurs. The localization of ulcers is most often similar. This is explained by the fact that Helicobacter itself is very fond of two parts of the stomach - the bulb and the pylorus.
Bismuth preparations
Bismuth was one of the first drugs to eradicate H. pylori. There is evidence that bismuth has a direct bactericidal effect, although its minimum inhibitory concentration (MIC - the smallest amount of drug that inhibits the growth of a pathogen) against H. pylori is too high. Like other heavy metals such as zinc and nickel, bismuth compounds reduce the activity of the enzyme urease, which is involved in the life cycle of H. pylori. In addition, bismuth preparations have local antimicrobial activity, acting directly on the bacterial cell wall and disrupting its integrity.
MALT lymphoma
MALT lymphoma is an extranodal marginal zone B-cell lymphoma associated with mucous membranes. It is a non-Hodgkin lymphoma, the substrate of which is sufficiently mature malignantly transformed lymphocytes originating from solitary lymphoid follicles of the mucous membranes.
Currently, H. Pylori is considered as the main causative agent of the disease, but the incidence in the world is low and amounts to 1 case per 30,000-80,000 infected individuals.
Metronidazole
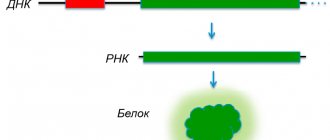
H. pylori is generally very sensitive to metronidazole, the effectiveness of which is independent of pH. After oral or infusion use, high concentrations of the drug are achieved in the gastric juice, which makes it possible to achieve the maximum therapeutic effect. Metronidazole is a prodrug that undergoes activation by bacterial nitroreductase during metabolism. Metronidazole causes H. pylori to lose its helical DNA structure, causing DNA damage and killing the bacterium.
NB!
The result of treatment is considered positive if the results of the test for H. pylori, carried out no earlier than 4 weeks after the course of treatment, are negative. Performing the test before 4 weeks after eradication therapy significantly increases the risk of false negative results. It is preferable to stop taking PPIs two weeks before diagnosis. Helicobacter pylori eradication therapy: scheme
First line eradication of Helicobacter pylori
The first-line three-drug regimen gets its name because it consists of three drugs:
- antibiotic Clarithromycin,
- antibiotic Amoxicillin,
- a proton pump inhibitor based on Omeprazole, which regulates the activity of the acidic environment of gastric juice.
Proton pump inhibitors make it possible to get rid of many negative manifestations of ulcers and gastritis caused by increased acidity of the stomach, as well as to avoid overly strict restrictions imposed on the diet of a patient with peptic ulcer disease. However, restrictions still remain, although not as strict.
It is possible to replace Amoxicillin with the antibiotic Nifuratel or Metronidazole. According to indications, the gastroenterologist can prescribe a drug based on bismuth derivatives in regimen 4. Normally, such drugs are included in the second-line eradication regimen, but their properties have a positive effect on the course of the process of stopping the inflammatory process. A protective coating is formed on the surface of the stomach, relieving symptoms of inflammation and pain.
Lightweight scheme for elderly patients:
- Antibiotic Amoxicillin;
- Proton pump inhibitor;
- Bismuth preparation.
To increase the effectiveness of standard first-line therapy, it is proposed to double the period of its use - from 7 to 14 days. Expected efficiency is up to 95%. If treatment is ineffective, the doctor recommends switching to a second line of eradication therapy.
Clarithromycin
Clarithromycin, a 14-member macrolide, is a derivative of erythromycin with a similar spectrum of activity and indications for use. However, unlike erythromycin, it is more acid resistant and has a longer half-life. The results of studies showing that the triple eradication therapy regimen for Helicobacter pylori using clarithromycin gives a positive result in 90% of cases, led to the widespread use of the antibiotic.
In this regard, an increase in the prevalence of clarithromycin-resistant strains of H. pylori has been recorded in recent years. There is no evidence that increasing the dose of clarithromycin will overcome the problem of antibiotic resistance to the drug.
Selection of drugs if a repeat course of eradication therapy is necessary
And the first, and second, and even third regimen of Helicobacter pylori therapy may be ineffective when the eradication rate is 80% or less of cases of achieving the target treatment goal. The effectiveness of treatment is reduced due to bacterial resistance to antibiotics, so researchers of the problem continue to search for better regimens.
There is no concern about Helicobacter pylori resistance to Amoxicillin (less than 1%), to Tetracycline (close to 0).
Number of bacterial strains resistant to other antibacterial drugs:
- To Clarithromycin - in Europe from 9.9 to 18%, in Moscow - 19.3% in adults, 28.5% in children;
- To Metronidazole - in Europe from 20 to 40%, in Moscow - 54.8% in adults, 23.8% in children
This is explained by the frequent prescription of macrolide antibiotics in pediatric and therapeutic practice. Of no small importance in the success of eradication therapy are proton pump inhibitors, which create a favorable environment in the gastrointestinal tract for the use of antibiotics. With the low quality of drugs in this group, the effectiveness of antibacterial agents also decreases.
Research is being conducted on adding a probiotic to standard therapy to reduce stool frequency and flatulence.
A new scheme for eradicating the bacterium has emerged - sequential therapy, taking 10 days. It is used when the first line scheme fails.
In the first 5 days take:
- Proton pump inhibitor – 2 times a day;
- Amoxicillin – 2000 mg/day.
In the next 5 days:
- Proton pump inhibitor – 2 times a day;
- Clarithromycin – 1000 mg/day;
- Tinidazole – 1000 mg/day.
According to the study, even in patients infected with Helicobacter pylori with high resistance to Clarithromycin, eradication increased from 29% to 89%. In the remaining patients with unsuccessful first-line eradication, the rate increased from 78% to 91%.
Indications for eradication therapy
According to the Maastricht 2-2000 Consensus Report, H. pylori eradication is strongly recommended:
- all patients with peptic ulcer disease;
- patients with poorly differentiated MALT lymphoma;
- persons with atrophic gastritis;
- after resection for gastric cancer;
- first-degree relatives of patients with stomach cancer.
The need for eradication therapy in patients with functional dyspepsia, GERD, as well as in persons taking non-steroidal anti-inflammatory drugs for a long time remains a subject of debate. There is no evidence that eradication of H. pylori in such patients affects the course of the disease. However, it is well known that individuals with H. pylori who have nonulcer dyspepsia and corpus-predominant gastritis are at increased risk of developing gastric adenocarcinoma. Thus, H. pylori eradication should also be recommended for patients with nonulcer dyspepsia, especially if histology reveals corpus-predominant gastritis.
The argument against anti-Helicobacter therapy in patients taking NSAIDs is that the body protects the gastric mucosa from the damaging effects of drugs by increasing cyclooxygenase activity and prostaglandin synthesis, while PPIs reduce natural defenses. However, eradication of H. pylori before prescribing NSAIDs significantly reduces the risk of peptic ulcer disease during subsequent treatment (a study by American scientists led by Francis K. Chan, published in The Lancet in 1997).
What is the Helicobacter bacterium?
Helicobacter is a special type of pathogenic microorganism. It is a dangerous bacterium that infects the duodenum and stomach of humans. The microorganism itself is a parasite that produces toxic substances that damage the mucous membranes of organs. It is damage to the mucous membrane that leads to peptic ulcers, gastritis and other dangerous ailments.
It has long been believed that no organism is able to survive in the acidic environment of the stomach. But this does not apply to Helicobacter. The bacterium, on the contrary, thrives in an acidic environment, which is preferable for it to any other habitat. Helicobacter pylori has a spiral shape and flagella. This structure of the microorganism allows it to move through the mucous membranes of internal organs and cause irreparable harm to their integrity.
Helicobacter can adapt to almost any habitat. This is explained by the fact that this organism practically does not require oxygen. And another distinctive feature of Helicobacter pylori is its ability to change its own shape and become oval or round.
Russian scientists have come to the decision to introduce a special term - helicobacteriosis. It denotes all the processes that begin to occur in the body immediately after the introduction of this pathogenic microorganism into it. But Western scientists conducted studies of patients’ charts and came to the conclusion that about 60-65% of the population of the entire Earth are susceptible to infection. Thus, Helicobacter is the most common infectious disease of humanity after herpes, which is a viral disease.
Eradication therapy
Despite the use of combination treatment regimens, 10–20% of patients infected with H. pylori fail to achieve elimination of the pathogen. The best strategy is to select the most effective treatment regimen, but the possibility of using two or even more sequential regimens should not be ruled out if the treatment of choice is insufficiently effective.
If the first attempt at eradication of H. pylori fails, it is recommended to immediately proceed to second-line therapy. Antibiotic sensitivity testing and switching to salvage therapy regimens are indicated only for those patients in whom second-line therapy will also not lead to eradication of the pathogen.
One of the most effective “rescue regimens” is a combination of PPI, rifabutin and amoxicillin (or levofloxacin 500 mg) for 7 days. An Italian study led by Fabrizio Perri and published in Alimentary Pharmacology & Therapeutics in 2000 confirmed that the rifabutin regimen was effective against strains of H. pylori resistant to clarithromycin or metronidazole. However, the high price of rifabutin limits its widespread use.
NB! To avoid the development of resistance to both metronidazole and clarithromycin, these drugs are never combined in the same regimen. The effectiveness of such a combination is very high, but patients who do not respond to therapy usually develop resistance to both drugs at once (a study by German scientists led by Ulrich Peitz, published in Alimentary Pharmacology & Therapeutics in 2002). And further selection of therapy causes serious difficulties.
Research data confirm that a 10-day salvage therapy regimen, including rabeprazole, amoxicillin and levofloxacin, is much more effective than standard second-line eradication therapy (a study by Italian scientists led by Enrico C Nista, published in Alimentary Pharmacology & Therapeutics in 2003 year).
RECOMMENDATIONS FOR TREATMENT OF HELICOBACTER PYLORI INFECTION
The paper discusses H. pylori eradication more specifically. Based on her own findings and the International Consensus Committee's recommendations for treating H. pylori infection, the author provides guidelines for the practitioners. The paper underlines the need for applying a uniform approach to the diagnosis and treatment of H. pylori infection.
T.L. Lapina – assistant course “Functional diagnostics and pharmacotherapy in gastroenterology”, Department of Family Medicine, Faculty of Postgraduate Professional Education
MMA im. THEM. Sechenov
TLLapina, Assistant, Course “Functional Diagnosis and Pharmacotherapy in Gastroenterology”, Department of Family Medicine, Faculty of Postgraduate Training IM Sechenov Moscow Medical Academy
WITH
1983, when a new type of microorganism, Helicobacter pylori (H. pylori), was first isolated in culture; numerous studies have proven its pathogenetic significance (Table 1).
The study of H. pylori is carried out using the latest scientific methods and is moving forward with enormous strides. Such a “rapid” accumulation of theoretical knowledge in this area, unfortunately, leads to some lag in the popularization of this information among practitioners. As a result, this results in errors in diagnosis, and most importantly, in the choice of treatment for H. pylori infection. Unfortunately, most of the literary sources that methodically correctly describe the practice of eradication therapy, i.e. therapy aimed at destroying H. pylori are available in English; only a few works have been published in Russian so far. Perhaps the first document aimed at “legitimizing” and unifying the treatment of H. pylori infection was adopted in February 1994 by a special conference of the US National Institutes of Health [1]. At the conference, a consensus was reached on the problem of “Helicobacter pylori and peptic ulcer disease”: patients with peptic ulcer disease with H. pylori infection must be treated with antimicrobial agents both during exacerbation of the disease and during remission, and certain treatment regimens were recommended. However, after 2 years, these recommendations became outdated, as data appeared on more effective combinations of drugs for the eradication of H. pylori. In several European countries, similar documents were independently developed, but the need for a unified approach to the diagnosis and treatment of H. pylori, based on the experience of the best European researchers, led to the convening of a special conference in Maastricht in February 1996. The conference, organized by the European H. pylori Study Group, brought together academic experts in the field, medical practitioners and representatives of National Gastroenterological Societies. After serious discussion, recommendations for the treatment of H. pylori infection were adopted that meet modern requirements [2]. The Maastricht Consensus provides guidance to practicing physicians in European countries and provides answers to questions about H. pylori that may arise in their daily activities and management of gastroenterological patients. Table 1. H. pylori and human pathology
| Pathological conditions | Association with H. Pylori |
| Chronic gastritis caused by H. pylori infection Peptic ulcer of the stomach and duodenum Gastric cancer MALT lymphoma | Installed |
| Non-ulcer dyspepsia Ménétrier's disease Coronary heart disease Child growth retardation | Likely |
| Gastroesophagojejunal reflux disease Gastroduodenal ulcerations associated with nonsteroidal anti-inflammatory drugs | Sporna |
“Recommendations for the diagnosis and treatment of Helicobacter pylori infection in adults with gastric and duodenal ulcers,” developed by the Russian group for the study of H. pylori, were discussed at a scientific conference dedicated to the 100th anniversary of the birth of V.Kh. Vasilenko in April 1997 and at the III National Gastroenterological Week in November 1997. They were published in the Russian Journal of Gastroenterology, Hepatology, Coloproctology [3] and with the help of the Russian Gastroenterological Association (RGA) were distributed to various regions of Russia. The recommendations are extremely specific and are designed to help practicing doctors and health care managers. Table 2. Indications for treatment of H. pylori infection
| Indications | Degree of scientific evidence | |
| Russian gastroenterological Russian group association on the study of H. pylori, April 1997 | European H. pylori Study Group Maastricht, September 1996 | |
| Peptic ulcer of the stomach and duodenum in the acute stage and in remission | Necessarily | |
| peptic ulcer | unconditional | |
| MALtomoma of the stomach | unconditional | |
| gastritis | probable | |
| after gastric resection surgery for cancer | probable | |
| Preferably | ||
| functional dyspepsia | possible | |
| heredity burdened by stomach cancer, | possible | |
| long-term use of proton pump inhibitors for gastroesophagojejunal reflux disease | probable | |
| therapy with non-steroidal anti-inflammatory drugs | possible | |
| after surgery for peptic ulcer | probable | |
| patient's wish | probable | |
| Maybe | ||
| to prevent stomach cancer | possible | |
| asymptomatic carriers | possible | |
| extra-nutritive diseases (coronary heart disease, growth retardation in children) | possible | |
Of fundamental importance for practice is the separation of methods for diagnosing H. pylori before treatment (primary diagnosis - detection of infection to justify treatment) and after eradication therapy (diagnosis of eradication - monitoring the success of the antibacterial regimen). The fact is that H. pylori is found in 100% of cases with chronic gastritis, gastric and duodenal ulcers. Therefore, in order to begin anti-Helicobacter therapy, it is enough to confirm the presence of the bacterium using one of the available methods (of course, subject to the rules for performing these methods and proper sterilization of endoscopic equipment). These methods are listed in the “Recommendations”: 1. Bacteriological: culture of a biopsy of the gastric mucosa on a differential diagnostic medium. 2. Morphological: – histological “gold standard” for diagnosing H. pylori: staining of the bacterium in histological preparations of the gastric mucosa according to Giemsa, toluidine blue, Warthin-Starry, Ghent; – cytological: staining of bacteria in biopsy smears of the gastric mucosa according to Giemsa, Gram. 3. Respiratory: determination of 14C or 13C isotopes in the patient’s exhaled air, which are released as a result of the breakdown of labeled urea in the patient’s stomach under the action of urease from the bacterium H. pylori. 4. Urease: determination of urease activity in a biopsy of the gastric mucosa by placing it in a liquid or gel-like medium containing a substrate, buffer and indicator. Table 3. Triple therapy based on bismuth preparations
| Bismuth preparation | Antibacterial drugs | |||
| Colloidal bismuth subcitrate or bismuth subsalicylate or bismuth gallate 120 mg 4 times a day (in terms of vimut oxide) | + | Tetracycline 500 mg 4 times a day | + | Metronidazole 250 mg 4 times a day or tinidazole 250 mg 4 times a day |
| Duration of treatment – 7 days | ||||
The “Recommendations” define the concept of “eradication” - this is the complete destruction of the bacterium H. pylori (both vegetative and coccoid forms) in the human stomach and duodenum. Eradication therapy is a serious task for a doctor, and does not always lead to success. For leading research centers, eradication of H. pylori in 80% of cases is an excellent indicator of the effectiveness of therapy.
Table 4. Bismuth salts inhibit H. pylori in vitro
| Bismuth salt | MIC 90 , ng/l |
| Bismuth subcitrate | 4 – 32 |
| Bismuth subsalicylate | 64 |
| Ranitidine bismuth citrate | 16 |
| Bismuth subgallate | 32 |
| Bismuth subnitrate | > 128 |
The use of antibacterial drugs sharply reduces the number of H. pylori in the gastroduodenal mucosa. Therefore, immediately after the end of eradication treatment, even if it fails, H. pylori is not detected. False-negative results are due to the fact that H. pylori may be absent in randomly taken single biopsies of the mucous membrane or may be present there in such small quantities that they are not perceived by diagnostic methods (morphological, urease). A decrease in the number of H. pylori is associated with difficulties in detecting it after monotherapy with bismuth-containing drugs, metronidazole, and any antibacterial drugs used for other indications (for example, augmentin for tonsillitis, furadonin for cystitis, etc.). Table 5. Triple therapy based on parietal cell proton pump inhibitors
| Proton pump inhibitors Antibacterial drugs | ||
| Omeprazole 20 mg 2 times a day | + | Clarithromycin 250 mg 2 times a day + metronidazole 400 mg 3 times a day |
| Or | or | |
| pantoprazole 40 mg 2 times a day | amoxicillin 1000 mg 2 times a day + clarithromycin 500 mg 2 times a day | |
| Or | or | |
| Lansoprazole 30 mg 2 times a day | Amoxicillin 500 mg 3 times a day + metronidazole 400 mg 3 times a day | |
| Duration of treatment – 7 days | ||
Table 6 .
Quad therapy
| Proton pump blockers | Bismuth preparation | Antibacterial drugs | ||
| Omeprazole 20 mg 2 times a day | Colloidal bismuth subcitrate | Tetracycline 500 mg 4 times a day | ||
| or | Or | + | ||
| Pantoprazole 40 mg 2 times a day | Bismuth subsalicylate | Metronidazole 250 mg 4 times a day | ||
| or | or | or | ||
| Lansoprazole 30 mg 2 times a day | Bismuth gallate 120 mg 4 times a day | Tinidazole 250 4 times a day | ||
| Duration of treatment – 7 days | ||||
It is important to note that the use of any proton pump inhibitors (omeprazole, pantoprazole, lansoprazole), due to the adaptation of H. pylori to certain pH values, leads to the redistribution of H. pylori throughout the mucous membrane: bacteria are eliminated from the antrum and are found in greater numbers in the body of the stomach . It is believed that powerful antisecretory therapy also leads to a decrease in the total number of H. pylori bacteria. Thus, if a test for H. pylori is carried out during or immediately after a course of therapy with proton pump inhibitors, a false negative result cannot be excluded, especially if we limit ourselves to biopsy samples from the antrum [4]. There is a known fact of false-negative diagnosis of H. pylori after treatment with omeprazole and using a breath test, which does not require a biopsy. Table 7. Therapy based on ranitidine bismuth citrate
| Ranitidine bismuth citrate 400 mg 2 times a day | Ranitidine bismuth citrate 400 mg 2 times a day | Ranitidine bismuth citrate 400 mg 2 times a day |
| + | + | + |
| tetracycline 500 mg 4 times a day | Clarithromycin 500 mg 2 times a day | Clarithromycin 250 mg 2 times a day |
| + | + | |
| Metronidazole 250 mg 4 times a day | Metronidazole 500 mg 2 times a day | |
| 14 days | 14 days | 7 days |
Table 8. Principles of therapy for H. pylori infection
| • The use of multicomponent treatment regimens - triple therapy - quadruple therapy • Strict adherence to the chosen treatment regimen - certain drugs - certain doses - a certain duration of therapy • Taking into account the synergy of drugs |
Therefore, monitoring the success of antibacterial treatment requires a special approach. The rules for diagnosing eradication according to the “Recommendations” are as follows: 1. Diagnosis of eradication should be carried out no earlier than 4–6 weeks after the end of the course of anti-Helicobacter therapy, or treatment with any antibiotics or antisecretory drugs for concomitant diseases. 2. Diagnosis of eradication is carried out by at least two of the indicated diagnostic methods, and when using methods for direct detection of bacteria in a biopsy of the gastric mucosa (bacteriological, morphological, urease), it is necessary to study 2 biopsies from the body of the stomach and 1 biopsy from the antrum. 3. The cytological method is not applicable to establish eradication. A special place in the diagnosis of H. pylori infection has an enzyme-linked immunosorbent assay and rapid tests based on immunoprecipitation, which make it possible to detect antibodies to H. pylori in the blood serum or capillary blood of patients. These methods can be used as screening methods or, in cases of established disease, for the initial diagnosis of H. pylori infection. It is clear that serological methods are not applicable to detect H. pylori after treatment, since even after eradication of the bacteria, anti-Helicobacter antibodies continue to circulate in the blood. “Recommendations for the diagnosis and treatment of Helicobacter pylori infection in adults with gastric and duodenal ulcers” establish as an indication for eradication treatment only peptic ulcers, both in the acute and remission stages. The significance of H. pylori in human pathology is much broader, although the results of eradication therapy are indeed better studied for this disease. The Maastricht recommendations cover a much wider range of indications for anti-Helicobacter treatment, and indicate the degree of importance of such treatment and its scientific validity (Table 2). It is likely that as new information accumulates, the indications for eradication therapy in the Russian recommendations will be expanded. Features of therapy for H. pylori infection are reflected in certain treatment principles, which are formulated in the “Recommendations” as follows: The basis of treatment is the use of combination (three-component) therapy: • capable of destroying the H. pylori bacterium in at least 80% of cases; • not causing forced withdrawal of therapy by the doctor due to side effects (acceptable in less than 5% of cases) or the patient stopping taking medications according to the regimen recommended by the doctor; • effective for a course duration of no more than 7 – 14 days. Indeed, the most effective eradication therapy regimens are three-component. Unfortunately, treatment with two drugs is not sufficient to eradicate H. pylori in at least 80% of treated patients. The combination of de-nol with metronidazole has not been used in clinical practice for a long time; eradication using such a regimen is practically unattainable. Research 1995 – 1996 showed that the combination of omeprazole with one antibiotic gives too much variation in the results of H. pylori eradication. Thus, dual therapy with omeprazole and amoxicillin is effective, according to various authors, in 29–92% of cases. On average, the effectiveness of dual therapy is estimated at 50–70%. Eradication in controlled studies occurs in less than 80% of those treated, and a dual treatment regimen cannot be recommended for practical healthcare. Thus, eradication schemes have become three-component and even four-component. Eradication therapy is antibiotic therapy, so there are natural requirements for the safety and good tolerability of such treatment. Unfortunately, a shortened course of less than 7 days usually leads to failure - eradication does not occur. Therefore, if an attempt at eradication therapy led to side effects that forced the interruption of the course (for example, an allergic reaction), we can confidently speak about the persistence of H. pylori infection. Recommended regimens for eradication of H. pylori are given in Table. 3, , , . Treatment regimens based on bismuth preparations, primarily colloidal bismuth subcitrate, were first used for H. pylori infection. Bismuth preparations in combination with tetracycline and metronidazole are even called classic triple therapy. The fact is that bismuth salts have bactericidal properties against H. pylori: they destroy the bacterial wall, inhibit bacterial enzymes (urease, catalase, lipase/phospholipase), and prevent the adhesion of H. pylori to the epithelial cells of the stomach. For bismuth salts, the minimum concentrations that inhibit H. pylori (MIC) were determined (Table 4). Currently, a triple therapy regimen with a proton pump inhibitor is considered optimal (Table 5). Due to their properties, proton pump inhibitors are indispensable in anti-Helicobacter treatment. In the early 90s, a number of authors showed that monotherapy with omeprazole leads to the suppression of H. pylori (when examining antral biopsies immediately after a course of antisecretory therapy with a proton pump inhibitor, the bacterium was often not detected). As has already been described, the use of omeprazole leads to a redistribution of the microorganism in the gastric mucosa: their number in the antrum decreases, often significantly, and increases in the body of the stomach. The mechanism of this regulatory effect of proton pump inhibitors is associated with a powerful inhibition of gastric secretion. The synthesis of ATP by H. pylori is carried out due to the presence of an electrochemical gradient of hydrogen ions. Bacterial urease, decomposing urea with the release of ammonium ions, leads to alkalization of the microenvironment of the bacterium, protecting it from the action of hydrochloric acid of gastric juice; under these conditions, ATP synthesis continues. But the use of proton pump inhibitors leads to an increase in pH, and the effect of urease leads to a total increase in pH, to a level that is incompatible with the life of the microorganism. Thus, H. pylori is tolerant to acidic pH values (due to its unique urease activity), but is a “neutrophil” unstable to the alkaline reaction of the environment. When using proton pump inhibitors, bacteria have to move to parts of the stomach with lower pH values, i.e., into the body of the stomach from the antrum. The most powerful antisecretory drugs known today—proton pump inhibitors—not only inhibit H. pylori in the antrum, but also stimulate the host’s defense mechanisms against the bacterium. Antibodies to H. pylori, secreted onto the surface of the gastric mucosa, are quickly degraded under the influence of proteolytic enzymes of gastric juice. A shift in pH to the alkaline side when using H+, K+-ATPase blockers significantly reduces the proteolytic activity of gastric contents and lengthens the half-life of antibodies and their concentration. The functional activity of neutrophils also depends on pH and increases when it shifts to the alkaline side. Proton pump inhibitors have synergism with antibacterial drugs. The activity of many antibiotics increases when pH values shift from acidic to alkaline. In addition, a decrease in secretion volume increases the concentration of antibacterial drugs in gastric juice [4]. However, the anti-Helicobacter effect of proton pump inhibitors is explained not only by suppression of secretion. These drugs have a specific ability, unique to this class of drugs, to suppress H. pylori in vitro and, probably, in vivo. There is evidence that they inhibit bacterial urease and one of its ATPases. Suppression of the urease activity of a microorganism has recently been shown not only in vitro, but also in clinical experiments. All benzimidazole derivatives - omeprazole, pantoprazole, lansoprazole - lead to the same redistribution of bacteria in the gastric mucosa and have a similar bacteriostatic effect (the minimum inhibitory concentrations of each of these drugs are known). Thus, the anti-Helicobacter effect is a property of proton pump inhibitors as a class of drugs. Quadruple therapy should be considered as a reserve therapy. Its effectiveness against H. pylori is assessed as maximum (Table 6). It is advisable to use a combination of four drugs as a “second-line” treatment, after the failure of the first eradication course, or in special cases (for example, in the treatment of gastric MALToma.) The new formula - ranitidine-bismuth-citrate - is a compound that combines the medicinal activity of an antisecretory agent and bactericidal properties of bismuth. The effect of this combination drug exceeds the total capabilities of combining a histamine H2 receptor blocker and bismuth salt, due to the special synergism inherent in this chemical structure. The special properties of ranitidine-bismuth citrate make it possible to combine it with only one antibiotic - clarithromycin, although in fact this combination is already three-component (Table 7). The development of H. pylori resistance to antibiotics significantly reduces the success of eradication therapy. The most common resistance of the microorganism is to metronidazole, although strains of H. pylori resistant to clarithromycin and amoxicillin have been described. Resistance, as a rule, occurs due to uncontrolled, illiterate prescription of an antibacterial agent. Unfortunately, the situation with metronidazole in Russia can be described in exactly this way. According to L.V. Kudryavtseva, reported at the III Russian Gastroenterological Week (1997), primary resistance of H. pylori to metronidazole is detected in 30% of cases; with a repeated course of metronidazole, the bacterium is resistant to it in almost 100% of cases. The most serious and most common mistake in prescribing antibacterial drugs for peptic ulcer disease is the use of metronidazole not as part of the described regimens, but as an additional drug together with histamine H2 receptor blockers, de-nol, or as monotherapy. The reparative properties of metronidazole, if they exist, are so weak that when using modern inhibitors of histamine H2 receptors or proton pumps, which lead to ulcer healing in 2 weeks, it is simply pointless to rely on them. But resistance of H. pylori to metronidazole inevitably arises in case of its unreasonable use. It is in connection with the problem of resistance that the “Recommendations” highlight the rules for the use of anti-Helicobacter therapy: 1. If the use of a treatment regimen does not lead to eradication, it should not be repeated. 2. If the regimen used did not lead to eradication, this means that the bacterium has acquired resistance to one of the components of the treatment regimen (nitroimidazole derivatives, macrolides). 3. If the use of one and then another treatment regimen does not lead to eradication, then the sensitivity of the H. pylori strain to the entire range of antibiotics used should be determined. 4. The appearance of bacteria in the patient’s body a year after treatment should be regarded as a relapse of the infection, and not a reinfection*. If the infection recurs, it is necessary to use a more effective treatment regimen. A common mistake is to reduce the dose of antibacterial drugs or the duration of treatment, or arbitrarily replace components of the regimen. Even replacing tetracycline with doxycycline leads to a decrease in the effectiveness of treatment; replacing clarithromycin with erythromycin practically negates the doctor’s efforts to eradicate H. pylori infection. In most cases, replacing proton pump inhibitors with histamine H2 receptor antagonists is inadequate (Table 8). Unfortunately, there is even a “step-by-step” prescription of the components of the regimen: first a week of omeprazole with metronidazole, and then a week of taking clarithromycin. The result is the same - eradication does not occur, the patient takes antibiotics without any sense, the number of resistant strains of H. pylori increases. Thus, only strict adherence to established treatment regimens (type of drugs, their combination, dose and duration of treatment) makes it possible to achieve eradication of H. pylori in most patients.
Literature:
1. NIH consensus development panel on Helicobacter pylori in peptic ulcer disease. JAMA 1994; 272:65–9. 2. Current European concepts in the management of Helicobacter pylori infection. The Maastricht Consensus Report. Gut 1997; 41(1):8–13. 3. Recommendations for the diagnosis and treatment of Helicobacter pylori infection in adults with gastric and duodenal ulcers. // Russian Journal of Gastroenterology, Hepatology, Coloproctology, 1998; No. 1. 4. Hunt RH The role of acid suppression in the treatment of H. pylori infection. In: Helicobacter pylori. Basic mechanisms to clinical cure. Ed. by RH Hunt, GNJ Tytgat. Kluwer academic publishers. Dordrecht, Boston, London, 1995; 584–93.
Diagnosis of helicobacteriosis
Diagnosis of helicobacteriosis involves a comprehensive assessment of the state of the gastrointestinal tract. The following examination methods are considered the most effective:
- Determination of antibodies to a pathogen in the blood through enzyme-linked immunosorbent assay. If the antibody concentration is higher than 1.1 units/ml, the test is considered positive. At a concentration of 0.9 to 1.1 units/ml, the result is defined as doubtful, which does not exclude the development of helicobacteriosis.
- Esophagogastroduodenoscopy. This is an invasive method that allows you to determine the condition of the epithelium. With pathology, the mucous membranes of the gastrointestinal tract are swollen and hyperemic. An additional endoscopic biopsy is also performed, during which a small fragment of the mucosa is taken for further histological examination.
- Breath test. Prescribed to determine the presence of microorganisms and to monitor treatment. The procedure is simple and non-traumatic. The test is highly informative. It is used to determine whether there are waste products of Helicobacter in the air exhaled by the patient.
- Additional research. A general blood test during exacerbation of helicobacteriosis shows an increase in ESR, a decreased value of hemoglobin and red blood cells, as well as macrocytosis. It is also possible to carry out bacteriological research by cultivating the material on special nutrient media.
Methods of infection
There are several main routes of infection:
- contact-household. Poorly washed cutlery and dishes, personal hygiene items, and towels are indirect carriers of the disease. The bacterium is relatively resistant to the environment: when boiled, it dies almost immediately, when exposed to chemicals - after a couple of minutes.
- oral-fecal. You can become infected through contact with food or contaminated water.