My stomach is rumbling... Well, for now it’s just my intestines making unpleasant sounds and not hurting! Through these 12-13 meters - this is the length of the intestines in an adult - food, medicines, and water pass through. The balance is disrupted, inflammation and diarrhea begin, and life becomes sad!
Don’t think that intestinal inflammation is shameful or disgusting. This part of our body is no different from the ears, noses and eyes. But its value is great! Therefore, symptoms of an inflammatory process have arisen in any part of the intestine - put your feet up and go to an appointment with a gastroenterologist! What are the main symptoms of intestinal inflammation and what treatment is needed?
Intestines - a little human anatomy
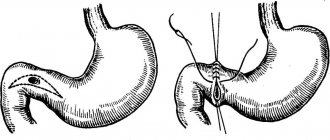
The intestine consists of: large and small sections and duodenum
The intestine is a composite name for several sections of the gastrointestinal tract. It consists of the large, small intestine and duodenum. Each section has its own subspecies. The task of the intestines is to break down incoming food and other substances to the smallest elements.
This happens thanks to digestive enzymes. Intestinal diseases negatively affect the condition of the entire human body and do not depend on age or gender. Intestinal inflammation is also a collective concept. The location of the pathological process directly affects the diagnosis, symptoms and treatment of the patient.
Evaluation of therapy effectiveness
After therapy, re-diagnosis is required. For this, the same MRI method is used, since it is completely safe with frequent use. Scanning requires special equipment, which is not available in every public clinic. To find the nearest tomography center, use the site filters. Enter the name of the service, study the list of medical institutions, compare prices, choose the best offer and sign up for a study through the portal with a discount from the service.
Causes of the inflammatory process in the intestines
The gastrointestinal tract system is very vulnerable. All reasons contributing to pathological processes in the intestines can be divided into the following groups:
- Bacterial infection - damage by various microorganisms - E. coli, salmonella, shigella, viruses, protozoa.
- Helminthic infestation - pinworms, roundworms, bovine or pork tapeworm and others.
- Autoimmune diseases - the body begins to perceive itself as an enemy. The immune system tries to cope with the problem that has arisen, that is, it tries to protect the person from himself.
- The hereditary factor is a variety of genetic pathologies that are transmitted from parents to children.
- Violation of the regime and quality of nutrition is the abuse of fatty, heavy, fried foods, hot and hot spices, low-quality products, alcohol, and cigarettes. Even banal overeating can cause an inflammatory process in any part of the intestine.
- Poor circulation in the intestinal vessels.
- Changes in microflora - occurs when opportunistic organisms begin to prevail over the beneficial inhabitants of the intestines.
The essence of the inflammatory process in the gastrointestinal tract is a violation of the mucous membrane and, as a result, a violation of the absorption of nutrients in this area.
Disease prevention
Preventing irritable bowel syndrome is much easier and cheaper than treating it. Reconsider your lifestyle. Reduce the consumption of fatty, fried, smoked, spicy foods to a minimum, stop smoking and frequent alcohol consumption. Try to have breakfast, lunch and dinner at the same time, avoid snacking on the go. Follow a daily routine. Don't neglect physical activity, including walking and abdominal exercises. Positive attitudes will help reduce the level of anxiety; in difficult cases, consultations with a psychologist or psychotherapist.
Classification of inflammatory processes in the intestines
All gastrointestinal diseases are directly related to the location and duration of the process. Classification based on location:
- Duodenitis - an inflammatory process that occurs in the duodenum - the beginning of the small intestine
- Enteritis - the small intestine is captured in a limited area or for the entire duration
- Colitis – the inflammatory process involves the large intestine along its entire length
According to the duration of the process there are:
- Acute inflammation – lasts no more than 4 weeks
- Chronic – 4 weeks or more
Due to illness:
Diagnostic measures
If unpleasant symptoms appear, you should contact a therapist or gastroenterologist, who will conduct an initial history taking, examination and interview of the patient. If necessary, other highly specialized specialists will be involved in the examination: neurologists, oncologists, surgeons, gynecologists or infectious disease specialists. At the primary stage, laboratory test data is collected and assessed. The presence or absence of inflammatory processes, parasitic lesions, and pathogenic microflora is determined.
Next, hardware research methods are assigned, the list of which is as follows:
- non-invasive examination of the rectum;
- probing imaging methods (endoscopy, colonoscopy);
- ultrasonography;
- ultrasound examination (adjacent organs are studied);
- contrast radiography or MSCT;
- irrigoscopy;
- MRI of the intestines.
Instrumentally penetrating research methods are not always applicable in individual cases. There is a risk of additional injury when inserting a probe rectally, and traditional methods such as ultrasound or radiography are sometimes unable to provide correct results due to layers of intestinal structures. The most informative, safe and painless method is magnetic resonance screening, which allows you to study even distant canal loops that are inaccessible to colonoscopy.
Duodenitis - symptoms, diagnosis, treatment
Pain as a symptom of intestinal inflammation
The duodenum is a small section of the intestine, 12 to 15 cm long. Ducts from the gallbladder and pancreas drain into it. Actually, “duoden” in Latin means “duodenum,” and the suffix “itis” indicates an inflammatory process. Causes causing this disease:
- Infections – first place goes to Helicobacter pylori
- Stressful situations - spasm of intestinal vessels occurs, blood circulation in the organ decreases. There is a decrease in immunity and an inflammatory process occurs
- Unbalanced diet, violation of eating patterns - prolonged fasting is replaced by an overabundance of food
- Bad habits – alcohol, smoking
- Eating before bed – you need to forget about nightly raids on the refrigerator
- Hereditary factor
- Drug damage
Symptoms of duodenitis:
- Epigastric pain
- Dyspeptic symptoms - nausea, vomiting, bloating, constipation or diarrhea
- General intoxication of the body - weakness, low temperature, loss of appetite, weight loss
The diagnosis is established using fibrogastroscopy - an endoscopic examination of the gastrointestinal tract. Therapeutic tactics for inflammation of the duodenum:
- Antibiotics – if infection is detected
- Diet No. 1 according to Pevzner - balanced nutrition
- Enzymatic preparations
- Adsorbents
- Antispasmodics to reduce pain
Treatment of the inflammatory process in the duodenum is long-term. Recommendations regarding diet and quality of nutrition will have to be followed for the rest of your life.
The nature of pain in pathologies of the colon
Weight loss is a sign of colon pathology.
Pain due to pathology of the colon has a unique localization. They are often felt on the side of the abdomen and near the anus.
Less common are unpleasant sensations in the epigastric region, as well as above the navel.
Even in the absence of pain, there will be pain when palpating the area in the iliac region on the right and left.
They become more intense if a person drinks milk or eats a lot of vegetables or coarse cereals. The main character of the pain is aching, accompanied by a feeling of fullness.
If the intestines are freed from gases and feces, the pain subsides. However, immediately before defecation, the pain may become more severe. Sometimes they are cramp-like in nature.
Enteritis - causes, symptoms, treatment
There can be many causes of intestinal inflammation
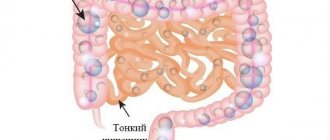
Enteritis is a pathological process in the small intestine. In this case, the absorption of nutrients, the processes of secretion of intestinal juice, and the protective functions of the intestinal wall are disrupted. The causes of this disease:
- Infections, viruses
- Toxic damage - poisons, drugs, mushrooms, alcohol, heavy metals, household and other chemicals
- Improper and unbalanced nutrition
- Helminthic infestation – Giardia, roundworms
- Hereditary and autoimmune diseases
- Surgery on the small intestine
- Adhesive process, peritoneal injuries
- Sedentary lifestyle
The main symptoms of acute enteritis:
- Frequent bowel movements - up to 10 times or more per day
- Epigastric pain, nausea, vomiting
- General intoxication of the body
- Temperature rise to critical values
- Coated tongue
- Dehydration, cramps, dry skin
- In case of prolonged and severe course - up to a state of shock
Symptoms of chronic enteritis differ from the acute process:
- Diarrhea that occurs after eating
- Pain syndrome is mild
- Changes in the appearance and composition of stool - wateriness, impurities, undigested food particles
- Hypovitaminosis
- Anemia
- Initial stages of osteoporosis
- Loss of body weight, in severe cases dystrophy
To make a diagnosis, the patient is prescribed the following tests and procedures:
- Stool, blood, urine tests - bacterial cultures, coprogram, feces for occult blood, general blood tests
- Biochemical blood tests
- Endoscopic and X-ray examinations
- Ultrasound of the peritoneal organs
Therapeutic tactics for enteritis:
Seven signs you have irritable bowel syndrome
Imagine the situation: there are unpleasant symptoms, but a medical examination shows that there is no problem. This is what affects the 6 to 18% of people worldwide who suffer from irritable bowel syndrome (IBS) (1).
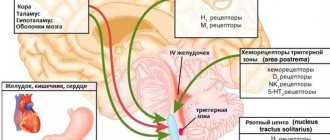
Abdominal pain
The cause of pain in the syndrome, which is not accompanied by any significant changes in the digestive tract, is problems with the transmission of signals from the intestines to the brain and back. The coordinated functioning of the digestive tract depends on their coordination. When there is interference in the brain-gut signaling pathway, pain occurs. With IBS, it usually appears in the lower abdomen, and after bowel movement it is significantly relieved.
How to make it easier?
A diet based on limiting the consumption of certain fruits, vegetables, sweets, milk and dairy products, legumes, and flour helps reduce pain in IBS. In addition, the doctor may recommend antispasmodic drugs that specifically relieve pain in the intestines.
Diarrhea or constipation
Impaired intestinal motility that occurs with IBS leads to changes in stool, and in different directions. In approximately 1/3 of cases, the syndrome is accompanied by weakness (2), or simply diarrhea. As a rule, this increases the frequency of trips to the toilet, according to some data, at least twice as much as normal (3). Another trouble is that the urge can arise suddenly, like a bolt from the blue.
Much more often, with IBS, the intestines contract too slowly, and much more fluid is absorbed from its contents than necessary, which leads to constipation. In such cases, the frequency of bowel movements is less than three times a week. Even when a long-awaited event occurs, it often does not bring relief - IBS is characterized by a feeling of incomplete relief. Sometimes constipation alternates with diarrhea.
How to make it easier?
For diarrhea, your doctor may prescribe antidiarrheal medications. To combat constipation, it is important to drink plenty of fluids, eat foods rich in fiber, and, if the problem persists, use laxatives.
Flatulence
Due to poor digestion in IBS, too much gas is produced in the intestines. As they accumulate, they cause discomfort: many patients consider bloating to be one of the most persistent and painful symptoms of the disease. Flatulence is also becoming the most common manifestation of irritable bowel syndrome, especially in women with a predominance of constipation or a mixed type, when the latter alternates with diarrhea (3).
How to make it easier?
Diet helps reduce the severity of bloating, in particular, reducing the proportion of fruits and vegetables, legumes and other foods in the diet that stimulate gas formation in the intestines. To alleviate the condition of already existing flatulence, drugs that have a so-called carminative effect help: they reduce the surface tension of gas bubbles formed in the intestines, which leads to their rupture. The gas itself is successfully absorbed by the intestinal walls or excreted naturally.
Intolerance to certain foods
In the vast majority of cases, manifestations of IBS are associated with errors in diet. Scientists today do not know why certain foods contribute to the exacerbation of the disease. Obviously, food intolerance has nothing to do with allergies and does not, in fact, cause indigestion, but only becomes a “trigger” of the syndrome. It’s interesting that everyone has their own trigger foods, but there are also some patterns. Pastries and cakes, peas and beans, cabbage and plums, and many other gas-inducing foods that contain lactose or gluten can cause a flare-up of IBS.
How to make it easier?
The only solution to this problem is to identify trigger foods and reduce their share in the diet.
Fatigue and sleep problems
In approximately half of cases, IBS is accompanied by fatigue (4), low endurance, which limits opportunities both at work and in everyday life, and the more difficult it is to cope with stress, the more pronounced the symptoms of the disease can be. At the same time, it is not always possible to have a good rest and sleep: difficulty falling asleep and waking up is another characteristic symptom of IBS. By the way, if you spend half the night trying to sleep, it is likely that the next day the troubles will be compounded by an exacerbation of characteristic intestinal problems.
How to make it easier?
If fatigue and insomnia due to IBS are your case, most likely you will have a hard time without the help of a competent neurologist.
Anxiety and depression
It is still unclear what comes first: the symptoms of IBS, which lead to emotional distress, or, on the contrary, stress, which triggers intestinal dysfunction. However, it is clear that those who suffer from IBS are 50% more likely to have an anxiety disorder and 70% more likely to have mood disorders such as depression than those with normal bowel function (5). These are such serious numbers that every person experiencing IBS should carefully monitor their psycho-emotional state and if, for example, depressed mood, loss of self-confidence, unreasonable feelings of guilt, mood swings, or anxiety appear, immediately consult a psychiatrist.
How to make it easier?
In this situation, it is better not to rely on the help of “folk methods” for improving mood - they can only aggravate the condition. Antidepressants and anti-anxiety drugs, which should be prescribed by a doctor, can provide real help.
Sources:
- Sperber AD et al. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: a Rome Foundation working team literature review // Gut. — 2017; 66(6):1075–1082.
- Camilleri M. Intestinal Secretory Mechanisms in Irritable Bowel Syndrome–Diarrhea // Clinical Gastroenterology and Hepatology. — 2015; 13(6):1051–1057.
- Portincasa P. et al. Pan-enteric dysmotility, impaired quality of life and alexithymia in a large group of patients meeting ROME II criteria for irritable bowel syndrome // World journal of gastroenterology. - 2003; 9 (10): 2293.
- Han CJ, Yang GS Fatigue in irritable bowel syndrome: a systematic review and meta-analysis of pooled frequency and severity of fatigue // Asian Nursing Research. - 2016; 10 (1): 1–10.
- Janssens KAM et al. Mood and anxiety disorders in chronic fatigue syndrome, fibromyalgia, and irritable bowel syndrome: results from the LifeLines cohort study // Psychosomatic medicine. — 2015; 77(4):449–457.
Marina Pozdeeva, pharmacist, medical journalist
Photo depositphotos.com The author’s opinion may not coincide with the opinion of the editors