prebiotics
probiotics
metaprebiotics
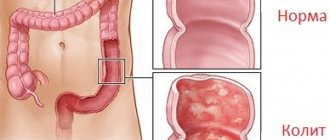
The normal balance of the microflora of the large intestine is an important condition not only for comfortable digestion, but also for creating a reliable immune defense of the body. Under the influence of external or internal negative factors, the development of dysbiosis (dysbiosis) is observed, which negatively affects the general condition of the body. Speaking about the difference between prebiotics and probiotics, it is necessary to become familiar with their function and the nature of their effect on the human body.
Gastrointestinal diseases
Microorganisms in the human intestine take up a lot of space. But in terms of mass, they weigh approximately 2-3 kg for an adult. A person of such weight not only has to be given water and food, but often also treated.
Artificial support is also often required for the intestines under conditions of stress, poor nutrition, and a sedentary lifestyle. And so-called probiotics and prebiotics are suitable for this case.
What are probiotics and prebiotics
Probiotics are beneficial substances for the human intestines.
Probiotics contain microorganisms specifically from among the beneficial inhabitants of the human intestine (these are symbiotic bacteria).
This drug also contains waste products of these types of bacteria. Drinking probiotics means populating your intestines with the “right tenants.”
Prebiotics do not contain microorganisms, but they are able to create optimal conditions for their development in the intestines. Often, these drugs consist of acids, enzymes, and oligosaccharides. It is these substances that microorganisms are accustomed to using as food, and prebiotics thus feed them and stimulate their development and growth.
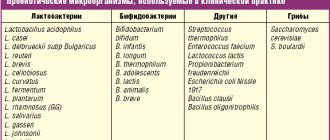
Classification of probiotics and prebiotics
Bifidumbacterin is a drug containing bifidobacteria.
Probiotics come in four forms. Monocomponent (they contain only one type of microorganisms):
- Bifidobacteria – “Bifidumbacterin”;
- Lactobacilli – “Lactobacterin”;
- Colibacteria – “Colibacterin”.
Multicomponent (contains several types of microorganisms):
Is there a “magic pill”?
Probiotic preparations appeared somewhere in the middle of the last century. Then they spread. The drugs demonstrated their remarkable properties in numerous experiments.
This group of drugs had practically no contraindications, and many thought that a magic elixir had been found. I took a pill and forgot about my health problems. But these were only forecasts. In practice, many patients simply wasted their money, and the results were not always pleasing to the patients. Currently, more and more reports have begun to come not about the benefits of the drug, but about its harm to health.
The effect of probiotics and prebiotics
Bifiform is a drug containing both prebiotics and probiotics.
Single-celled “antibiotics”, when they enter the intestines, begin a war immediately. The war for free living space.
These microorganisms begin to actively colonize the intestinal wall and leave virtually no room for pathogenic organisms.
As they settle in, beneficial bacteria are ready to change the pH of the environment towards acidic. Causative agents of intestinal infections are not ready to put up with “sour life” and so they simply die.
It is also worth noting that some types of bacteria have learned to synthesize antibiotics, which also affect harmful microbes.
This is why probiotics and prebiotics can be used during intestinal infections.
Prebiotics and sinobiotics: application and composition + useful table
In the last publication , we put together scientifically based facts about probiotics and provided a table with the composition of drugs and dietary supplements. In this article we look at the place of pre- and synbiotics in modern medicine.
Prebiotics - this term is used to refer to both prebiotics (containing substances that promote the growth of microorganisms) and metabiotics (containing metabolites, waste products of microorganisms). The most common prebiotic components: oligofructose, inulin, galacto-oligosaccharides, lactulose, breast milk oligosaccharides, butyrate, lactic acid, etc.
The mechanisms of action of prebiotics are associated with the interaction between the microbiota and the macroorganism and are divided into:
- Metabolic effects (production of short-chain fatty acids, absorption of calcium, iron, magnesium ions)
- Increased immunity of the macroorganism (production of IgA, modulation of cytokines)
There are quite strict requirements for prebiotics:
- should not be hydrolyzed by human digestive enzymes,
- should not be absorbed in the upper digestive tract,
- must selectively stimulate one species or a specific group of microorganisms resident in the colon.
The market for prebiotics and synbiotics is mainly a market for dietary supplements.
| Prebiotics (Metabiotics) | Galoctooligosaccharides, oligofructose, fructooligosaccharides (glucose, fructose, dextrose, maltose, maltotriose, maltodextrin - presented in synbiotics), lactulose (Duphalac, Normaze, Portlak, Prelax, etc.) Aqueous substrate of metabolic products of Escherichia coli DSM 4087, Enterococcus faecalis DSM 4086, Lactobacillus acidophilus DSM 4149 and Lactobacillus helveticus DSM 4183 ( Hilak Forte ) Calcium butyrate + inulin ( Zakofalk ) Metabolites of cell-free culture liquid of bacteria B.subtilis strain 3 + zeolite + fermented soy flour hydrolyzate ( Bactistatin ) Secretory enzymes from 16 strains of lactobacilli, obtained by fermentation for 1 year on soy + citric acid + lactic acid ( Daigo ) |
Scope of application of prebiotics: correction and prevention of dysbiotic conditions. [3,4]. For hepatic encephalopathy and functional constipation, lactulose is recommended as monotherapy with a high level of evidence (AB, read about levels of evidence here) [1]. International recommendations for the prevention (or prevention of relapse) of antibiotic-associated diarrhea (including those caused by Clostridium difficile) recommend complex therapy - oligofructose 4 g, three times a day with an average level of evidence [2]. In case of irritable bowel syndrome, the administration of prebiotics affects the quality of life (by normalizing stool, reducing the number of exacerbations and the intensity of abdominal pain syndrome), short-chain fructooligosaccharides 5 g/daily or galacto-oligosaccharides 3.5 g/daily – with level of evidence BC [1].
Note that in the Russian Federation, fructo- and oligosaccharides are presented only in the form of combined preparations, and in recommended quantities only as part of some synbiotics, for example, in the dietary supplements Enterolactis, Maxilak, RioFlora. In many products, the quantitative composition is not specified.
Synbiotics
Synbiotics are products containing both probiotics and prebiotics that have a positive effect on the health of the macroorganism [1].
| Synbiotics | Lactobacillus acidophilus CBT LA1 + Lactobacillus rhamnosus CBT LR5 + Bifidobacterium longum CBT BG7 + Bifidobacterium lactis CBT BL3 + Bifidobacterium bifidum CBT BF3 + Streptococcus thermophilus CBT ST3 + fructooligosaccharides (Neobiotic Lactobalance) Lactobacillus acidophilus CBT LA14 + Lactobacillus rhamnosus CBT LR32 + Bifidobacterium lactis CBT BL4 + inulin + vitamins B-B1, B6, B12 ( Floriosa ) Lactobacillus rhamnosus + Bifidobacterium bifidum + Lactobacillus acidophilus + Lactobacillus plantarum + Lactobacillus bulgaricus + inulin + psyllium ( Fitomucil Sorbent forte ) Lactobacillus Acidofilus LA-5 and Bifidobacterium BB-12+ fructooligosaccharides + nutriose + hydroxypropyl methylcellulose ( Florok forte ) Bifidobacterium animalis subspecies lactis BS01 + inulin, maltodextrin ( Probiologist transit [H7]) Bifidobacterium bifidum + Bifidobacterium longum + Bifidobacterium infantis + Lactobacillus rhamnosus + microcrystalline cellulose + oligofructose ( Florosan ) L.rhamnosus R049 + L.caseiR215 + L.plantarum R202 + L.acidophilus R053 + B.longum R023 + B.bifidum R071 + B.breve R070 + fructooligosaccharides ( Flora-Dophilus ) Bifidobacterium bifidum W23 + Bifidobacterium lactis W51 + Lactobacillus acidophilus W37 + Lactobacillus acidophilus W55 + Lactobacillus paracasei W20 + Lactobacillus plantarum W62 + Lactobacillus rhamnosus W71 + Lactobacillus salivarius W24 + inulin + fructooligosaccharides 1.2% ( RioFlora ) Bifidobacterium longum + Bifidobacterium breve + Lactobacillus acidophilus + Lactobacillus rhamnosus + Lactobacillus plantarum + Lactobacillus casei + Lactococcus lactis + Streptococcus thermophilus + Fructooligosaccharides 5 g + microcrystalline cellulose ( Maxilac ) Lactobacillus paracasei, strain CNCM I-1572 + fructooligosaccharides 5 g ( Enterolactis ) Lactobacillus acidophilus DDS®-1, B.bifidum UABB-10, B.longum UABL-14, B.lactis UABLA-12, rice maltodextrin, fructoologosaccharides ( LBS ) |
Synbiotics differ from probiotics in the presence of prebiotic components, as well as a more balanced composition with a larger number of strains of microorganisms in the composition of the preparations. Typically, the combination consists of several strains of bifdobacteria and lactobacilli. Also, synbiotics registered in the last few years already contain probiotic components in recommended doses - about 5 g of fructo-oligosaccharides.
Currently, the following combinations are recommended with moderate to low level of evidence (BC), due to insufficient number of studies:
- for antibiotic-associated diarrhea, probiotics and synbiotics, which contain from 3 to 8 components: Bifidobacterium bifidum W23, B. lactis W18, B. longum W51, Enterococcus faecium W54, Lactobacillus acidophilus W37 and W55, L. paracasei W72, L. plantarum W62, L. rhamnosus W71 and L. salivarius W24 [H9] - 109 CFU/g (5 g twice daily). Usually the combination includes several strains of different types of bacteria
- increase adherence to H. pylori eradication therapy - Mixture of Lactobacillus acidophilus and L. bulgaricus and Bifidobacterium bifidum and Streptococcus thermophilus and galactooligosaccharides 5 × 108 + 1 × 109, twice a day
- for irritable bowel syndrome - a number of combinations in a large dose as part of a synbiotic improves the quality of life of patients
- Lactobacillus rhamnosus NCIMB 30174, L. plantarum NCIMB 30173, L. acidophilus NCIMB 30175 and Enterococcus faecium NCIMB 30176 - 10 billion bacteria;
- Lactobacillus animalis subspecies lactis BB12®, L. acidophilus LA-5®, L. delbrueckii subspecies bulgaricus LBY-27, Streptococcus thermophilus STY-31 - 4 billion CFU, twice a day;
- Bifidobacterium animalis DN-173 010 in fermented milk (with Streptococcus thermophilus and Lactobacillus bulgaricus) 1010 CFU, twice daily.[1, 5]
An increase in the number of components did not make synbiotics universal drugs. Different combinations of microorganisms have shown their effectiveness for different conditions.
Let's summarize all biotics
At the moment, all recommendations for biotics are weak. For some nosoologies (ulcerative colitis, Crohn's disease, diarrhea, pseudomembranous colitis), the administration of probiotics, especially combinations, is not recommended due to insufficient knowledge [1,5]. There is also a possibility of developing sepsis caused by strains of probiotic microorganisms, in risk groups - the presence of immune deficiency, weakened patients, incl. with cancer, disruption of the intestinal epithelial barrier. [6]
At the moment, the main place of use for pro-, pre- or synbiotics is the prevention of dysbiotic conditions and the treatment of dysbiosis in specific pathologies as part of complex therapy. Probiotics of all generations continue to be used in clinical practice. The effect of a prebiotic will appear faster, but the probiotic will work longer. The choice of drug will be determined not only by clinical recommendations, the safety of the drug, but also by the specific clinical situation: in the presence of diarrhea syndrome, the drug of choice may be a 4th generation probiotic or a synbiotic, in the presence of bacterial overgrowth syndrome, sanitizing probiotics of the 2nd generation, and in case of constipation – Some prebiotics performed better. But how a pro- or prebiotic will work in each specific situation depends not only on the drug itself, but also on the individual characteristics of the human microbiota.
The use of probiotic and prebiotic and synbiotic drugs continues to be promising for further clinical research. Probiotic preparations are widely used in medical rehabilitation and a set of preventive measures [2]. Further research will strengthen the requirements for these drugs in terms of safety and proven effectiveness. Despite the wide variety of different strains of microorganisms and their combinations, the problem of individual selection of drugs remains unresolved. This is due to the fact that the intestinal microbiome is individual for each person, and modern methods for assessing the composition of the intestinal microbiota are not widely used.
Bibliography:
- WGO Practice Guideline - Probiotics and Prebiotics
- Microbiota. Edited by E.L. Nikonova and E.L. Popova. Media Sphere; 2022.
- Ardatskaya O.M. Probiotics, prebiotics and metabiotics. Medical advice. 2015; 13:94-99
- Maev I.V., Samsonov A.A., Plotnikova E.Yu. et al. Probiotics and prebiotics in clinical practice. Pharmateka. 2011; 5: 33-41.
- AGA Clinical Practice Guidelines on the Role of Probiotics in the Management of Gastrointestinal Disorders. Gastroenterology 2020;-:1–9
- Boyle R., Robins-Bowne R., Tang M. Probiotic use in clinical practice: what are the risks? J. Clin. Nutr. 2006; 83:1256–64.
You can discuss the latest news with all your Russian colleagues in chats:
- WhatsApp: https://chat.whatsapp.com/Izj3ZQ7aI36KK8e2dCjcm4
- Telegram: https://tglink.ru/joinchat/GWBPCkkLipQUnTbXrKqzGA
- VKontakte: https://vk.me/join/AJQ1dzabQRfHvl5Y2AOVUsgJ
Our educational portal takes care of the constant improvement of the qualifications of doctors. The list of additional professional development programs within the framework of CME lasting 36 hours is available at the link. Webinar schedule is here. There is a convenient search by specialty, join us!
Based on the materials of the article.
Why probiotics can fail and what affects this
Before taking probiotics, you need to properly prepare your body.
Often, probiotics begin to fail due to inadequate treatment, if we try to influence only the symptoms of the disease, but without eliminating its causes:
- Hormonal disorders, chronic infections and diseases;
- Nutritional deficiency over a long period of time (low intake of plant fiber from food, insufficient consumption of fermented milk products, during fasting and a monocomponent diet);
- Long-term use of medications (more than 7-14 days of treatment with antibiotics, treatment with antisecretory agents, laxatives, oral contraceptives, corticosteroids);
- Also excessive consumption of flavor enhancers, dyes, preservatives;
- For immunodeficiency.
Elderly people are particularly at risk. Also people who have undergone abdominal surgery. In all the cases described above, conditions unsuitable for the existence of beneficial bacteria remain in the intestines for a long time.
And consequently, taking probiotics and prebiotics at these moments may not give the desired result, but only have temporary effects. If you start taking medications correctly, you should prepare your body in advance:
- Achieve remission of chronic diseases;
- Restore hormonal levels;
- Get rid of foci of infection;
- Adjust your diet.
The video story will tell you about the restoration of intestinal microflora and prebiotics:
Differences between the two groups
Probiotics are live microorganisms that are beneficial to the intestinal microflora. These include lacto-, coli-, propino- and bifidobacteria, yeast-like fungi, bacillus spores, enterococci and lactic streptococci. Once in the body, they suppress the growth of pathogenic agents, thereby restoring microbial balance. Probiotic products may contain one group of beneficial microorganisms or several. This depends on the generation of the drug chosen.
Prebiotics are substances of non-microbial origin. These are chemical compounds that create favorable conditions for the work of beneficial bacteria. These include fiber, lactulose, inulin, sorbitol, and fructosaccharides. Prebiotics are not broken down in the small intestine and are not digested in the upper gastrointestinal tract. The substances serve as a breeding ground for beneficial microorganisms, thereby helping to maintain the balance of microflora.
Probiotics “to order”
This is a fairly new direction. Scientists are forced to engage in such developments due to the rejection of any types of drugs from the probiotic groups in some organisms.
Since there are frequent cases when the drug is rejected by the indigenous intestinal microflora. As if it were a foreign organ being transplanted, despite significant kinship. And even the best probiotics cannot always get along in such conditions.
This is how “custom-made” probiotics began to appear. They are created from the flora of this person. The method involves freezing normal human intestinal flora in liquid nitrogen. And then it is used as a probiotic if necessary.
Thus, on the eve of a stressful situation for the body, it will be possible to prepare treatment for it in advance using its own microflora, simply prepare a sample in a cryobank.
This can also be done on the eve of long-term medication use, pregnancy, on the eve of surgery, a business trip and other cases.
Side effects
Probiotics contain bacteria that would normally already be present in the body. However, some problems can arise if probiotics are taken in the hope of quickly getting rid of unpleasant symptoms that accumulate over a long period of time. Chronic diseases, immunodeficiency, hormonal disorders, long-term treatment with antibiotics can create a situation in the body where probiotics will not have a very noticeable effect. In this case, step-by-step therapy should be carried out, including various measures to eliminate symptoms and restore the microflora.
Prebiotics should be used with caution for certain gastrointestinal diseases. Prebiotics can also cause enzymatic disorders in the intestines and an osmotic effect in the liver. Abuse of food containing prebiotics may result in diarrhea, flatulence, and intestinal colic.
Strategies
Lactobacterin is a drug containing natural intestinal microflora.
All groups of probiotics can be divided into two large groups.
The most common probiotics available are those that contain natural intestinal microflora. Among these drugs the following names can be noted:
- "Mutaflor";
- "Colibacterin";
- "Nutrolin";
- "Lactobacill";
- "Biobakton";
- "Lactobacterin";
- "Bifidumbacterin".
These drugs contain either bifidobacteria, or lactobacilli, or colibacteria. This group has been used in medicine for more than 80 years and is quite well studied. The advantages of these drugs:
- Almost complete absence of contraindications;
- Almost complete absence of side effects;
- Mild physiological effect.
Disadvantages of these drugs
It is worth noting that the therapeutic effect of these drugs decreases every year. After all, in order to provide the proper therapeutic effect, such drugs need to undergo a course of settling in the intestines.
Bacterial and biological preparations for the correction of dysbiosis and their rational use
Miroshnik O.A., Ph.D.
The article was published in Omsk Medical Newspaper No. 8 (29), May 1997.
In recent years, new approaches to treatment have become widespread, related to the restoration of the natural ecology of the body and based on the use of active biological products. One aspect of this approach is the normalization of the altered microbial landscape of the body with the help of bacterial and biological products. Currently, through the efforts of new industrial and commercial structures, the traditionally existing shortage of bacterial and biological products has been largely eliminated. Moreover, in addition to such long-familiar drugs as bifidumbacterin, lactobacterin, colibacterin and bificol, many new drugs have appeared, among which it is difficult for doctors, pharmacists and patients to navigate. We hope that the systematization of bacterial preparations proposed in this publication intended to correct the biocenosis of mucous membranes will help more complete and effective use of their entire rich arsenal in everyday practice.
1. BACTERIAL PREPARATIONS - EUBIOTICS
The most significant group of bacterial drugs are eubiotics
- medicines containing as active substances certain strains of representatives of the microflora of a healthy human body
.
It is known that bacteria that normally populate the mucous membranes have an antagonistic effect on pathogenic and opportunistic microflora and provide vitamin-forming and enzymatic functions. 1.1. Preparations of the bifidobacteria family.
The most famous and widely used eubiotic drug is Bifidumbacterin
, containing bifidobacteria of the bifidum species. It is this type of bifidobacteria that predominates in the intestines of newborns and children of the first years of life, therefore bifidumbacterin is the basic drug for correcting intestinal biocenosis in children. The indications for the use of bifidumbacterin are very wide, but the main ones are intestinal dysfunction due to dysbacteriosis, acute intestinal infections (AI), use for prophylactic purposes in weakened children with anemia, rickets, diathesis and during the early transfer of children from breastfeeding to artificial feeding, etc. d..
There are four main forms of release of Bifidumbacterin: vial, ampoule, tablet and powder in laminated foil bags
. The use of bifidumbacterin in pediatrics dictates extremely stringent requirements for the quality of the drug, and, above all, for the absence of foreign microflora. In this regard, the tablet form of bifidumbacterin is approved for use only from three years of age. From the neonatal period, only Bifidumbacterin in powder, bottles or ampoules is approved for use. A number of significant advantages have the form of Bifidumbacterin in powder produced by JSC “Partner”, which is a mixture of dry bifidobacteria with chemically pure lactose, packaged in gas-tight bags made of laminated aluminum foil. The production technology of this drug involves the removal of the cultivation medium and the almost complete absence (less than 10%) of dead bacterial cells. Therefore, when the drug dissolves, an almost colorless opalescent suspension without a pronounced odor or taste is formed. Lactose, which promotes the growth of bifidobacteria in the intestines, slightly increases the dissolution time of the drug.
Bifidumbacterin-forte
- a complex bacterial preparation containing bifidobacteria of the bifidum species immobilized on stone activated carbon. Upon contact with the intestinal mucosa, the sorbent allows the growth of bifidobacteria in the form of individual microcolonies. The drug has all the properties of bifidumbacterin and at the same time the antitoxic effect inherent in the sorbent. The drug has a more pronounced clinical effect and is able to normalize the disturbed intestinal biocenosis at an earlier time compared to conventional bifidumbacterin. The drug is used after a meal and does not require prior dissolution in water.
Bifidumbacterin in suppositories
used for the treatment of intestinal dysfunction with damage to its distal parts (colitis, proctitis) and in gynecological practice (senile nonspecific bacterial colpitis, bacterial vaginosis, impaired vaginal cleanliness of 3-4 degrees, preparation of the birth canal for childbirth, etc.).
Bifidin
as an active ingredient it contains bifidobacteria of the Adolescentis species, which have a wider spectrum of carbohydrate fermentation. However, this type of bifidobacteria grows in the intestines of adults and children over three years of age. In children under one year of age, Bifidobacterium adolescentis is found only if they are bottle-fed. The drug is prescribed to children over three years of age with intestinal disorders accompanied by dysbacteriosis, sick children on early artificial feeding, with a protracted course of intestinal dysfunctions, with repeated isolation of pathogens after acute intestinal infections.
Bifilong
contains bifidobacteria of the species longum, which are the second in quantitative content after bifidobacteria of the species bifidum, representatives of the normal microflora of breastfed children. There is currently no industrial production of Bifidin and Bifilong.
Bifiliz
- a combined preparation containing bifidobacteria of the type bifidum and lysozyme (in one bottle 5 doses and 10 mg, respectively). Lysozyme has bifidogenic, immunomodulatory, anti-inflammatory, reparative and antimicrobial effects. The optimal combination of bifidobacteria and lysozyme in this preparation allows us to enhance the therapeutic effect of each component.
In Novosibirsk, CJSC NPF Vector-Biomed has mastered the production of Bifidobacteria Concentrate
, which is a suspension of bifidobacteria, the bifidum species, in a milk culture medium. The drug is registered as a food supplement and is distributed through a distribution network of doctors. The advantage of the Concentrate is that the bifidobacteria in the preparation are in the growth phase and, therefore, they are more active. However, the fact that to achieve a clinical effect requires taking the Concentrate in doses tens of times higher than those used in treatment with pharmacopoeial bifidumbacterin (8000 and 300 doses, respectively) casts doubt on this.
In Novosibirsk, Bio-Vesta LLC produces an almost similar drug - Liquid concentrate of bifidobacteria (Biovestin)
, the active substance in which is bifidobacteria of the Adolescentis species, the features of which are mentioned above.
1.2. Preparations of the lactobacilli family
Lactobacilli, together with bifidobacteria, are also the main representatives of the normal human microflora. Lactobacilli are present in all parts of the digestive tract, from the oral cavity to the colon, are the predominant flora of the genital tract, and are found in breast milk.
The first attempts at the therapeutic use of lactobacilli to correct biochemical processes occurring in the intestines were made by I.I. Mechnikov 100 years ago. Subsequently, a pronounced antagonistic activity of lactobacilli was discovered against putrefactive opportunistic microorganisms and pathogens of acute intestinal and infections, which is associated with the ability of lactobacilli to form lactic acid, hydrogen peroxide, lysozyme and other substances with antimicrobial action against a wide range of gram-positive and gram-negative bacteria. The reparative properties and immunomodulatory role of lactobacilli have been revealed, manifested in particular in the ability to increase the general level of secretory Ig A and titers of specific secretory antibodies, enhance phagocytosis, etc. The role of lactobacilli in reducing cholesterol levels in the blood, preventing the production of carcinogens and in the destruction of oxalic acid is discussed. thereby preventing the formation of oxalates in the body.
Lactobacterin is widely used in our country.
, created in the early 70s based on lactobacilli of the plantarum species, which, like bifidobacteria, have an antagonistic effect against pathogenic and opportunistic microorganisms. Indications for its use are similar to those of bifidumbacterin.
Acilact , was developed at the Moscow Research Institute of Epidemiology and Microbiology named after G.N. Gabrichevsky
, which includes lactobacilli of the species acidophilus. Unlike lactobacilli of the plantarum species, acidophilic lactobacilli used for the preparation of Acylact belong to the category of obligate microorganisms for humans. The criteria for selecting a new industrial species of lactobacilli were the ability of bacteria to form acids, antimicrobial activity, adhesive properties that promote long-term preservation in the intestines, resistance to the action of digestive secretions and antibiotics used. The new drug Acylact meets all these conditions.
Acylact is used for indications common to other bacterial preparations: intestinal dysbiosis, acute intestinal infections, chronic enterocolitis, as well as inflammatory diseases of the oral mucosa. Since Acylact is characterized by increased acid-forming activity, it is preferable for the treatment of dysbiosis in patients with hypoacid conditions and reduced intestinal motility.
The reduced content of lactose in Acylact, combined with the high ability of the acidophilic lactobacilli that form the basis of the drug to break down lactose, makes Acylact the drug of choice for the treatment of intestinal dysbiosis in patients with milk intolerance (lactase deficiency).
The use of Acylact for 2-3 courses in children with atopic dermatitis leads to normalization of initially depressed immunity and improvement of clinical symptoms.
Acylact can be used to treat gynecological diseases accompanied by disturbances of the vaginal microflora, but in this case it is more convenient to use Acylact in suppositories
. Normally, the vaginal microflora is represented mainly by lactobacilli, the so-called Dederlein bacilli, which maintain an acidic environment in the vagina and suppress the growth of opportunistic microorganisms. Acylact in suppositories is used for pathological conditions associated with a deficiency of lactoflora of the female genital tract, which are especially significant for the following diseases:
- Senile colpitis. The degree of colonization of the vaginal mucosa by lactobacilli depends on the production of estrogen, therefore, in the postmenopausal period, with estrogen deficiency, the level of lactoflora decreases, which is associated with the development of a number of symptoms of senile colpitis (dryness, atrophy of the mucosa, etc.), as well as an increase in the frequency of urinary infections.
- Nonspecific bacterial colpitis caused by staphylococcus, Escherichia coli or their association.
- Persistent violation of the purity of vaginal secretions up to 3-4 degrees.
- Bacterial vaginosis, which is known to be characterized by the proliferation of anaerobic flora and a sharp depletion of the vaginal mucosa in lactobacilli. In this case, Acylact is included in complex therapy, which also includes the use of metronidazole or clindamycin.
- Long-term courses of antibiotic therapy that suppress the natural microflora of the vagina.
- Prevention of bacterial colpitis and cystitis with frequent changes of sexual partners.
- In combination with other drugs in the treatment of chlamydia and mycoplasma infection of the female genital tract.
- Preparation of the birth canal for childbirth, since the biocenosis of the newborn’s intestines that forms from the first hours of life largely depends on the microbial landscape of the mother’s birth canal.
A contraindication to the use of Acylact in suppositories is candidiasis, since in some cases a rapid shift in pH to the acidic side promotes the growth of fungi. Acylact in this case is used after specific antifungal therapy or after the use of Bifidumbacterin in suppositories.
Acilact is also available
, the use of which by resorption in the mouth is indicated for inflammatory diseases of the gums and oral mucosa
Acipol
- a combined preparation consisting of lactobacilli acidophilus and heat-inactivated kefir grains (Kefir grains), available in tablets of 5 doses. The drug is highly active against pathogenic and opportunistic microflora and normalizes some immunological parameters. Acipol is prescribed from the first days of a child’s life for acute intestinal infections, dysbiosis, weakened patients with signs of exudative diathesis and other allergic manifestations.
1.3. Preparations of the colibacterium family
A drug from the colibacterium family - Colibacterin
is the very first domestic bacterial preparation. It contains an antagonistically active strain of non-pathogenic Escherichia coli M-17. Some experts believe that this strain, isolated many years ago, has now somewhat lost its antagonistic activity and ability to take root in the intestines. Colibacterin is used mainly for chronic diseases of the colon in elderly people, in whom the microflora of this part of the intestine is populated predominantly by E. coli, as well as for dysbacteriosis caused by the presence of hemolyzing forms of E. coli.
Combined drug Bifikol
contains bifidobacteria of the bifidum species and Escherichia coli strain M-17, therefore, its action and indications for use are in many ways similar to those of Bifidumbacterin and Colibacterin.
Many eubiotic drugs are also produced abroad, but due to the high cost, attempts to widely introduce them on the Russian pharmaceutical market have so far been unsuccessful.
Bifiform
(Ferrosan)
is available in capsules with a gastroinsoluble coating and contains bifidobacteria of the bifidum species and enterococci.
Primadophyllus
company
(Nature's Way)
is available in two forms.
The powder for preparing the suspension contains bifidobacteria of the infantus and longum species and lactobacilli of the acidophilus and banmosus species. This form is intended for children from the first days of life to 5 years. The capsule version of the drug additionally contains bifidobacteria of the brevis species and is intended for children aged 6 to 12 years. Primadophilus is distinguished by the absence of allergenic factors in its composition; capsules are more convenient to take compared to powders, which must first be dissolved in water. Another foreign drug - Probionik (Enrich)
is a chewable tablet with a pleasant strawberry flavor containing bifidobacteria of the species adolescentis, infantis, longum and lactobacilli acidophilus. These drugs are certified as food supplements and are usually distributed through a network of private distributors. It should be noted that the cost of one package, designed for a 6-8 week course of treatment, is about 25 US dollars. dollars for Primadophilus and about 20 US. dollars for Probionik, which puts effective, inexpensive and well-known Russian drugs beyond competition.
2. DRUGS - PROBIOTICS
Another large class of biological products used to correct dysbiosis and treat diarrheal diseases are probiotics.
. Probiotics are activators of the growth of normal microflora and release substances that suppress the proliferation of pathogenic microorganisms.
The best known probiotics are those containing pure spores of the bacteria Bacillus subtilis strain IP 5832. These are Bactisubtil
(Hoechst Marion Roussellt, currently Aventis) and
Flonivin BS
(ICN)
. In Russia, a similar drug called Bactisporin
is produced by the NPO Immunopreparat in Ufa.
The difference between Bactisporin is that it contains lyophilized live bacteria Bacillus subtilis strain No. 3H. The new drug Biosporin
is designed on the basis of the association of two types of spore-forming microorganisms B.subtilis 3 and B.licheniformis 31. The industrial production of the drug is carried out by the TsVTP BZ MO RF. Biosporin is characterized by pronounced specific activity against Staphylococcus aureus and fungi of the genus Candida. It has been established that Biosporin, along with pronounced selective antagonistic activity against pathogenic and conditionally pathogenic microorganisms, is characterized by the ability to significantly enhance the body's defense reactions - increase the phagocytic activity of blood leukocytes, induce the production of endogenous interferon, etc.
All drugs based on spores of the bacteria Bacillus subtilis have a similar mechanism of action. The bacillus spores germinate into a vegetative form in the small intestine. This process reaches its maximum in the ileocecal region. When spores germinate, enzymes are released that promote the breakdown of proteins, fats and carbohydrates, and an acidic environment is formed that prevents decay processes and the growth of pathogenic bacteria. In addition, enzymes cause direct lysis of the cell walls of Proteus, Escherichia coli, and pathogenic staphylococcus. Since this strain of bacilli was obtained artificially and is not a physiological component of the intestinal biocenosis, caution is recommended when prescribing drugs from spore-forming microorganisms: their use in short courses and with a weak effect from the previous use of eubiotic bacterial drugs.
Linex
(Lek)
is more physiological , containing acidophilus lactobacilli bacteria, bifidobacteria infantis species and fecal streptococci as active ingredients. Lactic acid bacteria produce lactic, acetic and propionic acids. The acidic environment they create in the intestines is unfavorable for the growth of pathogenic microorganisms. Lactic acid bacteria are involved in the resorption of monosaccharides, stabilize the membranes of intestinal epithelial cells and regulate the absorption of electrolytes. Representatives of normal microflora (bifidobacteria and fecal streptococci) contribute to the restoration of intestinal biocenosis.
Enterol
(Biocodex)
contains lyophilized fungi Sacchoromyces boulardii.
The drug normalizes the disturbed balance of intestinal microflora, promotes the production of secretory Ig A by lymphoid cells of the intestinal mucosa. Enterol is effective for diarrhea caused by taking antibiotics, including pseudomembranous colitis caused by clostridial spore-forming microflora. Hilak
(Ludwig Merkle)
- a liquid containing a sterile concentrate of metabolic products of intestinal flora symbionts, biosynthetic lactic acid, short-chain volatile fatty acids and other components.
These biological products change the acidity of the intestinal contents to the acidic side, create unfavorable conditions for the growth of pathogenic microorganisms and stimulate the growth of normal microflora, improve the physiological functions of the gastrointestinal tract, promote the regeneration of the mucous membrane, and restore the disturbed water-electrolyte balance in the intestinal lumen. Hilak is indicated for intestinal dysfunctions and allergic diseases associated with intestinal dysbiosis, for the prevention of dysbiosis and acute intestinal infections that occur during sudden changes in climatic conditions (travelers' diarrhea), etc. Lactulose
- a synthetic disaccharide produced under different brand names (
Normaze, Laktofalk, Duphalac, Portolac,
etc.) can also be classified as probiotics. Lactulose does not undergo hydrolysis in the small intestine and enters the colon unchanged, where it creates a natural nutrient medium for the growth of lactic acid bacteria, resulting in the formation of lactic and short-chain fatty acids, increased acidity and increased peristalsis of the large intestine. The drug inhibits the growth of salmonella in the intestine, reduces the formation of nitrogen-containing substances and prevents the absorption of ammonia in the colon. Lactulose is used for chronic constipation, salmonellosis, digestive disorders associated with putrefactive processes as a result of food poisoning in infants and children under 10 years of age, as well as for hepatic encephalopathy.
Unusual properties have been discovered in the synthetic proteolytic enzyme inhibitor PAMBA
(BYK GULDEN)
.
PAMBA increases the growth of lactobacilli, bifidobacteria and Escherichia coli, while simultaneously reducing the proteolytic activity of Proteus, pseudomonads and other microorganisms and enhancing macrophage phagocytosis. Pantothenic acid also has bifidogenic properties ( Calcium pantothenate, Panthenol
), included in many multivitamin preparations, or used as a separate preparation.
3. BACTERIOPHAGES
bacteriophages are successfully used to sanitize mucous membranes, skin and wound surfaces from pathogenic and opportunistic bacteria.
. Bacteriophages are viruses that exclusively infect bacteria; they are environmentally friendly biological objects for humans and can be used to treat dysbacteriosis, acute intestinal infections, and purulent skin infections at any age.
Bacteriophages, like other viruses, are absolute intracellular parasites; their reproduction occurs in a living cell. Having penetrated the bacterium through phage-specific receptors located on its surface, the phage DNA changes the synthesizing mechanisms of the cell, forcing the bacterium to synthesize phage DNA and proteins. At a certain stage, the bacterium is destroyed, and a new generation of daughter bacteriophages emerges from it. An important property of bacteriophages is their high specificity; they selectively lyse not only bacteria of a certain type, but even their individual serological groups. Bacteriophages accurately find and destroy only those bacteria against which their action is directed, without affecting the normal microflora of the body, not to mention its own cells. This is precisely what explains the absence of side effects and contraindications to the use of bacteriophages, which makes their use in pediatric practice especially attractive. The emergence of antibiotic resistance in bacteria does not affect their sensitivity to bacteriophages, so the latter are often active even against multidrug-resistant hospital microflora. However, the specificity of bacteriophages should be taken into account: each type of phage is recognized as its target only by those serotypes of bacteria that have certain phage-specific receptors. Therefore, it is necessary to prescribe bacteriophages under microbiological control of the sensitivity of the given pathogen to them.
The domestic industry produces a wide range of medicinal bacteriophages: Staphylococcal, Streptococcal, Coli, Proteus, Pseudomonas, Klebsiella, Typhoid, Dysenteric, Salmonella
.
There are also their combined forms: Coliprotein bacteriophage
,
Intesti bacteriophage
(contains phages of Shigella Flexner serovar 1,2,3,4,6 and Sonne, salmonella (paratyphoid A and B, enterilitis, typhimurium, cholera suis, Oranienburg), enteropathogenic groups of Escherichia coli , Protea vulgaris and mirabilis, staphylococci, Pseudomonas aeruginosa and pathogenic enterococci),
Pyobacteriophage combined
(contains phages of staphylococci, streptococci, pathogenic Escherichia coli, Proteus and Pseudomonas aeruginosa).
Consonant, but still different, the purified polyvalent Pyobacteriophage
contains phages of staphylococci, streptococci, pathogenic Escherichia coli, Pseudomonas aeruginosa, Proteus and Klebsiella pneumoniae
. This drug is distinguished by the highest degree of purification from bacterial metabolites, which significantly improves its taste and makes it the first choice for children under one year of age. The purified polyvalent Klebsiella bacteriophage
is active against
Klebsiella pneumonia, ozena, and rhinoscleroma
. Bacteriophage are usually produced in liquid form or in tablets; currently, the production of combined Pyobacteriophage and Staphylococcal bacteriophage in the form of liniment has also been launched.
So far, bacteriophages have been most widely used in the treatment of intestinal dysbiosis, acute intestinal infections, enterocolitis, and purulent-inflammatory diseases of the throat and nose. However, the scope of their clinical application is much wider and they can be successfully used to treat surgical, urogenital, skin and other infections.
There is no mention of phage therapy in foreign manuals. But it is necessary to take into account that, firstly, phage therapy is a special direction in bacteriology, developed by Russian scientists, and, secondly, the use of bacterial preparations for therapeutic purposes in Western standards is generally extremely limited. For example, in the USA, almost all bacterial preparations are classified as food additives, and, therefore, are not included in standard treatment programs. Bacterial preparations fall into the sphere of interest of nutritionists who have tasks other than medical ones. Perhaps it is not an exaggeration to say that Russia has accumulated much more scientific material and experience in the use of bacterial preparations in medicine.
4. IMMUNOGLOBULIN PREPARATIONS
A fundamentally new direction in the treatment of dysbacteriosis and acute intestinal infections is associated with the creation in our country of an original drug, a complex immunoglobulin preparation.
(KIP) KIP contains human immunoglobulins of three classes: Ig A (15-25%), Ig M (15-25%) and Ig G (50-70%). What distinguishes CIP from all other immunoglobulin preparations used in Russia is the high content of Ig A and Ig M, an increased concentration of antibodies to enteropathogenic bacteria of the intestinal group (Shigella, Salmonella, Escherichia, Klebsiella, etc.), a high concentration of antibodies to rotaviruses, as well as oral mode of application.
Ig M, which is part of the CIP, has a bactericidal effect on pathogenic microorganisms, Ig A makes it difficult for them to attach to the epithelium of the mucous membrane, reproduce and ensures rapid removal from the intestine, Ig G neutralizes microbial toxins and viruses, mediates the “sticking” of bacteria to macrophages with their subsequent phagocytosis . In addition to removing pathogenic and opportunistic microorganisms from the body, CIP promotes the growth of normal intestinal microflora (bifidobacteria, lactobacilli, enterococci and non-pathogenic Escherichia coli), increases the production of secretory Ig A and normalizes altered indicators of systemic immunity. The oral method of taking CIP ensures the delivery of large doses of the active substance to the lesion site with a subsequent decrease in the adsorption of pathogens on the epithelial cells of the intestinal mucosa and a local immunomodulatory effect.
A large comparative study showed that among all possible treatment regimens for acute intestinal infections in children, it is CIP therapy that gives the best results, assessed by such parameters as the duration of symptoms of intoxication and diarrhea syndrome, re-seeding of pathogens, changes in the intestinal biocenosis and the dynamics of the main indicators of immunity.
A positive effect of CIP in the treatment of allergic dermatoses was noted. This is explained by an increase in the level of secretory Ig A, as a result of which the local resistance of the gastrointestinal mucosa increases and the removal of allergens from food from the intestine increases.
The main indications for the use of CIP are the following diseases and pathological processes:
- Intestinal dysbiosis in children and adults, caused by any factors (post-acute intestinal infections, long-term and irrational antibiotic therapy, chronic diseases, stress, immunodeficiency states, etc.).
- Acute intestinal infections. The possibility of obtaining a pronounced therapeutic effect 2-3 days after the start of administration makes CIP the drug of choice in the treatment of acute intestinal infections (including rotavirus etiology) in children of the first year of life.
- Chronic enterocolitis.
- Complex therapy of allergic dermatoses combined with intestinal dysfunction.
- Immunodeficiency states with disorders mainly in the humoral immunity.
At the Research Institute of Epidemiology and Microbiology named after G.N. Gabrichesvsky, together with f, a combination drug Kipferon
in rectal and vaginal suppositories, which includes KIP in an amount of 50 mg and recombinant interferon-alpha2a in a dose of 500,000 IU.
5.FOOD ADDITIVES
To correct the intestinal microflora, special food additives are used that contain dietary fibers related to carbohydrates, which are not digested by digestive enzymes, but serve as a nutrient substrate for the microflora of the large intestine. Dietary fibers that have a stimulating effect on the intestinal microflora include oligosaccharides, in particular fructooligosaccharides, the most famous representative of which is inulin
. A large amount of inulin is contained in Jerusalem artichoke root crops. There are several food supplements containing Jerusalem artichoke concentrate (Jerusalem artichoke concentrate, Topivit, Jerusalem artichoke concentrate, etc.). Fructooligosaccharides and, in particular, inulin significantly stimulate the growth of bifidobacteria in the intestine, change the pH of the large intestine to the acidic side, promote the formation in the intestine of short-chain fatty acids and other biologically active substances that have a beneficial effect on the intestinal biocenosis.
6. HEALTHY FERMENTED MILK PRODUCTS
Characteristics of drugs used to correct mucosal biocenosis would be incomplete without mentioning fermented milk products containing bifidobacteria and lactobacilli. These products are intended for daily nutrition and have certain regulatory functions. There are hundreds of recipes for such products produced abroad; several dozen have been developed in Russia. A number of fermented milk products are also produced in Omsk. So in the composition of the fermented milk mixture Narine
includes acidophilic lactobacilli and their metabolic products.
Pastolakt
contains special strains of acidophilus bacillus and bifidobacteria growth factors.
Acidolact
contains acidophilic lactobacilli with lactic acid streptococcus.
Bifido-containing products are represented by Bifilin
, obtained from bifidobacteria of the species
Adolescentis
and characterized by deep hydrolysis of the protein component, and
Bifidok
- kefir, enriched with bifidobacteria of the species
bifidum
.
7. RATIONAL THERAPY FOR PATIENTS WITH INTESTINAL DYSBACTERIOSIS
The scheme for correcting intestinal dysbiosis can be divided into several stages.
1. Sanitation of the intestines from opportunistic microflora.
Traditional treatment of patients with intestinal dysbiosis involves preliminary decontamination of the intestine using antimicrobial agents. However, the latter often cause side effects that make it difficult to draw up a rational treatment program, especially for a child. In most cases, effective and safe decontamination of the intestine from opportunistic bacteria is possible by replacing antimicrobial agents with safer and highly effective bacterial preparations: CIPs and bacteriophages. Enteral administration of KIP 1 dose 1-2 times a day has a sanitizing effect against most gram-negative enteropathogenic bacteria (Escherichia, Klebsiella, Proteus, as well as Shigella and Salmonella). Depending on the opportunistic microflora present, bacteriophages are additionally prescribed internally (Intesti-bacteriophage, combined Pyobacteriophage, purified polyvalent Pyobacteriophage, Staphylococcal or Klebsiella bacteriophages). If there is an overgrowth of clostridia, Enterol is used.
2. Replacement therapy with bacterial drugs.
After antimicrobial therapy, depending on the identified deficiency of a particular type of bacteria, bacterial preparations are prescribed for 4 weeks in standard doses. In children, Bifidumbacterin or Bifidumbacterin-forte is more often used, in adults - Bifidumbacterin, Bifidumbacterin-forte or Bifikol, in the elderly - Bifikol or Colibacterin. Then, in order to maintain the clinical effect, dry Acylact is indicated for 2 weeks, which helps increase acidity in the intestines and stabilize the composition of the microflora. The use of bacterial preparations is combined with the use of Hilak-Forte drops in moderate therapeutic doses. For constipation, Lactulose and Acylact or Bifidumbacterin in suppositories also have a good effect.
Simultaneously with the start of treatment, the patient takes vitamins A, E and group B as part of multivitamin preparations (Glutamevit, Complivit, Kvadevit, Unicap-M, Centrum, etc.), enzyme preparations: Festal, Panzinorm-Forte, Digestal (for constipation) or Mezim -Forte, Pancreatin, Pankurmen, Pancintrat (for diarrhea syndrome).
3. Maintenance therapy.
After a course of bacterial preparations, food supplements containing inulin (Jerusalem artichoke concentrate, Topivit, Jerusalem artichoke concentrate, etc.) are prescribed for 2-3 weeks. After the main course of treatment, herbal medicine is prescribed (infusions of St. John's wort, sage, yarrow, plantain leaf, mint, etc.), in the selection of which much attention is paid to individual intolerance to herbs, manifested by dyspeptic complaints, changes in gastrointestinal motility, and allergic reactions. The full course of treatment ends with a 3-4 week intake of adaptogenic agents. The patient is also given recommendations on a balanced diet, including the use of medicinal fermented milk and vegetable products.
When carrying out this therapy, it is necessary to keep in mind that dysbiosis is not an independent nosological unit, but only a pathogenetic link of the underlying disease, therefore the main attention should be directed precisely to its decoding and treatment.
Thus, doctors and patients today have a sufficient choice of means to preserve and maintain the balance of the normal microflora of the body. The task is their rational and targeted use, taking into account the individual characteristics of the biocenosis of a particular patient, which depends on an understanding of the differences in the action of individual drugs and a clear understanding of the therapeutic goals pursued when prescribing them.
Recommended reading:
Elisabeth Kütter. Phage therapy: bacteriophages as anibiotics. PHAGE THERAPY: BACTERIOPHAGES AS ANTIBIOTICS. Elizabeth Kutter, Evergreen State College, Olympia, WA 98505 - Nov. 15, 1997. (PDF)
Elisabeth Kütter “Phage therapy: bacteriophages as antibiotics”
“PHAGE THERAPY: BACTERIOPHAGES AS ANTIBIOTICS. Elizabeth Kutter, Evergreen State College, Olympia, WA 98505 - Nov. 15, 1997 rar .