What it is
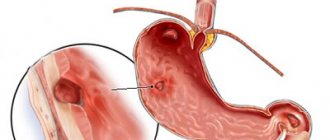
Antral gastritis is an inflammation of the gastric mucosa in its lower section, near the transition to the duodenum. In this case, the damage is superficial. Therefore, endoscopic examination of the stomach (FGDS) usually reveals catarrhal forms without erosions, hemorrhages and ulcers. There is a special type of this pathology associated with the reflux of the contents of the duodenum into the stomach (duodeno-gastric reflux).
Among all forms of inflammatory diseases of the stomach, chronic antral gastritis accounts for more than 75% of cases and occurs in almost half of the adult population. According to ICD-10, the disease has code K29.3.
Gastritis of the antrum is characterized by a long course, while atrophic forms of the disease do not develop, but concomitant duodenitis is possible. The lesion is widespread; focal changes in the antrum are uncharacteristic.
Chronic gastritis - symptoms and treatment
Currently there is no generally accepted classification of the disease. In clinical practice in the Russian Federation, the working classification created on the basis of the classification of S.M. is most often used. Ryss and the Houston modification of the Sydney HG classification. It is compiled with the inclusion of clinical and functional sections, with their designation (in the spirit of the Sydney system) by the grammatical terms “inflection” (ending). The group of hCG type C also includes medicinal and professional forms of hCG.[7]
Working classification of CG
By etiology and pathogenesis (prefix):
- CG type A: autoimmune fundic atrophic, including those associated with megaloblastic Addison-Birmer anemia;
- CG type B: bacterial antral nonatrophic, associated with HP infection;
- CG type AB: combined atrophic pangastritis (with damage to all parts of the stomach).
According to topographic and morphological features (root or core):
- by localization:
- fundic hCG (type A);
- antral hCG (type B);
- pangastritis (type AB) with predominant damage to the antrum or fundus;
- according to morphological criteria:
- superficial CG;
- interstitial hCG;
- atrophic CG with mild, moderate or severe atrophy;
- CG with intestinal metaplasia (complete or incomplete, small intestinal or colonic).
According to specific morphological characteristics (suffix):
- according to the severity of the inflammatory process in the gastric mucosa:
- minimum;
- minor;
- moderate;
- pronounced (depending on the degree of lymphoplasmacytic inflammatory infiltration of the gastric mucosa);
- according to hCG activity:
- no activity;
- light (I);
- medium (II);
- ▪ high (III) (depends on the presence and severity of the neutrophilic - granulocytic component in the inflammatory infiltration of the gastric mucosa);
- according to the presence and severity of contamination of the coolant with HP infection:
- absent;
- light (I);
- medium (II);
- high (III);
According to clinical features:
- CG (type B) with a predominance of pain syndrome (Gastritis dolorosa);
- CG (type A) with a predominance of dyspeptic symptoms;
- CG with a latent (asymptomatic) course (~50%).
According to functional criteria (flexion), the following forms of chronic gastritis :
- HCG with preserved (and increased) secretion;
- CG with secretory insufficiency (moderate, severe, total).
Endoscopic criteria for hCG:
- erythematous (exudative) superficial CG;
- CG with flat (sharp) erosions;
- CG with rising (chronic) erosions;
- hemorrhagic hCG;
- hyperplastic hCG;
- HCG complicated by GDR (reflux gastritis).
When formulating a diagnosis, the following algorithm is used: Prefix (etiology) - Root (localization) - Suffix (morphology) - Inflection (function) with the addition of endoscopic criteria.
Example of diagnosis: Chronic Helicobacter gastritis of the antrum of the stomach with moderate inflammation, moderate activity, high contamination with Helicobacter pylorus with preserved secretion.
Due to the greater availability of morphological assessment of the condition of the gastric mucosa based on the results of studies of biopsy material, the CG classification according to the OLGA (Operative Link for Gastritis Assessment) system is increasingly being used. Over time, the morphological classification of CG will become the leading one in the world.
CG, like all chronic diseases, has two stages: exacerbations and remissions, which successively replace each other. With each exacerbation, greater structural changes occur in the mucosa. Exacerbation and remission of hCG can be confirmed clinically or endoscopically (the most accurate confirmation is based on the results of endoscopy and the morphology of the biopsy material).
Based on the cause of occurrence, the following types of chronic gastritis : caused by Helicobacter Pylori infection, drug-induced and autoimmune atrophic gastritis.
Caused by Helicobacter Pylori infection (HP infection)
Currently, HP infection (type B gastritis) plays a leading role in the development of CG. The majority of adults over 60 years of age are infected with this bacterium. In Russia, among children over 5 years old, 30% are infected, at the age of 15-20 years - 63%, adults - more than 85% [10]. The pathogenesis of the effect of this pathogen on the stomach is that chronic Helicobacter Pylori infection causes changes in the tissues of the gastric mucosa. For a long time, the infection occurs without symptoms. As inflammation spreads to the body of the stomach and the response of the mucous membrane increases, the first symptoms of gastritis appear. The longer the infection lasts, the stronger the restructuring of the mucous membrane. This restructuring of the mucosa consistently leads to atrophy, intestinal metaplasia and dysplasia, leading to gastric cancer. The development of gastric atrophy is a critical step in the transition of hCG to gastric cancer.
Drug-induced gastritis (type C)
This is the second most common form of gastritis. The effect on the stomach of non-steroidal anti-inflammatory drugs (NSAIDs) has been most studied. They do not cause direct aggressive action, like acids (hydrochloric acid is tens of times more aggressive). The pathogenesis of their effect on the gastric mucosa is based on the blocking of cyclooxygenase enzymes (isomers COX-1 and COX-2). When COX-1 is blocked, the synthesis of prostaglandins (E2 and I2) is suppressed, which ensure the quality and strength of the mucosal barrier that protects the mucous membrane from the aggressive effects of hydrochloric acid and pepsin. Therefore, long-term use of NSAIDs leads to a thinning of the protective layer of mucus and an increase in the aggressive effect of hydrochloric acid on the gastric mucosa, causing chronic inflammation.
Autoimmune atrophic gastritis (type A gastritis)
The rarest form of hCG is autoimmune atrophic gastritis (type A gastritis). Until now, its etiology is not known. It is based on the production of antibodies by immune cells to the parietal cells of the mucous membrane (synthesize hydrochloric acid) and the internal factor of Castle (participates in the absorption of iron in the intestine). As a result of this, inflammatory changes develop, very early leading to atrophy and achlorhydria (a condition in which there is no hydrochloric acid in the gastric juice). The metabolism of vitamin B12 is also disrupted, aggravating the course of anemia.
In addition to those listed, there is a group of specific types of chronic gastritis.
Radiation gastritis - the causative factor is ionizing radiation, which has both a direct damaging effect on the mucous membrane and through a cascade of reactions with the formation of free radicals and lipid peroxidation of cell membranes. As a result, with prolonged exposure to doses of ionizing radiation exceeding the maximum threshold, chronic radiation gastritis develops.
Lymphocytic gastritis is characterized by specific inflammation in the gastric mucosa, which develops against the background of gluten enteropathy - celiac disease (a pathological disorder of the intestines in which gluten intolerance occurs). The mucous membrane is damaged by its own antibodies with the development of chronic inflammation.
Granulomatous gastritis develops as a result of the involvement of the stomach in the inflammatory process in Crohn's disease (chronic inflammatory bowel disease) and occurs with similar mucosal lesions in the form of erosions and ulcers. Specific foci of chronic inflammation, granulomas, form in the mucosa.
Eosinophilic chronic gastritis develops with food allergies. If you do not follow a diet that excludes the allergen, chronic inflammation develops in the gastric mucosa. The more often allergens enter the stomach, the more pronounced the manifestations of gastritis.
The course of chronic gastritis
CG is a long-term disease: on average, 18-25 years pass before the development of pronounced structural changes in the gastric mucosa in the form of atrophy, dystrophy or dysplasia. Over time, each exacerbation leads to the spread of the inflammatory process not only over the area (breadth), but also into the depth of the mucous membrane. When the body and fundus of the stomach are involved in the process, the production of hydrochloric acid and pepsin begins to decrease, which leads to digestive disorders.
Symptoms
Antral gastritis is accompanied by minor complaints or manifests itself in various variants of dyspepsia - digestive disorders:
- ulcer-like dyspepsia – dull pain in the upper abdomen, heartburn;
- dyskinetic variant of gastric dyspepsia - nausea, rapid satiety, bloating after eating.
As the pathology progresses, the pain syndrome intensifies. The pain becomes cramping, aching, sucking, and can bother you on an empty stomach and at night. It is accompanied by belching, a burning sensation in the chest, often reminiscent of an angina attack.
When you feel (palpate) the abdomen, you can determine moderate pain in the upper abdominal cavity and its swelling. With a chronic course of the process, weight loss, sleep disturbances, and irritability are possible.
Topography of gastritis
There are three histological zones in the stomach, the difference of which is based on the type of glands: cardiac, acid-producing (fundic) and antral.
The mucosa at the border of these zones may contain a mixture of two adjacent types of mucosa for several centimeters. The topographic distribution of gastritis is often related to the type of glands. Cardia.
The mucous membrane of the cardia occupies only a few centimeters below the gastroesophageal junction.
Its glands are mainly mucous, similar to the antrum glands. Inflammation of the cardia region (“carditis”) was largely ignored until recently; scientific interest in this area has now arisen. One reason for this is the dramatic increase in cardia cancer in Western countries and the possibility that cardia cancer may develop from intestinal metaplasia at the junction of squamous and columnar epithelium. It is possible that this intestinal metaplasia is a consequence of gastroesophageal reflux disease in some patients. A second reason for interest in "carditis
" is that biopsy in this area may be more sensitive than squamous epithelial biopsy in diagnosing patients with atypical symptoms of gastroesophageal reflux disease.
Acid-producing department.
The acid-producing mucosa occupies the fundus and body of the stomach (the upper three-quarters of the stomach). Acid-producing glands consist of parietal cells that produce acid and intrinsic factor and chief cells that secrete pepsinogen.
Antral region.
The antral mucosa occupies the distal quarter of the stomach and is limited by the angle of the stomach proximally and the pylorus distally. It contains mucous cells and gastrin-producing cells.
Treatment
For treatment of antral gastritis to be effective, it is necessary to undergo a course of therapy under the supervision of a therapist or gastroenterologist. It begins after an examination, which usually includes an FGDS, a biopsy and a rapid urease test to detect Helicobacter pylori.
Treatment includes a diet enriched with proteins. Vermicelli, milk, cereals, omelettes, vegetable purees, salads are useful. Rich soups, tough meat, fresh baked goods, spices, smoked meats, marinades, coarse fiber, chocolate, tea, coffee are limited.
Diet alone is not enough for complete recovery.
Along with proper nutrition, patients with antral gastritis are prescribed:
- antibacterial agents in various combinations for a course of 10 or 14 days;
- drugs that reduce the intensity of gastric secretion;
- medications to reduce gastric acidity.
Risk factors for the occurrence of Antral gastritis are eliminated, and if necessary, enzyme therapy is prescribed, for example, the drug Mikrasim®, which improves digestion.
Important: before use, read the instructions or consult your doctor.
Treatment of erosive gastritis
Treatment of erosive gastritis is carried out in a hospital setting. In most cases, patients can be cured. An important role in this matter is played by timely consultation with a doctor, correct diagnosis and adequate treatment.
There can be no talk of any self-medication. Only a doctor, based on a complete medical history, will be able to select the appropriate medications. A proper diet and a balanced menu are an important component of treatment for gastritis. Indeed, often the disease itself occurs precisely as a result of nutritional disorders. Avoid fried, salty and spicy foods. Eat little and often, chewing your food thoroughly. Food should not be too hot or too cold.
Nonerosive gastritis
The diagnosis of non-erosive gastritis is made on the basis of histology; the endoscopic picture cannot accurately predict whether there is inflammation of the mucous membrane. The most common type of nonerosive gastritis is HP associated gastritis. HP associated gastritis is considered here as a nonspecific type because its finding does not predict which associated disorder is present. For example, a patient with HP gastritis may have an associated duodenal or gastric ulcer or may be one of the main completely asymptomatic group of patients. The main causes or types of non-erosive gastritis are HP, pernicytous anemia, lymphocytic gastritis or reactive gastropathy.