Treatment of hiatal hernia under the guidance of Doctor of Medical Sciences, Professor Mikhail Andreevich Agapov, at the University Clinic of the Moscow State University named after M.V. Lomonosov
Author:
- Agapov Mikhail Andreevich Head of the surgical department, surgeon, oncologist, coloproctologist
4 (Votes: 9)
What is a hiatal hernia?
Hiatal hernia
is a pathology in which the internal organs, which are physiologically located under the diaphragm, are displaced into the chest cavity.
Modern medicine notes a trend toward an increase in the number of gastroenterological pathologies. Along with gastritis and peptic ulcers, a hiatal hernia (HH) is often diagnosed, treatment of which is necessary to prevent life-threatening complications. The appearance of the hiatal hernia is considered as an exclusively surgical disease, since there is a change in the diaphragmatic ligaments, muscle stretching and expansion of the lumen of the diaphragm, which are most optimally eliminated surgically.
A hiatal hernia is when part of the stomach or part of the intestine gets into an overly enlarged hole in the diaphragm. The disease is common and causes patients a lot of pain and difficulty eating. Acquired hiatal hernias (HHH) appear more often in women, the risk of their occurrence increases significantly after 50 years (from 0.7% at an earlier age to 4.7% after reaching 50-60 years). Irregular symptoms of a hiatal hernia can be eliminated with medications and a certain diet. If a hernia in the esophagus begins to constantly make itself felt with heartburn, pain, reflux (reflux of food from the stomach), then the most effective treatment in such a situation is surgery. Proper surgical treatment will relieve the patient of the signs of a hiatal hernia without the need for additional medications.
Basic principles of physical therapy for spinal hernia
Physical therapy for the occurrence of a herniated disc is one of the main methods of therapy. It relieves pain, helps strengthen the muscle corset, returns the spine to its natural position, and improves blood circulation. Such a complex, as a rule, consists of simple exercises such as flexion, extension and extension of the spine.
Before starting exercise therapy, you should consult your doctor. He will help you select the types of exercises and adjust the number of repetitions, taking into account the current condition of the patient and the characteristics of his illness.
At the initial stage, you should perform only those tasks in which the movements of the vertebrae are minimal. Try to avoid sharpness, do not bend deeply, protect your back from shocks and blows.
It is necessary to increase the intensity, quantity and duration of exercises gradually, as you feel better and strengthen your muscle corset. This takes time. It is impossible to restore muscle functionality in a few days. Prepare yourself for long work. The first positive changes should appear after a few weeks of regular exercise therapy.
Exercise therapy necessarily provides for preliminary preparation of the body, namely:
- Normalization of breathing.
- Warming up the muscles.
Allow at least half an hour for classes. It is best to distribute the set of exercises throughout the day so as not to overload the sore lower back.
Causes of development of hiatal hernia disease
The esophagus has the shape of an elastic tube and consists of several layers (mucous, muscular and serous membranes). It is located mostly in the chest cavity. Passing between the lungs, large blood vessels and the heart, the esophagus enters the abdominal cavity through the esophageal hiatus in the diaphragm. The chest and abdominal cavities are separated from each other by a muscular horizontal septum (diaphragm), through which the esophagus passes. The normal dimensions of the opening in the diaphragm correspond exactly to the diameter of the passing esophagus, no more and no less. When the diameter of the hole changes, problems begin, one of which is called a hernia in the esophagus.
This phenomenon is quite common, but at small sizes it does not cause any particular problems and can only be noticed during a targeted examination. Medium and large hernias lead to the reflux of aggressive gastric juice into the esophagus and the appearance of clinical symptoms.
The most common causes of acquired hiatal hernia:
- Consequences of injuries to the thoracic and abdominal organs;
- Constant increase in intra-abdominal pressure, due to ascites (fluid in the abdominal cavity); with multiple or repeat pregnancies, chronic constipation, intense physical activity, due to frequent persistent cough (for example, with COPD - chronic obstructive pulmonary disease);
- Age-related decrease in tone (weakening) of the esophageal ligaments (the condition is more common in patients over 50 years old);
- Significant, sharp weight loss, disappearance of adipose tissue under the diaphragm;
- Previous operations on the esophagus;
- Obesity;
- Poor physical shape and tone of the diaphragmatic ligaments;
- Disturbances in the passage of food through the esophagus (esophageal motility disorders);
- Chronic diseases of the stomach, gall bladder, small intestine, leading to disruption of their motility (a situation where the normal contraction of organs and the process of passing food through them is disrupted) - often peptic ulcer of the stomach and duodenum, cholecystitis, pancreatitis.
Congenital hiatal hernia occurs in children with too short an esophagus, when the stomach (or part of it) is located abnormally high (in the chest cavity) due to insufficient length of the esophageal tube.
Physical therapy for spinal hernia using Bubnovsky’s method
The main distinguishing feature of Bubnovsky’s exercises from conventional physical therapy is the load on the muscles through pain. In his opinion, it is necessary to fight pathology by overcoming the pain threshold, since it is this symptom that limits movement and causes muscle atrophy. Classes using the Bubnovsky system prevent the development of a hernia and reduce its size. This method is also called kinesitherapy.
The effectiveness of physical therapy according to the Bubnovsky system largely depends on the fulfillment of the following requirements. Necessary:
- Maintain proper breathing.
- Stretch your muscles and spine.
- Complete absence of drug treatment.
- Strengthen the muscle frame.
The impact should be on all muscles of the body, and especially on those that are subject to stress in everyday life.
The basic complex includes the following exercises:
- In yoga it is called “Cat”. Get on all fours, focusing on your palms and knees. Inhale and arch your back. Exhaling, bend in the opposite direction. Hold the pose for two to three seconds and return to the starting position. Repeat 10–20 times. Perform movements smoothly and slowly.
- Walking on your buttocks. Sit on the floor, keep your legs and back straight, arms at chest level. Walk forward using your butt muscles and come back. Perform 8–10 reps.
- "Bike". Starting position – lying on your back. Bend both legs at the knees and alternate your feet in a circle in the air (in other words, move as if you were riding a bicycle). Do the exercise for one minute.
- Side bends. Stand straight, feet shoulder-width apart, hands on your waist. As you inhale, bend to the right (do not bend your back), while exhaling, return to the starting position. Repeat the movement to the left. Perform the exercise ten times on each side.
- "Bridge". Lie on your back. Inhale deeply and, as you exhale, bend, rising on your arms and legs to the maximum possible height. Hold the pose for three to five seconds. Do five reps.
Nowadays, you no longer have to spend a lot of time performing complex and unpleasant procedures at home. It is much easier to seek help from real professionals - the Veronika Herba beauty and health center, equipped with effective and modern equipment.
Why clients choose Veronika Herba Beauty and Health Center:
- This is a beauty center where you can take care of yourself at a reasonable cost, while your face and/or body will be treated not by an ordinary cosmetologist, but by one of the best dermatologists in Moscow. This is a completely different, higher level of service!
- You can receive qualified help at any time convenient for you. The beauty center is open from 9:00 to 21:00, seven days a week. The main thing is to agree with your doctor in advance on the date and time of your appointment.
Sign up for a consultation with a specialist by phone +7 (495) 085-15-13
, and you will see for yourself!
Esophageal hernia: symptoms and causes of their appearance
There are asymptomatic hiatal hernias, which can only be identified through instrumental studies. They are usually discovered by chance. But more often the disease makes itself felt by one or more signs with varying degrees of severity.
- Heartburn
The main reason for its occurrence is compression of the stomach or intestines in the diaphragmatic opening. Intragastric pressure increases, and food is thrown back into the esophagus. The condition is called gastroesophageal reflux disease (GERD). Food from the stomach contains a lot of gastric juice (acid), which irritates the mucous membrane of the esophagus and causes a burning sensation (heartburn).
- Belching
Belching air or acidic contents from the stomach (regurgitation). Hiatal Hernia (HH): The symptom of belching occurs for the same reasons as heartburn. The symptom is quite common, noted in 70% of cases.
- Pain
The nature and intensity of pain can be different: from aching, limited pain behind the sternum, to sharp, burning, stabbing pain of a girdling, diffuse nature. Pain occurs due to irritation of the esophageal mucosa by acidic food entering there from the stomach. Pain can also appear due to compression of the vagus nerves in the esophageal opening of the diaphragm. The anterior branches of which pass from the chest to the abdominal cavity along with the esophagus. Often, painful signs of a hiatal hernia are mistaken for heart pain (for example, confused with angina or even myocardial infarction). Pain accompanies half of patients with hiatal hernia; in time it is associated with eating, the patient remaining in a horizontal position or bending forward.
- Swallowing difficulty (dysphagia)
Patients are concerned about difficulty after swallowing food, a feeling of “lump” appears behind the sternum after eating (especially after eating too hot, cold or too much). Sometimes there is a paradoxical situation when solid food in a patient with hiatal hernia (hiatal hernia) passes more easily than liquid food. However, as the disease worsens, dysphagia appears even when eating food of any consistency and temperature.
- Tongue pain (glossalgia)
- Hoarseness of voice
The last 2 symptoms appear due to peptic burn (stomach acid burn) of the oral mucosa, tongue and larynx.
- Hiccups
- Heart rhythm disturbances
- Dry cough
- Attacks of suffocation similar to those of bronchial asthma
The group of the 4 symptoms listed above occurs due to the “fault” of the vagus nerve, which is compressed together with the esophagus in the opening of the diaphragm.
Swimming with a hernia of the lumbar spine
Many doctors agree that swimming is one of the most effective and least traumatic types of physical activity. Classes affect the maximum number of organs and tissues. During swimming, an even load is created on all the muscles of the body. Regular exercises help get rid of the pain syndrome that occurs with spasms, as well as minimize the risk of relapses.
Under the influence of water, painless stretching occurs in the affected area of the spine, which eliminates various types of displacement, indentation, and pinching in the intervertebral area.
It is for this reason that many patients who choose swimming as exercise therapy easily reduce the daily dosage of medications (mainly painkillers). This type of activity improves the overall emotional background due to the release of endorphins.
Like any physical therapy exercise, swimming has its limitations, contraindications and recommendations:
- You should not swim during an exacerbation of the pain syndrome, as even careful movements can cause harm. You should start only after a long remission, after consultation with a specialist in the field of neurology and under the supervision of a qualified trainer.
- The training program should be developed together with the attending physician, since it is necessary to take into account many factors, for example, how strong the hernia is, how quickly it develops, and what other diseases the patient has. Regular sport swimming puts excessive stress on the spine, so its volume and type must be selected individually.
- Preference should be given to backstroke and freestyle swimming, as they are the most effective and safe. It is these styles that train the lower back muscles, but do not put pressure on the intervertebral discs.
- Do not forget that, first of all, you need to listen to your body and if the slightest pain or discomfort occurs, you should abandon the movements that cause them. If a pain attack occurs while swimming, you must stop immediately.
- Many pools have a special system that simulates a whirlpool. This massage has a good effect on the muscles, relaxes and tones them at the same time.
- Classes should be systematic, and one session should last about an hour.
- The water temperature in the pool should be comfortable, especially during the first sessions. The ideal value is around thirty degrees. In the future, it will be possible to gradually lower the temperature to +23 °C so as not to irritate the body.
- Proper breathing during therapeutic swimming has a beneficial effect on blood circulation. Inhale deeply and exhale quickly.
One of the prerequisites for the occurrence of a hernia of the lumbar or sacral spine is osteochondrosis. It is observed in the vast majority of patients with lumbar hernia. Therefore, the swimming style should be selected based on the characteristics of osteochondrosis and other pathological processes:
- If there is a flattened curve of the ridge in the sternum area, it is necessary to swim on your back. In this position, she regains her physiological forms. If you swim on your stomach with this pathology, the condition can only worsen.
- If the back is too arched back, swimming on the back is contraindicated. After all, it loads the muscles of the shoulder girdle, and as a result the spine is even more rounded. That's why we swim only on our chest.
- For patients with low immunity, in years, with weakened muscles, movements with a large amplitude, such as in the crawl, are contraindicated.
If, after a doctor’s examination, no pathologies are found, the patient is prescribed a treatment complex containing the following tasks:
- Take a swimming board, sit comfortably on it and repeat the dolphin style with your feet at a distance of 100 m.
- Lie on your back and swim 400 m while moving your arms.
- Stay in this position and swim 250 m, alternately moving your arms.
- Swim crawl 150 m.
- Finish with a gentle 100m breaststroke.
Read material on the topic:
Manual therapy of the cervical spine as a worthy replacement for alternative treatment
Types of hernias UNDER
- Sliding. Another name – floating hiatal hernia – reflects the essence of the disease. The stomach, intestines or omentum enter the chest cavity periodically (freely passing back and forth). Manifestations of the disease may at times be absent and appear spontaneously when food refluxes from the stomach into the esophagus. Typically, heartburn, belching, and pain are a concern. How to relieve pain from a hiatal hernia (sliding)? Taking antacids (acid-reducing agents – Maalox, Smecta, Rennie, Almagel, etc.) helps;
- Paraesophageal (paraesophageal). Constantly located on the side of the esophagus in the chest cavity is the upper part of the stomach. The food that gets there stagnates, causing patients an extremely unpleasant, bursting sensation in the chest after eating. Therefore, they first try to eat less, and then they may even refuse to eat (for fear of pain). This behavior leads to exhaustion of the patient;
- Complicated hernias. The most dangerous thing is a strangulated hernia. The hernial sac becomes motionless in the hole, its contents cannot be evacuated. Signs of intoxication appear (high temperature, pallor, weakness, increased pulse and heart rate), vomiting of undigested food, bile and even blood. There is a high probability of rupture of the hernial sac, which can lead to mediastinitis or peritonitis, and then sepsis. Less serious complications are anemia, bleeding from the esophagus, gastritis and stomach ulcers (where it enters the hernial sac), prolapse of the stomach into the esophagus (prolapse).
It is precisely because of the risk of complications that patients need a thorough examination and decision on the issue of surgical treatment of hernia.
Dikul exercises for spinal hernia
Dikul’s set of physical therapy exercises belongs to kinesitherapy, the founder of which is considered to be Doctor of Medical Sciences S. M. Bubnovsky. The program was developed, one might say, from our own experience. At the age of 15, Valentin Dikul received a severe spinal cord injury as a result of multiple local injuries and a compression fracture of the spine. Doctors did not give any positive prognosis or prospects for recovery. But thanks to his own technique, Dikul was able to completely restore all functions of the spinal cord and return to his normal life. Its complex makes it possible to get rid of pain and cure pathology.
In the process of treating patients with intervertebral hernias, special simulators are used, personally developed by Valentin Ivanovich. The training program is selected individually for each patient. Before starting training, exercises are discussed with your doctor and possible contraindications are identified.
The complex for the lumbar spine, which Dikul proposed, helps solve several problems at once:
- strengthens the muscle corset, forms correct posture;
- reduces pain syndromes of paravertebral muscles and spinal cord nerves;
- eliminates muscle spasms and swelling;
- normalizes blood circulation and lymph movement in lymphatic vessels;
- works the deep-lying paravertebral muscles and restores normal muscle tension.
Valentin Dikul is sure: for classes to be effective, it is necessary to strictly follow the rules that he prepared for stable development of neurophysiological indicators and better adaptation of the body to new loads.
These rules read:
- Never change the sequence of exercises in the treatment complex on your own. This order must always be maintained.
- Classes should be regular, three to four times a week for 40–50 minutes. If training has stopped for any reason, then it is necessary to start it from the first stage, since muscle tissue very quickly adapts to the intensity of the current load.
- A set of exercises should be selected in consultation with a specialist.
- Gradually increase the load as the spinal muscles strengthen.
- Focus on your feelings during physical therapy exercises. If you experience discomfort, then you should stop training.
The duration of treatment depends on factors such as the condition of the muscles and the severity of the disease.
The Dikul training complex includes three stages:
- First, it is necessary to prepare for stress, especially for those patients who lead a sedentary lifestyle and have weakened muscles.
- The second stage is aimed at strengthening joints and ligaments.
- The third includes a therapeutic set of exercises to develop flexibility, mobility, and strengthen the spine.
The starting position for the main part of the exercises is lying on your back, on a hard surface. Some tasks may require additional equipment to complete. Physical therapy for lumbar spinal hernia includes exercises such as:
- Start with a warm-up to warm up your muscles (smooth stretches, turns, bends).
- Lie on your back. Cross your arms at the chest area. Take ten incremental steps, first to the left, then to the right. Make sure your legs and upper torso do not leave the floor.
- The starting position remains the same. Perform ten bends in each direction, sliding along the floor. The lower part of the body should remain motionless.
- The starting position is the same, bend your legs. Slowly draw your knees towards your sternum. Perform 7–10 times.
- Starting position – standing. Lower your hands, take a gymnastic stick. Keeping your back straight, bend down 7-10 times. For convenience, your legs need to be slightly bent.
- Take a rubber band in your left hand and secure the end of the projectile with your foot under your toe. Make five slow bends to the right. The patient must overcome the resistance of the elastic material. In this case, the right hand should be placed on the back of the head. Repeat to the left five times.
Read the material on the topic: MRI of the shoulder joint: indications and contraindications for its implementation
Treatment of hiatal hernia
There is a common belief that patients diagnosed with hiatal hernia mainly suffer from gastroesophageal reflux, and this is indeed the case. Gastroesophageal reflux disease (GERD) is a disease accompanied by the reflux of acidic, aggressive stomach contents into the esophagus. Today, GERD is recognized as a disease of the 21st century, which is confirmed by its high prevalence along with other diseases of the gastrointestinal tract. The main symptom of this disease is heartburn, which is detected in our country and other countries in 40% of the population. The causes of this disease may coincide with the causes of hiatal hernia. The danger of these diseases lies not only in discomfort and pain, but also in constant inflammation of the mucous membrane of the esophagus, which can ultimately lead to erosive esophagitis, Barrett's esophagus, and esophageal cancer.
The conservative treatment method is used after consultation with a gastroenterologist and surgeon and after all necessary examinations. In addition to examination and questioning, this is an FGDS (fibrogastroduodenoscopy, examination of the esophagus and stomach from the inside with a special instrument). X-ray examination (survey images and images after taking a barium suspension). pH-metry of the esophagus and stomach (study of the acidity level of their contents). Esophagogododenometry (measurement of pressure inside the esophagus and stomach).
Esophageal hernia, how to cure it with medications. Treatment without surgery can be carried out for small hernias, uncomplicated and not accompanied by pronounced symptoms. The goal of treatment is to reduce the intensity of symptoms and avoid the risk of disease progression. It is impossible to eliminate a defect in the diaphragm using therapeutic methods. Treatment begins with lifestyle and nutrition correction. It is necessary to eliminate the factors leading to increased intra-abdominal pressure: lose weight, treat chronic diseases, quit smoking and other bad habits, strictly follow a diet. It is mandatory to prescribe pharmaceuticals that reduce the acidity of the stomach (antacids) and agents that protect the mucous membrane of the esophagus and stomach from the aggressive effects of acidic contents (gastroprotectors),
Recommendations for hiatus hernia
- eat small meals several times a day;
- eat food 2-3 hours before bedtime;
- eat food of gentle temperature and consistency (chopped, pureed);
- if you have symptoms, avoid eating chocolate, onions, citrus fruits, tomatoes, spicy foods and other foods that cause heartburn;
- eliminate alcohol consumption;
- stop smoking!;
- normalize weight;
- sleep with the head of the bed raised 15 cm.
For patients with a hiatal hernia, there are a lot of taboos: you can’t eat fried, salty, smoked, carbonated drinks, spicy food, fast food, alcohol, smoked meats or sweets. In general, everything that stimulates increased production of digestive enzymes and can cause heartburn.
Surgical treatment of hiatal hernia
Surgery for a hiatal hernia is the main radical way to restore the correct anatomical relationship and location of organs and relieve the patient from the unpleasant symptoms of the disease.
Preoperative examination for hiatal hernia includes:
- conducting a general blood test;
- X-ray of the esophagus using barium fluid to ensure a clear silhouette of the esophagus and stomach;
- esophagogastroduodenoscopy, during which the upper part of the gastrointestinal tract is examined using an endoscope;
- esophagomanometry to measure pressure inside the esophagus and stomach.
In each specific case, taking into account concomitant diseases, the attending physician may prescribe additional tests and studies.
Now, in most cases, laparoscopic methods for correcting the esophageal opening of the diaphragm and the esophagogastric junction are the best choice.
Laparoscopic treatment of hiatal hernia has a number of advantages:
- Preservation of the natural anatomy of the thoracic cavity and upper abdominal cavity;
- Less traumatic;
- Fast patient recovery after surgery;
- No cosmetic defects after the intervention (no scars).
During the operation, surgeons see an image from the magnifying optics of the laparoscope on an external monitor. Magnification makes it possible to distinguish fine branches of nerves, fascial spaces and vessels. Mini-instruments inserted through small punctures carry out surgical treatment according to the chosen technique. It could be:
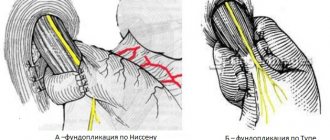
- Modification of the classic Nissen operation (fundoplication). When the lower part of the esophagus is strengthened with a kind of coupling (a cuff several centimeters wide, taken from the tissues of the fundus of the stomach and wrapped around the esophagus 360 degrees. After the operation, the frequency of reflux of food from the stomach is reduced, its motility is normalized, and the tone of the esophagus is strengthened.
- Toupet method. The difference between the method is the amount of coverage of the esophagus with a reinforcing cuff - 270 degrees instead of 360 according to the classical method. The advantages of this method: preservation of the natural mechanisms of belching and the ability to realize the gag reflex.
During the operation, the lower part of the esophagus and the fundus of the stomach are isolated from the adhesions, brought down into the abdominal cavity and fixed in an anatomically based position.
Then crurorrhaphy (reduction of the diaphragmatic opening) and fundoplication (strengthening the lower part of the esophagus with a cuff from stomach tissue) are performed. Sometimes the patient may undergo the Esophyx method of surgery. When there are no punctures, a flexible endoscope and the necessary instruments are inserted through the oral cavity into the esophagus. And they change the angle of the stomach to the esophagus to the correct value. Then the cuff strengthens the transition between the organs.
New laparoscopic surgical techniques have reduced the relapse rate to 3.5% over a five-year period. That is, almost 97 patients out of 100 after 5 years retain the positive effect of treatment, without additional use of medications.
There are different options for fundoplications. The type of operation is determined individually.
Antireflux surgical methods are aimed at eliminating the hernial orifice, forming a physiological mechanism that prevents stomach contents from entering the esophagus, and preventing displacement of the stomach and esophagus. Fundopletion is such an effective, recognized method. This operation has been performed since 1955 and is based on wrapping the fundus of the stomach around the esophagus 360 degrees. This creates a cuff that prevents gastric juice from refluxing into the esophagus. This operation has different execution options. Considering the presence of a large number of anatomical and physiological features in each patient, the cost of the operation is determined individually.
Laparoscopic surgery for hiatal hernia, laparoscopic surgery for cholecystitis (scientific Simultaneous surgery - laparoscopic fundoplication and laparoscopic cholecystectomy).
Contraindications to physical therapy
There are cases when physical therapy is contraindicated. Among them are:
- oncological diseases;
- stroke;
- pre-infarction condition;
- diseases accompanied by elevated body temperature;
- exacerbation of intervertebral hernia;
- hypertensive crisis;
- if a little time has passed since surgery.