Necrotizing enterocolitis of newborns
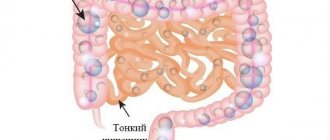
Necrotizing enterocolitis of newborns (NEC) is a serious intestinal disease that occurs against the background of acute hypoxia, disruption of normal colonization of the intestine by microflora, leading to necrosis and perforation of the intestinal wall, peritonitis. The incidence rate is 1 - 5 cases per 1000 live births. Premature babies and children with low birth weight are most often affected. Factors leading to the occurrence of NEC:
- Premature birth
- Acute hypoxia during labor
- Lung diseases
- Congenital heart defects
- Birth of twins
- Hemolytic disease of the newborn
- "Aggressive enteral feeding"
- Umbilical vein catheterization
- Anemia of newborns
- Cooling
- Mother's drug addiction
- Congenital malformations - Hirschsprung's disease, gastroschisis, intestinal obstruction.
Classification of NEC according to Bell (1978) as modified by Walsh and Kliegman (1987):
Stage I – initial manifestations: changes in the child’s behavior (excitability or lethargy), bloating, discharge through a gastric tube, stool retention. I a – occult blood in the stool I b – obvious blood in the stool
Stage II - the height of the disease: lethargy, hypotension, adynamia, changes in the frequency and depth of breathing, rapid heartbeat, increased bloating, lack of intestinal motility, stagnant discharge through the gastric tube, stool retention or an increase in pathological impurities (mucus, blood) in the stool. X-ray signs appear (pneumatosis of the intestinal walls), and ultrasonic signs (decreased peristalsis, swelling of the intestinal wall, the appearance of a static loop of intestine). II a – moderate course II b – severe course with symptoms of systemic intoxication III a – intestinal necrosis without perforation III b – intestinal perforation.
Stage III - development of complications: septic condition of the child, adynamia, severe water and electrolyte disturbances, microcirculation disorders, bleeding, tendency to thrombosis, tension and bloating, swelling and hyperemia of the anterior abdominal wall, contouring of the subcutaneous venous network, lack of intestinal motility. Ultrasound examination reveals the presence of free fluid in the abdominal cavity, gas in the portal system of the liver, identification of infiltrate in the abdominal cavity, necrotic intestines with depleted blood flow. The radiograph shows uneven swelling of the intestinal loops, free air in the abdominal cavity.
In the reversible stage of NEC, it is possible to cure the child without resorting to surgery. The child is not fed, a gastric tube is inserted, infusion therapy is carried out, antibiotics are prescribed, immunotherapy is carried out, and thrombus prevention is carried out.
In the case of a complicated course of NEC, surgical treatment is performed: laparoscopy, laparotomy, resection of the affected area of the intestine, formation of a primary anastomosis, and enterostomy.
In the postoperative period, the child requires intensive infusion and antibacterial therapy; after restoration of intestinal function, enteral feeding is carefully introduced.
The use of modern methods of diagnosis and treatment of NEC will reduce mortality in this pathology. Long-term complications of NEC include short bowel syndrome, intestinal stenosis, and malabsorption syndrome.
The quality of life of children who have had NEC is affected by concomitant pathology characteristic of premature infants: bronchopulmonary dysplasia, chronic lung diseases, consequences of perinatal damage to the central nervous system, retinopathy of prematurity, delayed physical and psychomotor development.
Causes
Despite the fact that enterocolitis most often occurs in premature babies, in particular those whose birth weight was less than 2 kg, the disease is infectious in nature and can manifest itself in a baby with normal parameters at birth.
It is not possible to name the exact causes of enterocolitis, but doctors identify several characteristic features :
- the woman was treated with antibiotics during the perinatal period;
- intrauterine or postpartum infection of the baby with parasites;
- violation of the vitamin and mineral composition in the mother’s body due to improperly selected nutrition;
- the composition of breast milk is pathologically harmful;
- intrauterine intestinal development disorder (a common occurrence, especially for those born with insufficient body weight);
- infections of staphylococcus, E. coli;
- trauma received during childbirth;
- postpartum complications (asphyxia, hypoxia and severe blood loss);
- incorrect or untimely attachment to the breast.
One of the subtypes is allergic enterocolitis, the main symptoms of which are:
- nausea;
- gagging;
- diarrhea (up to 10 times a day);
- in rare cases, severe pain is observed in the area of the small intestine.
Allergic enterocolitis can occur against the background of a reaction to certain types of pathogens - chicken egg white, which contains lysozyme, certain varieties of berries, and seafood.
Additionally, in patients with suspected allergic enterocolitis, the following was observed:
- iodine-containing medications,
- antibiotics,
- some types of sulfonamides.
The cause may also be poisoning with heavy metal salts, mushrooms, or medications. A pattern was revealed that most cases of the disease in newborns were associated with:
- the onset of labor before the due date;
- living conditions in a family with poor sanitary conditions;
- ignoring doctor's instructions and the presence of bad habits in the mother.
In addition to the main reasons , infants who have :
- an intestinal infection entered the body through the mouth (in such cases, salmonellosis, cholera, dysentery, shigellosis develop);
- infection with enterobiasis (pinworms) or ascariasis (roundworms) has occurred. This is typical for infants;
- the functioning of the pancreas, stomach or gallbladder is impaired;
- food allergies were identified, mainly to gluten and lactose.
On the mother's side, the reasons may be:
- unreasonable use of antibiotics, the intake of which, even in small doses, passes into breast milk;
- unsanitary conditions in the newborn's room, violation of hygiene rules for caring for the baby;
- infection by the staphylococcus virus during gestation;
- consumption of prohibited foods during breastfeeding;
- incorrect introduction of complementary foods.
Symptoms
In children under one year of age, enterocolitis tends to manifest itself in sudden attacks with acute pain, but it happens that the disease proceeds hidden, imperceptibly increasing pain in children.
The disease has the following manifestations:
- frequent and profuse regurgitation;
- frequent loose stools (diarrhea);
- bloody clots in the stool of newborns;
- bloating;
- increased flatulence;
- deterioration of the baby’s general condition (motor activity decreases);
- frequent bowel movements;
- muscle pain and cramps (due to dehydration and loss of chlorides);
- high fever that does not go away within 2 weeks.
The most dangerous is infectious enterocolitis, which is manifested by a sharp increase in body temperature. Most often, this means that an infection has entered the intestines or there has been a case of secondary infection of an already damaged area of the intestine.
In addition to the described symptoms, the following is observed:
- lethargic behavior of the newborn;
- constant drowsiness;
- decreased appetite;
- causeless whims.
In cases of the disease in newborns, the disease is most often necrotic in nature . The risk group of children who may develop necrotizing enterocolitis includes:
- newborns born prematurely;
- full-term infants with abnormalities of intrauterine development;
- babies with birth injuries (cerebral hypoxia, ischemia and heart disease).
If you suspect enterocolitis in a newborn, you need to know in what cases you need to seek emergency medical help :
- the baby is under 1 year old;
- in 12 hours, the child experienced diarrhea up to 10 times;
- temperature rise above 38 degrees;
- feces mixed with blood streaks;
- loss of skin elasticity due to the general weakness of the baby.
The main thing to remember is that after calling an ambulance, you must constantly replenish the baby’s fluid loss with the help of oral hydrants . Otherwise, dehydration, especially in small children, can lead to death. Giving medications is not recommended, since medications can “lubricate” existing symptoms.
Possible consequences
The prognosis of the disease depends on its causes and timely initiation of therapy. Prevention consists of preventing and treating intestinal infections . Correct lifestyle and diet play a big role in further prevention.
Despite the overall favorable prognosis, if not treated in a timely manner, enterocolitis can cause the following complications:
- development of necrotizing enterocolitis;
- pathogens can spread to other organs and cause, for example, meningitis or pneumonia;
- development of pseudomembranous enterocolitis (characterized by the complete absence of bacteria in the intestines).
Treatment
Therapeutic measures are based on restoring the functioning of the gastrointestinal tract . Treatment prevents the development of exacerbation and also prevents its transition to a chronic form.
Newborns and babies up to one year old are required to be put on a strict diet , and also undergo a course of drug treatment, which includes:
- antimicrobials;
- antiviral;
- vitamin complexes;
- enzymes;
- anti-inflammatory agents.
In cases where the cause of the disease is ascariasis or helminthiasis parasites, first of all, therapy is carried out using antiparasitic drugs. Young patients are shown bed rest and diet No. 4 (after improvement - No. 4B).
Therapy for breastfed children
Therapy for enterocolitis in infants has its own characteristics . First of all, children are prescribed a strict diet. In an infant, symptoms and treatment are directly related: the more acutely a particular symptom of the disease manifests itself, the more targeted the treatment.
In cases where the development of acute enterocolitis is observed in infants, first of all, gastric lavage is performed. Only after this is a diet based on tea and/or water prescribed. Such children are sent to an infectious diseases hospital.
After the end of the diet, the baby can be returned to the previous diet . At first, he needs to be fed frequently and preferably with breast milk. If a woman cannot continue breastfeeding, doctors may prescribe a medicinal formula for artificial feeding.
Important! Infants with a chronic form of the disease are prescribed treatment with probiotics and pribiotics, as well as lactobacilli and sorbents in moderation. In cases of chronic obstruction of feces, the baby is prescribed laxatives.
Treatment of chronic enterocolitis is carried out over a long period of time and in stages. In most cases, treatment lasts from 6 to 10 months, but improvements are obvious as early as 3-4 weeks.
It is worth remembering that even after a significant improvement in the patient’s condition, it is not recommended to suspend the course of treatment , as this may provoke a relapse of the disease.
Children at the common table should be limited in their consumption of:
- spicy, salty and sour;
- cow's milk;
- fatty fish and meat;
- honey;
- flour products.
Products that are allowed to be consumed for enterocolitis:
- soups with low-fat broth;
- cottage cheese, kefir;
- eggs (boiled);
- jelly;
- butter;
- lean fish;
- meatballs;
- baked vegetables and fruits.
Mothers of newborns should adhere to the above diet during breastfeeding.