| This article requires additional links for verification . |
| Sigmoidoscopy | |
| ICD-10-PC | 0DBN8ZX (with biopsy) |
| MeSH | D012812 |
| Code OPS-301 | 1-651 |
| MedlinePlus | 003885 |
| [edit in Wikidata] | |
Rigmoidoscopy
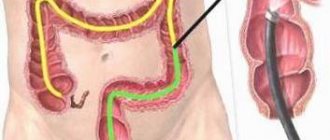
(from the Greek word "s/ς" + "eidos" + "scopy": namely, to look inside a "s"/"an"-like object) is a minimally invasive medical examination of the colon using the rectum through the proximal part colon, in the sigmoid colon.
There are two types of sigmoidoscopy: flexible sigmoidoscopy
, which uses a flexible endoscope, and
rigid sigmoidoscopy
, which uses a rigid device. Flexible sigmoidoscopy is usually the preferred procedure. Sigmoidoscopy is similar to, but different from, colonoscopy. Sigmoidoscopy examines only the sigmoid colon, the most distal part of the colon, while colonoscopy examines the entire colon.
Flexible sigmoidoscopy[edit]
A flexible sigmoidoscopy allows the doctor to look at the inside of the colon, from the rectum to the left side of the colon, called the sigmoid colon. Doctors may use this procedure to find the cause of diarrhea, abdominal pain, or constipation. They also use it to look for benign and malignant polyps, as well as early signs of cancer in the descending colon and rectum. [1] Using flexible sigmoidoscopy, the doctor can see intestinal bleeding, inflammation, abnormal growths, and ulcers in the descending colon and rectum. Flexible sigmoidoscopy is not sufficient to detect polyps or cancer in the ascending colon or transverse colon (two-thirds of the colon). However, although in absolute terms only a relatively small area of the colon can be examined by sigmoidoscopy, the areas observed represent the areas most commonly affected by diseases such as colorectal cancer, such as the rectum.
For the procedure, the patient must lie on his side on the examination table. The doctor inserts a short, flexible, lighted tube into the rectum and slowly inserts it into the colon. The tube is called a sigmoidoscope. The telescope provides an image of the inside of the rectum and colon, so the doctor can closely examine the lining of these organs. The scope also blows air into these organs, which inflates them so the doctor can see better.
If there is something unusual in the rectum or colon, such as a polyp or inflamed tissue, the doctor may remove part of it using instruments inserted into the endoscope. The doctor will send this piece of tissue (biopsy) to a laboratory for testing.
Possible complications of sigmoidoscopy are bleeding and puncture of the colon. However, such complications are rare.
Flexible sigmoidoscopy takes 10 to 20 minutes. During the procedure, the patient may feel pressure and mild cramping in the lower abdomen, but afterward the patient will feel better as the air leaves the colon.
One week before the procedure
Ask questions about your medications
You may need to stop taking certain medications before the procedure. Talk to your healthcare provider about which medications you can stop taking. Below are some common examples.
Anticoagulants (blood thinners)
If you are taking anticoagulants (medicines that affect blood clotting), ask your healthcare provider what is best for you. You may be told to stop taking this medicine; this decision will depend on the type of procedure and the reason you are taking anticoagulants.
Examples of blood thinning medications:
|
|
Do not stop taking your blood thinning medications without talking to one of your healthcare providers.
Medicines for diabetes
If you take insulin or other medications for diabetes, ask the healthcare professional who prescribed the medication what to do the morning of your procedure. You may need to change your dose before the procedure.
If you are taking metformin (such as Glucophage® or Glumetza®) or a medicine that contains metformin (such as Janumet®), do not take it one day before or on the day of your procedure.
If you are taking any other oral medications (medicines that you swallow) for diabetes, do not take them one day before or on the day of your procedure.
If you have an AICD, tell your healthcare provider.
Tell your Memorial Sloan Kettering (MSK) healthcare provider if you have an automatic implantable cardioverter-defibrillator (AICD). If you have an AICD, the procedure must be performed at Memorial Hospital (MSK's main hospital).
If necessary, obtain a certificate from your doctor
- If you have an automated implantable cardioverter defibrillator (AICD), you will need to get a clearance letter from your cardiologist (heart doctor) before having the procedure. A certificate of admission is a document that states that this procedure is safe for you.
- If you have had chest pain, dizziness, trouble breathing, or fainting in the last 6 weeks, you will need to be seen by your doctor and cleared for the procedure before your procedure.
A certificate of admission to the procedure must be submitted to the MSK doctor's office no later than 1 day before the procedure.
Arrange for someone to take you home
You must have a responsible companion to take you home after the procedure. A responsible companion is someone who will help you get home safely. This person should be able to contact your healthcare team if there are any concerns. Agree on this in advance, before the day of the procedure.
If you are unable to find a responsible escort to take you home, call one of the agencies below. You will be provided with an escort who will take you home. There is often a fee for these services and you will need to provide transportation. You can take a taxi or rent a car, but in this case you will still need to have a responsible escort with you.
| Agencies in New York | Agencies in New Jersey |
| Partners in Care: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
Buy everything you need
- 1 (10 oz [300 ml]) bottle of magnesium citrate (magnesium citrate)
- 1 saline enema (such as Fleet® enema)
- Clear liquids
- Vaseline® or A&D® Ointment
to come back to the beginning
Preparation[edit]
The colon and rectum must be completely empty for flexible sigmoidoscopy to be complete and safe, so the patient should only drink clear liquids for 12 to 24 hours. This includes broth or stock, gelatin, strained fruit juice, water, plain coffee, plain tea, or diet soft drinks. The night before or immediately before the procedure, the patient is given a laxative and an enema - a liquid solution that washes the intestines. Sedation is not required during this procedure unless the examination exceeds the level of the splenic flexure.
3 days before the procedure
The endoscopy nurse will call you between 8:00 am and 6:00 pm 3 days before your procedure. Your nurse will explain the instructions in this manual and ask you questions about your medical record. Your nurse will also review your medications and tell you which ones you should take the morning of your procedure.
Write them in the space provided for you below. ___________________________________________________
___________________________________________________
___________________________________________________
to come back to the beginning
Rigid sigmoidoscopy[edit]
Rigid sigmoidoscopy may be useful for anorectal conditions such as rectal bleeding or inflammatory rectal disease, especially in general practice and pediatrics.
To conduct the study, the patient must lie on his left side, in the so-called Sims position. The intestines are first emptied with a suppository and a digital rectal examination is first performed. The sigmoidoscope is lubricated and inserted with an obturator in the general direction of the navel. The direction is then reversed and the obturator is removed to allow the physician to penetrate further with direct vision. A bellows is used to blow air into the rectum. Lateral movements of the sigmoidoscope tip pass through the valve of Houston and the rectosigmoid junction.
Fecal occult blood test
The essence of this research method is to identify “hidden” blood in the stool, which is not visible during microscopic examination. The presence of hidden blood in the stool indicates the presence of bleeding from any part of the gastrointestinal tract.
A fecal occult blood test is indicated if there is a suspicion of bleeding from any part of the gastrointestinal tract, which can occur, for example, with bleeding polyps or colon cancer.
Preparing for analysis
Typically, medications (especially bismuth and iron preparations) should be discontinued a week before a stool occult blood test. In addition, it is not recommended to perform enemas, and at least 2 days should pass after X-ray examinations of the stomach and intestines. Before performing a stool occult blood test, meat, liver, and all foods containing iron should be excluded from the diet.
Benefits[edit]
Several studies have shown the potential benefits of sigmoidoscopy in detecting colorectal cancer.
In a 2009 Norwegian study, the results were somewhat inconclusive after seven years. [2]
We found a downward trend in colorectal cancer mortality for both overall colorectal cancer mortality (27% reduction) and rectosigmoid cancer mortality (37%), but this was not statistically significant in the intent-to-screen analysis. The corresponding reductions in mortality among visitors (that is, people actually screened, not just those in the group to be screened—this data set may include selection bias) were 59% and 76%, which are statistically significant compared with the control group. [.] [2]
The study found no significant difference in all-cause mortality.
A 2010 British study [3] found that sigmoidoscopy reduced “overall incidence and mortality from colorectal cancer by 31 percent” and “the incidence of cancer in the lower colon (or distal colon) alone was reduced by approximately 50 percent in those who were screened versus a control group." [4] Overall mortality from colon cancer was reduced by 43% (averting one cancer per 200 screenings and one cancer death per 500 screenings). The study also found that the effect was durable—a single sigmoidoscopy reduced the incidence of cancer throughout the 11-year study.
After the procedure
Although patients worry about the discomfort of the examination, most people tolerate it very well and feel much better afterwards. Most patients can return to normal activities, including eating, immediately after the examination. In many cases, the patient can go to work and drive the same day, as long as they have not received any medications that might interfere with these activities (such as medications used for sedation).
The patient should consult a doctor about the results of their test and, if they have any questions, they can always consult a specialist at the clinic.
Notes[edit]
- "Flexible Sigmoidoscopy". dx.doi.org
. Retrieved July 28, 2022. - ^ a b
Hoff, G.;
Grotmohl, T.; Skovlund, E.; Bretthauer, M.; Norwegian Colorectal Cancer Prevention Study Group (2009). "Risk of colorectal cancer seven years after flexible screening with sigmoidoscopy: a randomized controlled trial". BMJ
.
338
:b1846. DOI: 10.1136/bmj.b1846. PMC 2688666. PMID 19483252. - Atkin, W. S.; Edwards, R. Kral-Hans, I; Wooldrage, K; Hart, Arkansas; Northover, J.M.; Parkin, D.M. Wardle, J; and others. (2010). "One-time flexible screening with sigmoidoscopy in the prevention of colorectal cancer: a multicenter randomized controlled trial." Lancet
.
375
(9726):1624–33. DOI: 10.1016/S0140-6736(10)60551-X. PMID 20430429. - NCI summary archived 2011-06-07 at the Wayback Machine (accessed June 1, 2011)
- Adebogun, Akeem O.; Berg, Christine D.; Layemo, Adeyinka O. (August 2012). "Issues and challenges in flexible screening using sigmoidoscopy". Colorectal cancer
.
1
(4): 309–319. DOI: 10.2217/crc.12.33. ISSN 1758-194X. PMC 4108216. PMID 25067924.