Colon cancer is a malignant tumor that most often forms in people aged 40-70 years. The disease is asymptomatic for a long time or manifests itself as intestinal dysfunction. For this reason, the tumor is more often detected at a late stage of the oncological process, when difficulties arise with performing radical surgery.
- For the diagnosis and treatment of colon tumors, all conditions have been created at the Yusupov Hospital:
- European level of room comfort;
- The latest expert-class diagnostic equipment with high resolution;
- High level of qualification of doctors;
- Application of international protocols and standards for the treatment of malignant neoplasms of the colon;
- Attentive attitude of medical staff to the wishes of patients and their relatives.
Patients requiring palliative care may be treated in hospice care. Severe cases of colon cancer are discussed at a meeting of the Expert Council. Doctors and candidates of medical sciences, doctors of the highest qualification category take part in its work. Leading specialists in the field of oncology collectively develop patient management tactics.
Cause of the disease
Scientists have not yet established the exact cause of colon cancer. A malignant tumor can develop against the background of precancerous diseases: familial and acquired polyposis, villous tumors and adenomatous polyps. Researchers include the following pathological processes as factors that provoke tumor formation:
- Amoebiasis;
- Nonspecific ulcerative colitis;
- Diverticulosis.
The disease can develop due to poor nutrition and food composition. The tumor develops more often in people who eat large amounts of meat and meat products. Internal flora can produce carcinogenic substances from animal fats. The formation of a tumor is also caused by a violation of the passage of intestinal contents with insufficient consumption of fresh vegetables, fruits, and foods that contain a large amount of fiber.
IBD and calcium deficiency
Calcium deficiency is often observed in patients with IBD. The cause of deficiency may be impaired absorption (due to inflammation and as a result of vitamin D deficiency), increased loss and/or insufficient intake of calcium from food due to dietary restrictions or decreased appetite.
Calcium deficiency is associated with a risk of bone fracture due to osteoporosis (i.e. decreased bone mineral density), which can even lead to disability. In patients with IBD, osteoporosis can be both a complication of the disease itself and an expected side effect when taking steroid hormones.
Products containing calcium are milk and its derivatives (the source of more than half of the amount of calcium consumed), cheeses, eggs, soy isolates, buckwheat and oatmeal, fish and fish caviar. The patient's intolerance to milk and milk-based products or their unreasonable exclusion from the diet creates the preconditions for calcium deficiency. This is especially significant during therapy with steroid hormones, which promote calcium loss in the urine. In these cases, the daily requirement for calcium increases to 1500-2000 mg per day.
According to Russian standards of physiological needs for energy and nutrients for various groups of the population for healthy people is 1000 mg/day for men and women 18-60 years old, 1200 mg/day for people over 60 years old.
In order for the body to receive calcium in the required amount, it may be necessary to prescribe calcium supplements (necessarily in combination with vitamin D). Such drugs should be taken by all patients with IBD who take steroid hormones for more than 2 weeks. Calcium replacement therapy continues throughout the entire period of hormone treatment and is extended if necessary.
Kinds
Macroscopically, two forms of malignant neoplasm of the colon are distinguished - exophytic and endophytic. The first form of cancer is characterized by tumor growth into the intestinal lumen. It can take the form of a node or polyp, most often found in the right half of the colon, and is shaped like a cauliflower. An endophytic tumor in most cases forms in the left half of the colon. It infiltrates the intestinal wall, gradually covers its entire circumference and causes circular narrowing. Ulcers often form on the tumor.
Morphologists distinguish the following histological types of malignant neoplasms of the colon:
- Adenocarcinoma;
- Mucosal cancer;
- Solid cancer.
Colon cancer metastasizes late. This allows oncological surgeons to perform radical surgical interventions even with large tumors. The tumor is involved early in the inflammatory process. It often transfers to the fiber that surrounds the intestines. Metastases can remain in regional lymph nodes for a long time. They are removed during surgery along with the mesentery.
Make an appointment
What examinations should be performed if diverticular disease is suspected?
The first step in diagnosing diverticular disease outside of exacerbation is colonoscopy. Using a video camera inserted through the anus, more than a meter of intestine is examined - the entire large intestine and the final section of the small intestine. Colonoscopy allows not only to see the presence of a diverticulum, but also to determine the size of its gate, the condition of the wall, and its exact location. If other changes in the intestine are detected, colonoscopy allows you to take a piece of tissue for examination - perform a biopsy with further histological examination to understand the microscopic structure of the changes. This study can be performed under light anesthesia, which allows the patient to completely relieve the discomfort associated with the procedure.
The “gold standard” for diagnosing diverticular disease is irrigoscopy. This method allows you to determine the number of diverticula, their exact location, size and shape. The essence of the procedure is to inject an X-ray contrast agent into the colon, after which a series of X-rays are taken to evaluate the condition of the colon. In the photographs presented, arrows indicate the mouths of colonic diverticula. We marked with blue arrows multiple diverticula of the colon. This is exactly what they look like on a CT scan.
Figure 4. Irrigoscopy. Colon diverticulosis
On X-ray images taken during irrigoscopic examination, multiple diverticula of the colon are clearly visible. They look like sacs filled with radiopaque contrast agent.
No less important methods are ultrasound diagnostics and computed tomography. Due to its minimally invasive nature and ease of implementation, ultrasound diagnostics is very relevant at the stage of the initial examination. It allows you to see the presence of diverticula, identify indirect signs of their inflammation, such as infiltration, abscess, or suggest a generalized form - peritonitis.
To clarify the data obtained from ultrasound examination, if doubts arise and to clarify the diagnosis, spiral computed tomography is performed. Virtual computed tomography creates a three-dimensional image of the colon, including affected areas. Using this technique, you can accurately determine the boundaries of the infiltrate or abscess, and other organs involved in the inflammatory process.
Figure 5. Virtual colonoscopy. Orifice of diverticulum
Symptoms
The colon is a segment of the large intestine. The main functions of the colon are secretion, absorption and evacuation of intestinal contents. The colon has the longest length. It consists of the ascending, descending, transverse and sigmoid colon, has a hepatic flexure, and a splenic flexure. Colon cancer is one of the most common malignant diseases in developed countries, where the population consumes excess amounts of animal fats, a lot of meat and very little fresh vegetables and fruits.
Symptoms of the disease become more pronounced as the tumor grows and the body becomes intoxicated. The clinical picture can be varied, depending on the location, shape of the tumor, and various aggravating circumstances. Left-sided colon cancer is characterized by rapid narrowing of the intestinal lumen and the development of its obstruction. Right-sided colon cancer is characterized by anemia and intense abdominal pain. In the early stages of development of colon cancer, symptoms are similar to various diseases of the gastrointestinal tract, which often does not allow a correct diagnosis to be made in a timely manner. Symptoms of colon cancer include:
- belching;
- irregular vomiting;
- heaviness in the stomach after eating;
- nausea;
- flatulence;
- abdominal pain;
- constipation or diarrhea;
- change in the nature of the stool, its shape;
- feeling of discomfort, incomplete bowel movement;
- Iron-deficiency anemia.
Colon cancer is often accompanied by infection and the development of an inflammatory process in the tumor. Abdominal pain may resemble the pain of acute appendicitis, the temperature often rises, and blood tests show an increase in ESR and leukocytosis. All these symptoms often lead to medical errors. Early manifestations of colon cancer are intestinal discomfort, the symptoms of which are often attributed to diseases of the gallbladder, liver, and pancreas. Constipation in colon cancer cannot be treated, which becomes an important symptom of the development of cancer. Left-sided colon cancer is much more often accompanied by intestinal disorders than right-sided colon cancer.
Constipation with colon cancer can be replaced by diarrhea, the stomach is swollen, belching and rumbling in the stomach are disturbing. This condition can bother you for a long time. Prescribing a diet and treating intestinal disorders does not bring results. The most severe symptoms with bloating and constipation, characteristic of cancer of the rectosigmoid intestine, appear in the early stages of cancer development.
Intestinal obstruction in colon cancer is an indicator of a late manifestation of cancer and is more common in left-sided forms of cancer. The right section of the intestine has a large diameter, a thin wall, and the right section contains fluid - obstruction of this section occurs in the later stages of cancer. The left section of the intestine has a smaller diameter, it contains soft feces; as the tumor grows, the intestinal lumen narrows and the lumen becomes blocked with feces - intestinal obstruction develops.
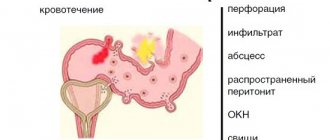
Upon palpation, doctors identify a stationary, slightly painful tumor in the right half of the abdomen. Due to the smaller diameter of the descending colon, the dense consistency of stool, endophytic growth with narrowing of the intestinal lumen, intestinal obstruction often develops with cancer of this localization. Colon cancer can be complicated by bleeding, intestinal obstruction, perforation (perforation of the intestinal wall), tumor growth into neighboring organs, and tumor inflammation.
With the right-sided form of cancer, patients often discover the tumor themselves by palpation of the abdomen.
Blood in stool
Patients complain of the presence of impurities in the stool: blood, pus, mucus. Bloody discharge in colon cancer is more often observed in exophytic types of tumors, begins with tumor disintegration, and is a late manifestation of malignancy. In some cases, the appearance of blood in the feces is the only sign of cancer, especially if the tumor is located in the left half and splenic angle of the colon.
Depending on the location of the tumor, stool may look different. When the ascending colon is affected, the stools are brown in color or tarry stools are observed. Feces mixed with blood are a sign of a tumor located in the area of the splenic angle and adjacent parts of the descending intestine. When the final section of the colon is affected, unchanged (scarlet or dark red) blood covers the stool.
Bloody discharge in colon cancer is more often observed in exophytic types of tumors, begins with tumor disintegration, and is a late manifestation of malignancy.
Cancer of the ascending colon
Cancer of the ascending colon is characterized by severe pain. Pain in the abdomen is also very disturbing with cancer of the cecum. This symptom is one of the signs of cancer of these parts of the colon.
Cancer of the splenic flexure of the colon
Due to its anatomical location, cancer of the splenic flexure of the colon is difficult to detect by palpation. Cancer of the hepatic flexure of the colon is also poorly defined. Most often, the examination is carried out in a standing or semi-sitting position. Such a study during the initial examination of the patient allows one to obtain information about the presence, size of the tumor and its location.
Transverse colon cancer
Transverse colon cancer develops less frequently than sigmoid or cecal cancer. With a growing tumor of the transverse colon, the right colon, middle, left colon and lower mesenteric lymph nodes are affected. Symptoms of transverse colon cancer are loss of appetite, a feeling of heaviness in the upper abdomen, belching, and vomiting. Such symptoms often characterize cancer of the right side of the transverse colon.
IBD and iron deficiency
Iron deficiency occurs in 60-80% of patients with IBD, and iron deficiency anemia occurs on average in 16% of outpatients and 64% of inpatients. The causes of iron deficiency and the development of iron deficiency anemia in ulcerative colitis and Crohn's disease are different: blood loss , decreased absorption of this microelement in the small intestine due to the inflammatory process, as well as insufficient intake due to dietary restrictions and poor appetite.
Healthy people absorb approximately 5-10% of the iron contained in food, and in conditions of iron deficiency - 10-20%. The absorption of iron from the intestines depends on the type of food: it is best absorbed from mammalian meat - 22%, from liver - 12-16%, from fish - 9-11%, while 2-3% of iron is absorbed from eggs and beans , from fruits - 3-4%, from rice and spinach - 1%. Oxalic acid (spinach, sorrel, legumes), tannins (blueberries, quince), phosphates and phytins (found in grains, legumes), strong tea and excess dietary fiber worsen the absorption of iron. Egg, soy, and milk proteins also reduce the absorption of iron from the gut. Organic acids (malic, citric, ascorbic) improve iron absorption. It is optimal to combine in one dose products containing heme iron (animal meat, poultry, liver, kidneys) and products rich in organic acids (rosehip decoction, blackcurrant, clarified juices, lemons, etc.).
Unfortunately, it is almost never possible to restore iron reserves in the body with diet alone, so patients are additionally prescribed iron supplements.
With low activity or remission of IBD, therapy for iron deficiency and mild iron deficiency anemia most often begins with oral iron supplements (tablets, capsules, dragees or liquid forms). Typically, these drugs are prescribed in a dose of 100-200 mg of iron per day (in terms of elemental iron), since the effectiveness does not increase with increasing dose, and the likelihood of side effects increases.
Iron therapy is considered effective when it leads to an increase in hemoglobin levels by 20 g/l or more within 4 weeks. After normalization of hemoglobin levels, iron supplements should be taken until the tissue depot of iron reserves is restored (controlled by determining the level of ferritin).
In case of high disease activity, intolerance or ineffectiveness of oral iron preparations (increase in hemoglobin, the use of parenteral forms of iron preparations (for intramuscular or intravenous administration) is recommended. In recent years, “bolus” intravenous iron preparations have become widespread, allowing the administration of a significant amount of iron in one infusion ( up to 500-1000 mg).
Complications
Colon cancer causes severe and life-threatening complications:
- Bleeding;
- Intestinal obstruction;
- Perforation (perforation of the intestinal wall);
- Growth of the tumor into neighboring organs;
- Inflammation of the tumor.
Bleeding from the colon in the presence of a malignant neoplasm is rarely profuse. Basically, blood is mixed with feces and determined using laboratory tests.
Intestinal obstruction in most patients is the first manifestation of the disease. It is an obstructive intestinal obstruction (a growing tumor narrows the lumen of the colon).
Intestinal perforation poses a great danger to the patient. Perforation occurs either in the area of the tumor during ulceration or decay, or proximally (above) it as a result of excessive stretching of the intestinal wall with contents. When a colon tumor perforates, the patient's condition sharply worsens and fecal peritonitis develops, often with a fatal outcome.
Great difficulties for diagnosis and treatment are inflammatory and suppurative processes in the tissue that surrounds the tumor of the colon. The infection most often affects the retroperitoneal tissue of the ascending and descending colon, which lack a serous membrane. In the presence of inflammation, patients complain of pain in the lower back and posterior abdominal wall. Their body temperature rises. During palpation, doctors determine muscle tension and pain in the anterior abdominal wall and lower back.
Make an appointment
Diagnostic methods
Doctors at the Oncology Clinic of the Yusupov Hospital make a diagnosis of colon cancer based on an analysis of the clinical picture of the disease, physical examination data, endoscopic and radiological studies, and biopsy results. The following changes may occur in the blood test:
- Anemia (decreased number of red blood cells and hemoglobin);
- Hypoproteinemia (decreased protein concentration);
- Increased erythrocyte sedimentation rate;
- Hypoprothrombinemia (decreased platelet count);
- Decreased hematocrit.
A laboratory test is used to determine the presence of occult blood in the stool. During irrigoscopy (x-ray examination of the large intestine with barium contrast), the location, size, extent and growth pattern of the tumor are determined. X-rays show characteristic signs of a malignant tumor of the colon:
- Narrowing (stenosis) of the intestinal lumen;
- Filling defect;
- Rigidity of the intestinal wall.
Colonoscopy (endoscopic examination) allows you to examine all parts of the colon and perform a biopsy. Sections of tissue from pathologically changed areas of the intestine are sent to a morphological laboratory to verify the histological type of cancer. Using colonoscopy, performed using the latest equipment, oncologists at the Yusupov Hospital identify the initial stages of colon cancer that are inaccessible to other research methods.
To exclude the presence of liver metastases, radioisotope scanning is performed. Doctors at the oncology clinic take the results of the study into account when determining the stage of the tumor process and drawing up a plan for surgical intervention. Positron electron computed tomography (PET-CT) is performed if metastases are suspected. If using these diagnostic methods it is not possible to establish an accurate diagnosis, oncologists perform exploratory laparotomy.
Before surgery, surgeons carry out a differential diagnosis of colon cancer with the following diseases:
- Tuberculosis;
- Crohn's disease;
- Actinomycosis.
If the tumor is located in the left half of the colon, amebiasis, diverticulitis, and ulcerative colitis are excluded. If the hepatic angle is affected by a malignant tumor, a differential diagnosis is made with a tumor of the liver or right kidney, calculous cholecystitis. If oncologists suspect cancer of the splenic flexure of the colon, they exclude a tumor and cyst of the spleen, tail of the pancreas or left kidney.
IBD and vitamin D deficiency
Vitamin D is synthesized under the influence of ultraviolet rays in the skin and also enters the human body with food. It is the main link in the hormonal regulation of calcium and phosphorus metabolism, stimulating the absorption of phosphorus in the intestine, promoting the deposition of calcium salts in the bone matrix. Vitamin D absorption occurs in the initial parts of the small intestine. Hypo- or avitaminosis D reduces calcium absorption with the development of secondary hyperparathyroidism, which leads to leaching of calcium from the bones. As a result, adult patients experience osteomalacia, which is characterized by low mineralization of bone tissue and increases the risk of fractures. The daily requirement for vitamin D for a healthy person, according to domestic standards, is 400 IU or 10 mcg/day, i.e. 1 mcg is equivalent to 40 IU of vitamin D.
Vitamin D deficiency is often observed in patients with ulcerative colitis and Crohn's disease. 50-70% of patients with IBD experience a decrease in the level of this vitamin in the blood. According to recent data, vitamin D deficiency is not only a consequence of a long-term active disease, but may in some cases precede the onset of IBD. Thus, in 2012, the results of long-term observations of 73 thousand women in the United States were published, assessing the level of vitamin D in the blood. It was found that women who had vitamin levels less than 20 ng/ml had a greater risk of developing Crohn's disease in the next 20 years. High levels of vitamin D (more than 30 ng/ml) reduced the risk of developing ulcerative colitis.
This is why there is a hypothesis that initially low levels of vitamin D may be a predisposing factor for the onset of IBD in individuals with a genetic predisposition, due to its influence on various immune mechanisms.
According to clinical studies, low levels of vitamin D in the blood are associated with:
- high risk of surgical intervention in patients with IBD
- higher incidence of infectious complications
- greater disease activity (especially Crohn's disease).
There are scientific studies showing an increase in the risk of developing colon cancer in patients with IBD with a decrease in vitamin D levels.
How can you detect vitamin D deficiency? Clinically, i.e. Based on the symptoms, this is quite difficult, so an assessment of vitamin D in the blood is recommended (the level of 25-hydrocalciferol is examined). It is advisable to conduct the study at the stage of establishing a diagnosis, before starting steroid hormone therapy and then at least once a year.
All patients with low vitamin D levels (less than 30 ng/ml) require correction of the deficiency. Replacement therapy is usually carried out by prescribing vitamin D3 in various forms (oil solution, tablets in combination with calcium supplements). Doses are determined by the attending physician and depend on the severity of the deficiency (varying from 1000 to 4000 IU). When carrying out vitamin D replacement therapy, it is important to remember that its uncontrolled use in high doses can lead to accumulation (cumulation) and the development of hypervitaminosis D.
The main food sources of vitamin D (IU/100 g) are fish oil or cod liver (4000.0), sardines (1380), salmon (300), 1 egg yolk (100), butter (40). However, most of these products are poorly tolerated during the phase of exacerbation and unstable remission of IBD, so their use in diet therapy is limited.
Exposure to the sun (insolation) can also replenish vitamin D deficiency.
To ensure a normal dose of the vitamin, it is necessary to stay with your limbs exposed to the sun's rays in the midday sun (between 10 am and 3 pm) at least twice a week - 5 minutes for people with fair skin and at least 30 minutes for dark-skinned people.
Treatment
Oncologists at the Yusupov Hospital remove a malignant tumor of the colon using surgery. Resection of the affected area of the colon along with the mesentery is performed, and lymph nodes are also removed. If cancer of the ascending colon is detected, treatment is carried out by right hemicolectomy. The tumor of the cecum is removed using the same method. The surgeon removes the lymphatic system, the entire right half of the colon, including one-third of the transverse colon, ascending colon, cecum, and portion of the hepatic flexure.
Preparing for surgery
Regardless of the nature and scope of the operation, doctors at the Oncology Clinic carry out general and special preoperative preparation, which largely ensures the success of the surgical intervention. With the help of modern infusion agents, water-electrolyte imbalances are eliminated, protein levels are normalized, and hypochromic anemia and intoxication are combated. Patients are given intravenous infusion of drugs and blood components, glucose with vitamins, and electrolyte solutions. At the same time, measures are taken to improve the function of vital organs (heart, lungs, adrenal glands, liver, kidneys).
Special preparation is aimed at removing feces mechanically. Patients are given laxatives, given enemas, and pathogenic microflora, which is abundantly present in the intestinal contents, is suppressed with medications.
For preoperative preparation of the large intestine, an elemental diet is used. 3-5 days before surgery, doctors prescribe special medications to patients that contain all vital food ingredients in refined form.
Make an appointment
Palliative resections
In the absence of the technical ability to perform radical surgery, surgeons perform palliative resections of the colon. The choice of palliative intervention depends on the following factors:
- Localization of the neoplasm;
- Degree of tumor spread;
- Anatomical features of the location of the primary lesion;
- Complications of the tumor process;
- General condition of the patient.
If it is impossible to remove the tumor of the right half of the colon, surgeons perform a bypass ileotransverse anastomosis. For inoperable neoplasms of the descending colon and splenic angle, a bypass transversosigmoanastomosis is created. If a tumor of the final part of the colon is detected, a proximal colostomy, single-barrel or double-barrel unnatural anus, is applied.
Chemotherapy
Chemotherapy in the treatment of colon cancer is used for different purposes - to shrink the tumor before surgery, stop its growth, destroy cancer cells, and metastases. Colorectal cancer is a tumor that is quite resistant to cytostatics. Chemotherapy for colon cancer is prescribed by a doctor depending on the size of the tumor and the presence of metastases, and is carried out in courses.
If regional lymph nodes are affected or the tumor has invaded the serous membrane of the intestine, adjuvant chemotherapy is performed. If there is a potential risk of developing metastases to other organs, the most active chemotherapy is performed. After several cycles of treatment with antitumor drugs, the state of metastases is assessed and the lesions are removed. After surgery, adjuvant chemotherapy is used.
Metastases
Colon cancer most often metastasizes to regional lymph nodes not immediately, but after a long time after tumor development.
The tumor often grows into neighboring tissues and organs. Colon cancer is generalized, with penetrating metastases to the lungs, liver requires consultation with a thoracic surgeon, hepatologist surgeon. Unresectable colon cancer is characterized by tumor growth into bone structures and great vessels. The possibility of tumor removal is being assessed; if surgery is not possible, palliative treatment (chemotherapy) is used.
Initially resectable metastatic lesions are removed surgically, followed by palliative chemotherapy. Also, as a treatment, systemic chemotherapy is carried out before surgery to remove metastases, and after surgery, chemotherapy treatment is continued.
Forecast
The prognosis in the absence of metastases to regional lymph nodes is optimistic. The five-year survival rate is about 80%. In the presence of metastases to regional lymph nodes, about 25% of patients live for more than five years.
When the first signs of colon dysfunction appear, make an appointment with an oncologist at the Yusupov Hospital by calling the contact center phone number. Detection and treatment of colon cancer at an early stage of the disease improves the prognosis and promotes cure for the patient.
Make an appointment
What is diverticular disease (diverticulosis) of the colon?
Diverticula (Latin diverticulum - literally “branch”, “road to the side”) are understood as sac-like protrusions of all layers of the wall of the colon or only the mucous membrane and submucosal layer through a defect in the muscle layer.
Figure 1. Section of the colon. Diverticulum
Colon diverticulosis is a condition in which there is at least one diverticulum in the colon.
Figure 2. Diverticulosis of the left colon
Diverticular disease is a disease characterized by clinical manifestations of the inflammatory process and its possible complications - abscesses, perforation of diverticula, fistula formation, peritonitis, and bleeding.