In medicine, a condition characterized by a restructuring of the functions of the biliary system after surgery to eliminate the consequences of cholelithiasis, accompanied by impaired motility of the sphincter of Oddi and duodenal motility, is called postcholecystectomy syndrome. The pathology is accompanied by various disorders of the digestive system, and in some cases leads to extreme exhaustion, vitamin deficiency, re-formation of stones and other complications.
In the classification of diseases, this syndrome is assigned a code according to ICD-10: K-91.5. Previously, the syndrome included organic and physiological disorders after removal of the gallbladder. Today, gastroenterologists apply this term to situations in which exclusively functional disorders are noted that arose after gall bladder surgery.
General information
Postcholecystectomy syndrome (PCES) is a whole complex of symptoms that appear in a person after he has had his gallbladder removed. This condition is characterized by attacks of pain, digestive problems, diarrhea , weight loss, etc.
According to medical statistics, postcholecystectomy syndrome, whose ICD-10 code is K91.5, occurs in 5–40% of patients. Experts suggest that this condition is either a continuation of the disease that led to surgery, or a consequence of the operation. As a rule, removal of the gallbladder does not lead to serious negative consequences for the functioning of the biliary tract. About 10% of cases of biliary colic are the result of disorders of the sphincter of Oddi , both structural and functional. The term " sphincter of Oddi dysfunction " is also used instead of the definition of "postcholecystectomy syndrome".
How postcholecystectomy syndrome can manifest itself when a spasm of the sphincter of Oddi occurs and how to act correctly to eliminate unpleasant signs will be discussed in this article, which describes the symptoms and treatment of postcholecystectomy syndrome.
Treatment
When treating PCES, diet No. 5 is prescribed. It is allowed to drink weak tea, wheat bread, compote, cottage cheese (necessarily low-fat), vegetable soups, cereals, salads, legumes, lean beef, and non-acidic fruits.
It is prohibited to consume baked goods, fatty meat, mustard, alcohol, ice cream, various semi-finished products, sorrel, fatty fish, spinach, and black coffee. Small and fractional meals are prescribed to slowly reduce body weight.
The diet includes vitamin therapy (folic acid, B12, vitamins K, A, E, and iron). Dietary fiber is also added to the diet. Consumption is limited to foods that are poorly digestible because they do not contain food enzymes. To treat PCES, it is necessary to limit physical and mental stress on the human body.
Postcholecystectomy syndrome is also treated with medication. To control the functions of the sphincter of Oddi, nitroglycerin preparations are prescribed, which control the flow of bile from the body.
Anti-spasm medications and painkillers are prescribed to reduce pain. Enzyme preparations are used to improve digestion. Antacid medications are prescribed to reduce the acidity of gastric juice.
Antibacterial medications are needed to cure a bacterial infection, if present. If scars or stones remain after the operation, or they appear during treatment, then surgical intervention is necessary.
Complications
After the operation, complications may develop such as:
- divergence of wound edges due to failure of surgical sutures;
- infection in the wound;
- development of ulcers or abscesses;
- pneumonia;
- SIBO (bacterial overgrowth syndrome);
- atherosclerosis (a disease of the arteries of a chronic type, which begins to develop due to disturbances in lipid metabolism; the disease is accompanied by the deposition of cholesterol on the walls of blood vessels);
- complications of malabsorption (impaired absorption of nutrients and vitamins in the intestine).
The occurrence of the disease is associated with a lack of nutrients, certain vitamins and microelements:
- anemia occurs when there is a decrease in hemoglobin (the protein that carries oxygen) and red blood cells in the blood of a sick person;
- body weight decreases;
- hypovitaminosis or vitamin deficiency develops in the body;
- the skeleton is deformed;
- impotence (sexual impotence) develops.
Prevention
Before performing the operation, it is necessary to carry out a thorough examination of the body, and the patient must also receive appropriate care after the operation.
It is necessary to promptly diagnose and treat diseases that can play a significant role in the development of postcholecystectomy syndrome. These are diseases such as gastritis (in which inflammation of the stomach occurs), pancreatitis (when the pancreas becomes inflamed), cholecystitis (when the gall bladder becomes inflamed), cholelithiasis (when stones form in the gall bladder), enterocolitis (when the small and large intestines become inflamed) and other diseases.
To prevent and prevent the disease, you need to adhere to a balanced diet (eat foods containing fiber), avoid fried and canned foods, take vitamins and mineral complexes, and avoid excessive drinking and smoking.
Pathogenesis
The majority of patients with this syndrome have functional motor disorders. An integral part of the pathogenesis of cholelithiasis is motor disorders of the gallbladder and the sphincter apparatus of the biliary tract.
Due to the removal of the gallbladder, there is a dysfunction of the sphincter apparatus of the biliary tract. The development of pain after surgery is usually associated with an increase in pressure in the biliary tract, which is associated with dysfunction of the sphincter of Oddi.
In the body, the sphincter of Oddi provides an anatomical and physiological connection between the biliary tract, pancreas and duodenum.
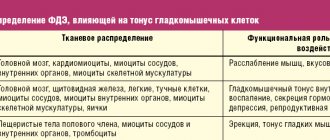
The physiological control of the sphincter of Oddi is determined by a number of hormonal and neural stimuli. In particular, gastrointestinal hormones play an important role in this regulation. Of particular importance are cholecystokinin (pancreozymin) and secretin .
When the gallbladder contracts and the sphincter of Oddi simultaneously relaxes, concentrated bile enters the duodenum. At this time, pancreatic juice is released under the influence of cholecystokinin, which provides all the conditions for the breakdown of food. If a sphincter spasm occurs, this process is disrupted.
The gallbladder is directly involved in modulating the response of the sphincter of Oddi to the influence of gastrointestinal hormones. After removal of the gallbladder, the sphincter of Oddi response to cholecystokinin decreases.
Sphincter of Oddi
There are different opinions about how the functional state of the sphincter of Oddi changes after cholecystectomy. In particular, there is a theory that after surgery the tone increases and the common bile duct expands. There is also an opinion that cholecystectomy results in insufficiency of the sphincter of Oddi, since it cannot withstand high bile pressure for a long time. The contradictions that are noted in the description of the state of the sphincter of Oddi are due to the fact that its functions were studied at different times after cholecystectomy.
Reasons for the development of PCES
In patients who have had their gallbladder removed, the main regulatory function is the sphincter of Oddi (SO), a circular muscle located at the exit of the bile duct into the duodenum. CO is responsible for the flow of bile into the intestines.
The development of PCES is based on a violation of the contractility of the sphincter. In many ways, its work depends on the pressure gradient between the duct system and the duodenum. There are other factors influencing the formation of PCES:
- Bacterial overgrowth syndrome (SIBO), which has developed in the intestines as a result of a decrease in the concentration of bile and a decrease in its bactericidal properties.
- Duodenal hypertension is an increase in pressure in the duodenum, as a result of SIBO.
- Chronic biliary insufficiency.
- Increased pressure in the intestines and abdominal cavity.
- Duodenogastric reflux.
Classification
In modern medicine there is no generally accepted classification of postcholecystectomy syndrome. Depending on the reason why such symptoms appear, in their practice, doctors define this condition broadly, using the following classification:
- Recurrences of the formation of common bile duct stones – both false and true.
- Stenosing duodenal papillitis.
- Strictures of the common bile duct.
- Limited peritonitis in chronic form.
- Cholepancreatitis.
- Secondary gastroduodenal ulcers are biliary or hepatogenic.
However, the 1999 Rome II criteria, as well as the 2006 Rome III criteria, limit the scope of “PCES” to sphincter of Oddi dysfunction occurring after cholecytectomy. The following classification of sphincter of Oddi dysfunction is used:
Dysfunction of the sphincter of Oddi of the biliary type. Three types of this variety are defined:
- Biliary type I - typical attacks of pain lasting 20 minutes or more appear; the common bile duct expands by more than 12 mm; when performing endoscopic retrograde cholangiopancreatography, the removal of the contrast agent slows down by more than 45 minutes; there is an excess of transaminases and/or alkaline phosphatase.
- Biliary type II – attacks of biliary pain appear; up to 63% of patients have manometric confirmation of the sphincter of Oddi. In this case, both structural and functional disorders are possible.
- Biliary type III - attacks of biliary pain without objective disturbances appear. Manometric confirmation of the sphincter of Oddi is observed in only 12-28% of patients. As a rule, dysfunction is of a functional nature.
Dysfunction of the sphincter of Oddi of the pancreatic type . The pancreatic type is manifested by epigastric pain, which is characteristic of pancreatitis . The pain radiates to the back and decreases when the patient leans forward. amylase and lipase levels increase significantly . Manometry reveals dysfunction of the sphincter of Oddi in 39–90% of cases.
Dysfunction of the sphincter of Oddi of mixed type . The mixed type is characterized by girdle pain, or the pain is localized in the epigastrium. Other signs characteristic of both biliary and pancreatic types also appear.
3. Symptoms, diagnosis
In the clinical picture of DSO, biliary (bile), pancreatic (pancreas) and combined types of symptoms are distinguished, which depends on the nature of organic and functional disorders in a particular case. The most common symptoms of DSO are pain in the hypochondrium and dyspepsia (indigestion). Sometimes the pain radiates to the back or under the shoulder blade. With the pancreatic type, such pain is localized on the left side, with the biliary type, on the right, with the combined type, it is girdling in nature. There are recurrent attacks of pain due to eating or during sleep, often with nausea and vomiting. Often, DSO is also accompanied by symptoms of intestinal dyskinesia and/or inflammation of the intestinal mucosa.
To diagnose DSO in each individual case, you may need your own set of diagnostic measures - fortunately, modern medicine has a fairly wide selection of them. In addition to the mandatory clinical questioning and examination, indirect studies (all kinds of laboratory tests) are prescribed; Ultrasound is widely used in various methodological modifications; ERCP (endoscopic retrograde cholangiopancreatography) is performed, and if the clinic has such a possibility, direct manometry is performed, an invasive and comprehensively informative method for studying the circulation of bile and pancreatic secretions through the sphincter system.
About our clinic Chistye Prudy metro station Medintercom page!
Causes
Most often, signs of PCES appear due to the following reasons:
- Stones in the bile ducts (choledocholithiasis). These can be either relapses of cholelithiasis , when stones re-form, or false relapses with remaining stones. In most cases, the stones that remain are those that were not removed during the first operation.
- Organic and functional changes in the major duodenal papilla (MDP). This reason leads to pain, fever and jaundice after removal of the gallbladder. After such an intervention, in most patients the tone of the sphincter of the abdominal joint increases for some time. But in the absence of pathological changes, the tone gradually returns to normal. Approximately a quarter of the operated people have stenosis of the abdominal joint. First, swelling develops, after which, with prolonged trauma during the passage of stones, its narrowing is noted.
- Damage to the bile ducts and strictures. The narrowing of the duct occurs either due to changes in the wall associated with inflammation, or is a consequence of the presence of a stone there. Sometimes this is influenced by external reasons.
- Cholangitis . With poor release of bile, it stagnates in the bile ducts. As a result, conditions are created for the upward spread of infection. With cholecystectomy, only one source of infection is removed, but the ducts may remain infected.
- Features of the operation. Recurrence of pain develops if the remaining part of the gallbladder or stump contains stones or condensed bile.
- Tumors of the bile ducts. They may not be detected during the operation or they may appear later.
- Diseases of the duodenum. People with diseases of the biliary tract often experience swelling and hyperemia of the mucous membrane of the duodenum, its atrophy, and impaired motor function.
- Chronic pancreatitis. Often found in people who have had cholecystectomy. With a technically correctly performed cholecystectomy, the outflow of pancreatic juice improves and the exocrine function of the gland is restored. But if fibrotic changes are pronounced, then after surgery pancreatitis can manifest itself as an independent disease.
- Other reasons. Recurrence of pain after surgery can be caused by dysbiosis , colitis , impaired intestinal absorption, hemolytic disease, as well as diseases of the kidneys, colon, and spine. Pain not associated with changes in the biliary system can also be perceived as PCES.
Symptoms of postcholecystectomy syndrome
The main symptoms of spasm of the sphincter of Oddi are the manifestation of attacks of severe or moderate intensity pain that last more than 20 minutes and appear for more than three months. Dyspeptic and neurotic disorders also appear. I'm worried about heaviness in the right hypochondrium. As a rule, the pain is constant. Sometimes attacks appear rarely at first and last for several hours, and then, in the intervals between attacks, pain is not felt at all. In some patients, the frequency of attacks and the intensity of pain increases over time. The connection between attacks and food intake manifests itself differently for everyone. But most often the pain occurs 2-3 hours after eating.
Sometimes, in severe cases, the pain is prolonged and persistent, it is combined with vomiting and nausea, as well as painful attacks of heartburn .
If the causes of PHES are associated with a true relapse of the formation of bile duct stones, then unpleasant symptoms appear no earlier than several years after the operation. In this case, the following symptoms develop:
- Pain in the right hypochondrium and in the right part of the epigastric region is usually monotonous, less often in the form of attacks. In most cases, the pain is less severe than before surgery.
- Impaired bile circulation, as confirmed by diagnosis.
- An infectious and inflammatory process that develops as a result of impaired bile circulation. It manifests itself with fever and poor health. ESR increases . If purulent cholangitis , the symptoms worsen.
- With a false recurrence of bile duct stone formation, the manifestations are similar to a true relapse. But with this condition, symptoms appear earlier - about 2 years after surgery.
Clinical manifestations of PCES
Symptoms that existed before surgery may persist after cholecystectomy. Often complaints arise for the first time after surgery.
The main clinical manifestation is pain of varying severity, usually of a paroxysmal nature, lasting from 20 minutes, which has been disturbing for more than 3 months. Pain can occur both after eating and at night. Often accompanied by nausea or vomiting.
There are three clinically significant variants of PCES:
- Biliary – characterized by paroxysmal pain in the right hypochondrium.
- Pancreatic, in which pain in the upper part of the abdomen of a girdling nature is noted.
- Combined bile-pancreatic type.
The second most common disorder is dyspepsia. Patients have the following complaints:
- nausea, vomiting);
- bitterness in the mouth;
- heartburn;
- flatulence;
- diarrhea;
- “fatty” stool (steatorrhea).
As a result of insufficient absorption in the intestines, the body does not absorb sufficient amounts of nutrients, vitamins and microelements. In this regard, other complaints arise: weight loss, general weakness, lethargy, anemia, erectile dysfunction, cracks in the corners of the lips (jams) and other manifestations of vitamin deficiency.
The patient may be concerned about an increase in body temperature, yellowness of the skin and sclera, which indicates the presence of an inflammatory process and cholestasis (cessation or reduction of the passage of bile in the duodenum). If there are any complaints after cholecystectomy, the patient should consult a gastroenterologist to clarify the diagnosis and decide on treatment.
Tests and diagnostics
People who have undergone cholecystectomy are monitored by a specialist in order to early identify unfavorable results, as well as provide important preventive measures and monitor the patient's compliance with recommendations.
During the diagnostic process, a number of studies and laboratory tests are carried out. The doctor necessarily studies the medical history, conducts a survey and examines the patient. To establish a diagnosis, the following is carried out:
- General blood analysis.
- Biochemical blood test, during which biochemical markers of cholestasis-cytolysis syndrome are determined.
- Analysis of urine.
- Electrocardiography.
- Chest X-ray.
- Ultrasonography.
- FGDS.
- CT, MRI.
In the process of examining patients who complain of signs of PCES, the principle of searching for the causes of such manifestations from simpler to more complex is used, as well as using techniques from non-invasive to more traumatic, but allowing one to obtain important information.
Another important point concerns surgical vigilance for such symptoms: it should be greater, the less time has passed since the operation.
As a rule, after laboratory tests, examination of such patients begins with an ultrasound of the abdominal cavity, which makes it possible to exclude anatomical changes in organs and move on to more targeted examinations.
However, despite the fact that the possibilities of modern diagnostics are quite wide, in a certain number of people it is not possible to find out the cause of unpleasant symptoms after undergoing cholecystectomy .
Treatment with folk remedies
You can use folk remedies for postcholecystectomy syndrome after the approval of such methods by your doctor. Some of them can alleviate the condition and improve the general well-being of the patient.
The following traditional treatment methods can be used:
- Collecting herbs is the first option. It is used after removal of the gallbladder. You need to take 4 parts of immortelle flowers and coriander seeds, as well as 3 parts of watch and peppermint. Mix everything and pour 2 tbsp. l. 350 ml boiling water. After an hour and a half, strain and drink 100 ml before meals. However, such treatment must be agreed with your doctor.
- Herbal collection is the second option (choleretic). It includes chamomile, calendula, peppermint, yarrow in equal proportions. You should also add some tansy flowers - its amount should not be more than 10 parts of the total amount collected. Take 2 tbsp. l. collection and pour 250 ml of boiling water. Leave for an hour, strain, add water so that the total amount of product is 250 ml. Drink three times throughout the day. Consume before meals.
- Collecting herbs is the third option. Mix an equal amount of celandine, lemon balm, peppermint, and cinquefoil. 1 tbsp. l. collection, pour 250 ml of boiling water, leave. Drink a third of a glass three times a day before meals.
- Collecting herbs is the fourth option. Mix 10 g of St. John's wort and wheatgrass roots, 20 g of immortelle flowers and buckthorn bark. 2 tbsp. l of the mixture, pour 500 ml of boiling water, cook for 5 minutes. Drink half a glass 5 times a day.
- Decoctions and infusions of herbs. You can also prepare decoctions and infusions of some herbs. If pathological processes develop after surgery, it is recommended to drink calendula infusion (30 g of flowers pour 1 liter of boiling water). They drink it throughout the day. In the evening you need to drink the infusion. It is recommended to drink a decoction of Solyanka Kholmovoy (1 tsp of the product per 250 ml of boiling water, cook for about 5 minutes). Drink half a glass 3-4 times a day. A decoction of immortelle is useful (10 g of flowers per 250 ml of boiling water, cook for 5 minutes). Drink 3 tbsp. l. before eating. You can prepare a decoction of birch buds (20 g of product per 250 ml of boiling water, cook for 10 minutes). Drink 1 tbsp before meals. l. Infusions of St. John's wort, chamomile, and elecampane root are also recommended - such infusions are prepared at the rate of 10 g of raw material per 200 ml of water. These infusions should be drunk three times a day before meals, half a glass. It is recommended to alternate taking infusions of different herbs.
- Dandelion root. It must be crushed into powder and taken half a teaspoon. three times a day for 20 minutes. before meals, with water.
Prevention
- The most important condition for the prevention of PCES is timely surgery, a comprehensive examination of patients, and compliance with all doctor’s recommendations during the rehabilitation period.
- In the period before surgery, it is necessary to reduce the severity of disorders on the part of the organs of the hepatopancreatobiliary system by carrying out appropriate treatment.
- In the period after surgery, adequate medical supervision and the implementation of a set of rehabilitation measures, which are determined by the doctor, are very important.
- It is necessary to eat right, strictly adhering to the diet.
- It is also important to eliminate stress, both physical and emotional.
Diet
Diet 5th table
- Efficacy: therapeutic effect after 14 days
- Duration: from 3 months or more
- Cost of products: 1200 - 1350 rubles per week
Diet Table No. 5a
- Efficacy: therapeutic effect after 5-7 days
- Time frame: 2-6 weeks
- Cost of products: 1300 - 1400 rubles per week
After removal of the gallbladder, the patient is recommended to follow Diet No. 5 , and later Diet No. 5a . If the patient has complications from the pancreas, Diet No. 5 . Those who exhibit symptoms of sphincter of Oddi dysfunction also need to follow a strict diet.
The diet involves excluding those foods that contain large amounts of cholesterol , essential oils, and coarse fiber. Animal fats are limited.
It is recommended to eat mostly pureed foods. You can only consume warm food, eat 6 times a day. The last meal is taken before bed.
The diet includes, among other things: dried wheat bread, jelly, baked apples, low-fat broths, lean fish and meat, steamed cutlets, vegetable purees.
4.Treatment
The therapeutic strategy for DSO is aimed at normalizing the movement and outflow of biological fluids, sphincter tone and kinetics, the composition of bile and intestinal microflora. Tactics are determined by the clinical picture and diagnostic data; it usually includes three components: optimization of the regimen, diet and drug treatment, and the first two components are much more important and more effective than the third (and not vice versa, as many “lazy” patients are accustomed to believe). As a rule, frequent split meals, a special diet (prescribed by a doctor on a strictly individual basis), and antispasmodic drugs are indicated. To relieve pathological phenomena in the intestines, an optimal regimen of antibacterial correction (ciprofloxacin, metronidazole, biseptol, tetracycline, etc.) is selected (usually experimentally), after which the use of probiotics is indicated - drugs with normal intestinal microflora. You may need to correct stool frequency, take antacids and enzyme medications, etc.
In case of stenosis (pronounced narrowing of the lumen) of the sphincter of Oddi, in cases of ineffectiveness of conservative treatment, and with frequent relapses of pancreatitis, the question of repeated surgical intervention may be raised. However, in most cases, subject to complete and not selective compliance with medical prescriptions, the prognosis is quite favorable: combination therapy for postcholecystectomy dysfunction of the sphincter of Oddi is successful.
List of sources
- Burkov S.G. About the consequences of cholecystectomy or postcholecystectomy syndrome // Appendix gastroenterology // Consilium medi-cum. 2004. T.6, No. 1. pp. 1-8.
- Grigoriev P. Ya., Soluyanova I. P., Yakovenko A. V. Gallstone disease and consequences of cholecystectomy: diagnosis, treatment and prevention // Attending physician. 2002. - No. 6. pp. 26-32.
- Minushkin O. N., Guseva L. V., Burdina E. G., Vasilchenko S. A., Gurova N. Yu., Kononova T. N. Patients after removal of the gallbladder. Is it always postcholecystectomy syndrome? Medical advice. 2016;(14):122-128.
- Surgical diseases Textbook for students of higher medical educational institutions // Ed. A. F. Chernousova - M. GEOTAR-Media. 2010.
Gallstone disease (GSD) and PCES
Cholelithiasis is one of the most common diseases and is in third place after cardiovascular pathologies and diabetes mellitus. About 10-15% of the adult population in developed countries suffers from this disease. In Russia, about one million people annually visit clinics for the treatment of cholelithiasis. For this reason, cholecystectomy ranks second among surgical procedures (first place is appendectomy).
In Russia, about 7,000 operations are performed annually per hundred thousand people, and this figure is increasing.
Minimally invasive methods are used to remove the gallbladder, in particular laparoscopy. In rare cases, when minimally invasive surgery cannot be used, abdominal surgery is performed.
Due to the constant increase in the number of patients with cholelithiasis, the number of operations performed is also increasing, and with it the complications that arise after surgery.
According to some data, 1-3 out of 10 patients who have undergone surgery continue to experience discomfort from the gastrointestinal tract: pain, disturbances in the digestive process. These symptoms are collectively called postcholecystectomy syndrome. Typically, relapse occurs within the first year after cholecystectomy, but in some cases symptoms of PCES may appear at a later date.