Tumors of the retroperitoneal space are a group of formations that are located in the depths between the lumbar muscles and the organs of the peritoneal cavity. They can be benign (lipoma, teratoma, lymphangioma, etc.) or malignant. Tumors or cysts can originate from various tissues of the retroperitoneal space: fatty, connective, muscle, nervous, originate from lymph nodes or blood vessels, embryonic elements or nerves, etc.
Tumors of the retroperitoneal space of malignant origin (liposarcoma, fibrosarcoma, neurolemmoma, lymphangiosarcoma, etc.) are not so common, they account for up to 0.3% of all tumors. The disease is more often diagnosed after 50 years of age and can occur equally in men and women.
Causes
At the moment, the causes of the development of retroperitoneal tumors have not been fully established. However, there are a number of factors contributing to their appearance:
- genetic abnormalities;
- exposure to harmful radiation or chemicals (such as herbicides or pesticides);
- suppression of the immune system due to the toxic effects of chemicals.
There is a version that the disease develops in patients who have undergone radiation during treatment for cancer.
To determine the type of retroperitoneal cyst, its localization to the main structures of the organ and indications for surgery, as well as choosing the correct surgical treatment tactics, you must send me a complete description of the ultrasound of the abdominal cavity, MSCT data of the retroperitoneal space with contrast, indicate your age and main complaints to your personal email address . Then I will be able to give a more accurate answer to your situation.
Peritoneal tumors
Benign peritoneal tumors
They are a very rare pathology. The reasons for the development are unknown. The disease can be asymptomatic for years. In some cases, peritoneal tumors reach enormous sizes without significantly affecting the patient’s condition. The literature describes a case of removal of an omental lipoma weighing 22 kilograms. With large nodes, an enlarged abdomen is detected. Sometimes benign tumors of the peritoneum cause compression of nearby organs. Pain is uncharacteristic. Ascites occurs extremely rarely. The diagnosis is made based on the results of laparoscopy. The indication for surgery is the compressive effect of the tumor on neighboring organs.
Primary malignant tumors of the peritoneum
Peritoneal mesotheliomas are rare. Usually found in men over 50 years of age. A risk factor is prolonged contact with asbestos. They manifest themselves as pain, weight loss and symptoms of compression of nearby organs. With sufficiently large peritoneal tumors, an asymmetric protrusion in the abdominal area may be detected. On palpation, single or multiple tumor-like formations of various sizes are detected.
Characterized by rapid progression of symptoms. When the portal vein is compressed, ascites develops. Due to the lack of specific signs, the diagnosis of malignant peritoneal tumors is difficult. Often, the diagnosis is made only after excision of the tumor and subsequent histological examination of the removed tissue. The prognosis is unfavorable. Radical removal is possible only with limited processes. In other cases, patients with peritoneal tumors die from cachexia or from complications caused by dysfunction of the abdominal organs.
Pseudomyxoma peritonei
Occurs when an ovarian cystadenoma, pseudomucinous cyst of the appendix, or intestinal diverticulum ruptures. Mucus-producing epithelial cells spread across the surface of the peritoneum and begin to produce a thick, jelly-like fluid that fills the abdominal cavity. Typically, the rate of development of this peritoneal tumor corresponds to a low degree of malignancy. The disease progresses over several years. The jelly-like liquid gradually causes fibrotic changes in tissue. The presence of mucus and tumor formation interferes with the activity of internal organs.
Less commonly, high-grade peritoneal tumors are detected that are capable of lymphogenous and hematogenous metastasis. If left untreated, death occurs in all cases. The cause of death of patients is intestinal obstruction, exhaustion and other complications. The presence of a mucus-forming tumor of the peritoneum is indicated by an increase in the size of the abdomen with a decrease in body weight, digestive disorders and jelly-like discharge from the navel.
The diagnosis is established on the basis of CT, laparoscopy, histological and immunohistochemical studies. For malignant tumors of the peritoneum, positron emission tomography can be used. For a benign variant of the disease, this study is not informative. Treatment tactics for peritoneal tumors are determined individually. In some cases, surgical excision of the affected areas in combination with intraperitoneal intracavitary chemotherapy is possible. With timely initiation of treatment, the prognosis is quite favorable, especially for low-grade peritoneal tumors.
Single secondary malignant tumors of the peritoneum
The lesion occurs when the germination of malignant tumors located in organs partially or completely covered by the peritoneum. The appearance of peritoneal tumors is accompanied by increased pain and deterioration of the patient's condition. Palpation of the abdomen may reveal tumor-like formations. When a lesion in a hollow organ (stomach, intestine) disintegrates, the phenomena of perforated peritonitis are observed. In some cases, the primary tumor simultaneously grows into the wall of a hollow organ, the layers of the peritoneum and the anterior abdominal wall. When the resulting conglomerate disintegrates, soft tissue phlegmon occurs.
Peritoneal tumors are diagnosed based on medical history (there is a malignant neoplasm of an organ covered by the peritoneum), clinical manifestations, abdominal ultrasound data and other studies. With a limited process, radical excision of the primary tumor along with the affected area of the peritoneum is possible. In the presence of distant metastases, symptomatic therapy is carried out. Patients with peritoneal tumors are prescribed painkillers; if fluid accumulates in the abdominal cavity, laparocentesis is performed, etc. The prognosis depends on the extent of the process.
Peritoneal carcinomatosis
Malignant cells entering the abdominal cavity quickly spread throughout the peritoneum and form multiple small foci. At the time of diagnosis of stomach cancer, peritoneal carcinomatosis is detected in 30-40% of patients. In ovarian cancer, secondary peritoneal tumors are found in 70% of patients. The pathology is accompanied by the appearance of profuse effusion in the abdominal cavity. Patients are exhausted, weakness, fatigue, stool disorders, nausea and vomiting are detected. Large peritoneal tumors may be palpable through the abdominal wall.
There are three degrees of carcinomatosis: local (one affected area is detected), with damage to several areas (the affected areas alternate with areas of unchanged peritoneum) and widespread (multiple secondary peritoneal tumors are detected). With an undiagnosed primary tumor and multiple peritoneal nodes, clinical diagnosis in some cases is difficult due to the similarity with the picture of tuberculous peritonitis. Secondary tumors of the peritoneum are supported by the hemorrhagic nature of the effusion and the rapid reappearance of ascites after laparocentesis.
The diagnosis is established taking into account the history, clinical manifestations, ultrasound data of the abdominal organs, MSCT of the abdominal cavity with contrast, cytology of ascitic fluid obtained during laparocentesis, and histological examination of a sample of peritoneal tumor tissue taken during laparoscopy. As an additional diagnostic technique, a tumor marker test can be used to more accurately determine the prognosis, timely detect relapses and evaluate the effectiveness of therapy.
If it is possible to completely remove the primary neoplasm and peritoneal tumors, radical operations are performed. Depending on the location of the primary lesion, peritonectomy is performed in combination with colectomy, gastrectomy or gastrectomy, panhysterectomy and other surgical interventions. Due to the danger of contamination of the abdominal cavity with cancer cells and the possible presence of visually undetectable peritoneal tumors during or after surgery, intraperitoneal hyperthermic chemotherapy is performed. The procedure allows for a powerful local effect on cancer cells with minimal toxic effects of chemotherapy on the patient’s body.
Despite the use of new treatment methods, the prognosis for disseminated secondary peritoneal tumors still remains unfavorable. Carcinomatosis is one of the main causes of death in patients with cancer lesions of the abdominal cavity and pelvis. The average survival rate of patients with stomach cancer in combination with peritoneal tumors is about 5 months. Relapses after radical surgical interventions for secondary peritoneal tumors occur in 34% of patients. Experts continue to search for new, more effective methods of treating secondary peritoneal tumors. New chemotherapy drugs, immunochemotherapy, radioimmunotherapy, gene antisense therapy, photodynamic therapy and other techniques are used.
Symptoms
The disease can be asymptomatic for a long time, without disrupting the functioning of nearby organs. The first symptom of a retroperitoneal tumor, with which a patient first consults a doctor, is abdominal pain: from mild - dull and aching, to paroxysmal and intense.
But there are no specific signs; the manifestations are caused not by the type of tumor, but by its localization - in the upper, lower or lateral part of the retroperitoneal space, the proximity of nerves, blood vessels, lymphatic pathways, etc. However, disruption of the functioning of nearby organs develops when the formation reaches an impressive size and begins to compress nearby structures.
Nausea and vomiting, alternating diarrhea with constipation, rumbling and bloating may occur. When the bladder is compressed, urinary dysfunction occurs, and when pressure is placed on the diaphragm, shortness of breath occurs. In some cases, signs of hypothermia and hyperhidrosis of the lower limb - excessive sweating - may appear on the affected side. Compression of large vessels of the retroperitoneal space by the tumor leads to edema of the lower extremities.
During the malignant process, the following are noted: loss of appetite, nausea, fatigue, and at a later stage - weight loss, fever. Tumors of the retroperitoneal space of a malignant nature can metastasize, most often metastases are found in the liver and lungs.
Acute stomach
In making a diagnosis of acute abdomen, a correctly collected anamnesis in combination with a competent physical examination is of great importance. It is important to find out whether the pain developed acutely (perforation of a hollow organ) or whether the pain syndrome gradually intensified (peritonitis); whether the pain is localized in one place or migrates; Is the pain associated with eating? Vomiting indicates a violation of the passage of food through the intestines of a mechanical or reflex nature (intestinal obstruction, colic). You should definitely find out whether there have been any recent changes in the nature and frequency of stool, whether there were any pathological impurities in the stool (blood, mucus in the form of “raspberry jelly”, etc.).
During the examination, close attention is paid to the state of the cardiovascular system (heart rate, blood pressure) for timely diagnosis of bleeding and shock. When examining the abdomen, its shape is assessed (sunken or scaphoid, tense - with perforation of the stomach, intestines; overinflated and asymmetrical - indicates intestinal obstruction), cicatricial changes and hernia defects are identified. Palpation allows you to detect criteria for peritoneal irritation, space-occupying formations in the abdomen, and localize the source of pain. With percussion, you can determine the expansion of the borders of the liver, the presence of free gas or effusion in the abdominal cavity. When listening to the abdomen, intestinal sounds either increase significantly (in the initial phases of intestinal obstruction) or are not heard at all (in the peak phase of obstruction).
All patients with suspected acute abdomen should undergo a rectal examination. It is necessary to focus on the exacerbation of pain when pressing with a finger on the walls of the rectal ampulla (this indicates the presence of effusion in the pelvis). If even small hernial protrusions are detected in a patient, it is recommended to conduct a digital examination through the hernia gate. When using this technique, direct irritation of the parietal layer of the peritoneum occurs, so pain and tension in the abdominal wall will be more pronounced. In children, it is useful to palpate the abdominal organs in a state of sleep or sedation, when involuntary tension of the abdominal wall can be excluded.
Laboratory tests for an acute abdomen are uninformative; they reveal purulent-inflammatory changes and anemia. One of the simplest and most accessible methods for verifying a catastrophe in the abdomen is plain radiography of the abdominal cavity. For patients in extremely critical condition, photographs are taken in a horizontal position (in a lateral projection); in other cases, radiography is performed in a vertical position. The images visualize free gas in the abdominal cavity, darkening in sloping areas (exudate), arches and levels in intestinal loops, gas in the retroperitoneal tissue. An extended diagnostic search includes X-ray contrast studies: gas and a contrast agent are injected into the stomach or intestines. If air or contrast enters the free abdominal cavity, this indicates perforation of a hollow organ. If, when contrasting the stomach, its displacement anteriorly is noted, one can think about pancreatic necrosis. Sometimes a specialized X-ray examination (celiacography, mesentericography) may be required.
Ultrasound of the abdominal cavity will reveal exudate in the abdominal cavity, gas in the portal vein system, tumor conglomerate, intussusception and other pathological conditions that could cause acute surgical pathology. Ultrasound is the leading method for diagnosing acute urological and gynecological pathologies. In difficult situations, diagnostic laparoscopy will help establish the correct diagnosis.
If a patient is suspected of having an acute abdomen, care must be taken to rule out conditions that mimic an abdominal catastrophe. An operation performed on a patient with severe somatic pathology often leads to a deterioration in his condition and death. That is why, upon admission to the emergency room, it is necessary to exclude non-surgical factors of an acute abdomen: myocardial infarction (ischemia), pneumonia, pleurisy, pneumothorax, urolithiasis and cholelithiasis (colic), intestinal infections.
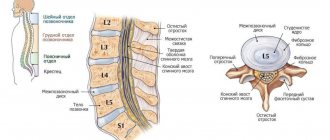
Diagnostics
In addition to laboratory tests (general tests, stool tests for occult blood, coagulograms, hormonal tests, analysis for tumor markers, etc.), instrumental diagnostic methods are prescribed:
- Ultrasound of the abdominal organs and retroperitoneal space, the purpose of the examination is to clarify the location and size of the formation, the presence of germination into neighboring structures, etc.;
- MRI or CT - necessary to clarify the extent of the process, including to detect metastasis;
- PET is a sensitive and informative method that allows you to identify micrometastases and small tumors.
X-ray, urography, irrigoscopy and other instrumental diagnostic methods for tumors of the retroperitoneal space are prescribed according to indications to confirm or exclude involvement of other organs in the process: lungs, intestines, genitourinary system, etc.
Abdominal pain: differential diagnosis, possible treatment approaches
P
The problem of abdominal pain exists because pain can accompany an extremely large number of diseases. The cause of abdominal pain is one of three broad nosological groups:
- diseases of the abdominal organs
(including acute ones requiring urgent surgical intervention); - radiating pain in diseases localized outside the abdominal cavity
(this is the so-called pseudo-abdominal syndrome (PAS) - a symptom complex that includes manifestations reminiscent of the clinical picture of an “acute abdomen”, but is formed by the pathology of other organs - the heart, lungs, pleura, endocrine organs, intoxication , some forms of poisoning, etc.); - systemic diseases
.
Since this large group of diseases includes those that require surgical treatment, the symptom of pain will always be considered urgent, at least until “acute surgical pathology” is rejected or confirmed, which in general in Moscow In recent years, there has been an upward trend (B.S. Briskin et al. 2002).
The abdominal organs are usually not sensitive to many stimuli that, when applied to the skin, provoke severe pain. Cuts, tears or other injuries to the internal organs of the abdominal cavity do not cause pain. The main influences to which visceral pain fibers are sensitive are stretching or disruption of the intestinal wall. This may be: tension in the peritoneum (for example, with a tumor), stretching of a hollow organ (for example, with biliary colic) or strong muscle contractions (for example, with intestinal obstruction). The nerve endings of the fibers responsible for pain in the hollow organs (intestines, gall bladder, bladder) are localized in the muscle layers. In parenchymal organs (liver, kidneys, spleen), the nerve endings are located in their capsule and respond to its stretching as the volume of the organ increases. The mesentery, parietal pleura, and peritoneal lining of the posterior abdominal wall are sensitive to pain, whereas the visceral pleura and greater omentum are not. For pain to appear, the rate of increase in tension must be sufficiently large. A gradual increase in tension, for example, such as with tumor obstruction of the biliary tract, can proceed painlessly for a long time.
Inflammation and ischemia can also cause visceral pain, while inflammation can increase the sensitivity of nerve endings and reduce the threshold of sensitivity to pain from other stimuli (including during the development of one disease in its different phases). Many biological active substances (bradykinin, serotonin, histamine, prostaglandins, etc.) are involved in the mechanisms of occurrence and progression of pain during inflammation.
The briefly listed pathophysiological mechanisms of the formation of abdominal pain are the initial difficulty, often leading to late, at best, delayed diagnosis. That's why revisiting this issue is always important and useful.
“acute abdomen” should be confirmed
, which refers to conditions that occur over several hours or days and are characterized by limited or diffuse phenomena of peritoneal irritation. In the first hours and sometimes days of observation of such patients, a group of those in need of surgical treatment is identified. Patients who do not need surgical treatment should be referred to therapists, cardiologists, pulmonologists, gastroenterologists, etc. That is why it is hardly advisable to consider the term “acute abdomen” a purely surgical concept, especially since most patients end up in need of non-surgical treatment.
Since the main symptom of the “acute abdomen” symptom complex is pain, the main diagnostic technique for finding out its cause is the method of differential diagnosis.
First group
constitute intra-abdominal focal purulent inflammatory processes and their complications.
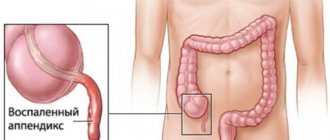
Acute appendicitis
. Regardless of the initial localization of pain, in the future, in the vast majority of patients, pain and symptoms of peritoneal irritation are localized in the right lower abdomen, increasing leukocytosis and an increase in ESR are recorded. If there is no tendency to normalize these indicators and if symptoms increase, laparotomy is indicated. It is also necessary to keep in mind the left-sided localization of the process with the complete reverse arrangement of the organs.
Suppuration of cysts and diverticula
vermiform appendix: there are no clinical signs that distinguish this pathology from acute appendicitis, but they may appear during an urgent ultrasound examination.
Cholecystitis, empyema and hydrocele of the gallbladder
. Localization of pain in the right upper abdomen with or without symptoms of peritoneal irritation. Leukocytosis with a shift of the formula to the left and an increase in ESR. With exacerbation of chronic cholecystitis in the elderly, with blockage of the cystic duct without signs of inflammation, these signs may be absent. The same symptoms can also be demonstrated by acute appendicitis (with a significant length and location of the appendicitis).
The most reliable diagnostic technique in this situation is ultrasound, since X-ray examination in acute and exacerbation of a chronic process is ineffective.
Diverticulitis
. Mainly in the sigmoid colon; soreness and symptoms of peritoneal irritation, mainly in the left lower abdomen. Elderly people suffering from pathology of the large intestine are more often ill; exacerbation is often preceded by persistent constipation (rarely relief). There are often symptoms of partial intestinal obstruction and blood in the stool. Colonoscopy and irrigoscopy are contraindicated in this situation. History, clinical observation and dynamic ultrasound examination are the most adequate diagnostic techniques.
Acute adnexitis
. Symptoms of peritoneal irritation are minor. According to clinical and laboratory data, it can be similar to any acute focal pathology. The most adequate diagnostic technique is ultrasound; if ineffective, laparoscopy.
In the presented group of diseases (especially at an early stage), it should be noted the predominance of local symptoms over general disorders. In the complicated stage of the disease - when local manifestations stabilize, general disorders and intoxication begin to increase and come to the fore.
Peritonitis (acute, chronic).
- Due to perforation of inflammatory, purulent-inflammatory, ulcerative processes and trophic
(including ischemic)
disorders of the gastrointestinal tract:
appendix, gallbladder, colon diverticulum (appendix cyst), pancreatic cyst, genital organs in women. At the same time, the pain becomes diffuse, the symptoms of intoxication increase; caused by an ulcerative process in the gastrointestinal tract: stomach and duodenal ulcers, simple ulcers of the small intestine, colon ulcers with nonspecific ulcerative colitis, ulcers of the small intestines with typhoid fever, which has reappeared. Often, anamnestic data answer the question of the cause. Diagnosis is based on the detection of fluid and free gas in the abdominal cavity (ultrasound and plain fluoroscopy), caused by acute destructive pancreatitis. The most important diagnostic techniques are ultrasound (especially in dynamics) and laparoscopy, which can also be a therapeutic procedure. - Due to traumatic injuries and injuries of hollow organs, postoperative complications:
anamnestic data, dynamic observation of the patient, monitoring laboratory tests of inflammation, hemoglobin. - Tuberculous peritonitis:
diagnosis is extremely difficult. It helps to detect adhesions in the abdominal cavity in the absence of any significant pathology of the internal organs. The diagnosis becomes proven when a morphological substrate is detected (during laparoscopy), but there are forms without tuberculosis tubercles - then serological diagnosis and ex juvantibus therapy with antituberculosis drugs can help. X-ray examination may reveal calcified lymph nodes; provocative tests are used. - Syphilitic peritonitis:
damage to the peritoneum, severe perivisceritis with serologically proven syphilis. If there is fluid in the abdominal cavity, it is hemorrhagic in nature. - Actinomycosis of the peritoneum:
the diagnosis is very difficult, but may be realistic when there is actinomycosis of the internal organs. The damage to the peritoneum is about 30%. In most cases, the clinical picture becomes significant with the development of a “secondary” infection of the abdominal cavity. - Parasitic diseases of the peritoneum:
they are rare and occur, as a rule, with perforation of hollow organs and cysts with pathogens entering the abdominal cavity. - Ascites-peritonitis
(in patients suffering from liver pathology in the stage of liver cirrhosis with severe portal hypertension). Suspicion of peritonitis should arise whenever ascites becomes resistant to therapy, if it is adequate from a pathogenetic point of view. An early form of diagnosis is the study of ascitic fluid for the presence of volatile fatty acids (they always indicate the presence of bacterial inflammation).
This group of diseases is clearly divided into two subgroups: the first is acute peritonitis, in the diagnosis of which the previous history plays a major role (with the exception of the onset of peptic ulcer disease in young people); the second is chronic forms of peritonitis, the diagnosis of which is extremely difficult. The situation is easier if the underlying disease is known and its continuation or complication is a process in the abdominal cavity.
Intestinal obstruction (acute, chronic)
.
According to the mechanism of development: mechanical
(adhesive, due to strangulation of a hernia, tumor, intussusception - more often in children).
In adults, intussusception is often caused by intestinal polyps, ulcerative scars, or blockage of the lumen by foreign bodies (gallstones, bezoars, etc.). With obstruction, the pain is cramping; with strangulation, along with contractions, the pain is constant (often shock); paralytic
(due to a disorder of innervation and blood supply to the intestinal wall), intoxication, due to thrombosis and embolism of mesenteric vessels, mesenteric infarction, after severe operations, with peritonitis, with severe infections, neuroreflex;
medicinal
– in treatment with ganglion blockers, b-blockers in large doses, etc.
In the diagnosis of this group of patients, a thorough analysis of anamnestic data (including medications) and the general condition of the patient, in particular, vascular lesions in elderly and old people suffering from heart and vascular diseases, leading to thrombosis and embolism of the mesenteric veins, is of great importance. In this case, an important diagnostic sign is bloody liquid stools. This group of patients is the most prominent and understandable in practical terms. Chronic (or partial) intestinal obstruction deserves special attention, which is often an early symptom of tumor obstruction and requires a very careful examination of the patient with the mandatory use of colonoscopy. No less important is the group with drug-induced paralytic obstruction, and in this regard the drug history is leading, which allows avoiding unnecessary surgical intervention.
Diseases that begin with pain and are accompanied by the development of jaundice:
a) acute and chronic calculous cholecystitis;
b) choledocholithiasis;
c) acute or exacerbation of chronic pancreatitis;
d) progressive stenosis of the terminal part of the common bile duct;
e) cancer of the gallbladder, common bile duct and pancreas;
f) liver diseases: acute and exacerbation of chronic hepatitis, liver cirrhosis, primary sclerosing cholangitis, metastatic liver.
The main symptom analyzed is jaundice. Of the laboratory tests, the determination of alkaline phosphatase is most important for suspecting its mechanical nature. A further research program clarifying the nature and pathogenesis of jaundice should be structured as follows:
Ultrasonography
(detecting biliary hypertension - ductal and intrahepatic; often the level of obstruction is also determined. It can not only open the research program, but also complete it).
Endoscopy of the upper gastrointestinal tract
(relative signs of damage to the pancreas, damage to the papilla of Vater, tumors of the stomach and duodenum, parafateral diverticulum with symptoms of diverticulitis can be obtained).
Retrograde cholangiopancreatography
(damage to the pancreatic, common bile and hepatic ducts, stones in them, obstructive pathology).
Laparoscopy
(has an advantage in cases where previous methods have not made it possible to clarify the diagnosis, and the clinical picture of the disease indicates an increase in the acute process - surgery becomes inevitable. With the help of laparoscopy, it is often possible not only to establish the level of obstruction, but also to unload the biliary system (drain the gallbladder, considering this as the first stage of the operation, drain the lesser omental bursa, etc.).
The validity of the existence and identification of this group of patients admitted to the clinic with a diagnosis of “acute abdomen” is beyond doubt, because the symptom of jaundice in patients in this group appears later.
Second group
diseases are diseases of organs outside the abdominal cavity, but forming a symptom complex similar to an “acute abdomen” - the so-called. “pseudo-abdominal syndrome” (PAS).
Thus, diseases of the chest organs that form the PAS are associated with the common innervation of the chest and anterior abdominal wall (spinal nerves for the parietal peritoneum of the upper 2/3 of the abdominal cavity (DX-L1) in their initial part pass in the chest, and acute heart disease , lungs and pleura in the first hours, in the absence of physical and auscultatory data, can be interpreted as an acute disease of the abdominal organs. “Referred pain” plays a certain role in the formation of PAS (zones of hyperalgesia G.A. Zakharyin, 1885; Geda , 1888); irritation of the phrenic, sympathetic and vagus nerves involved in the formation of the solar plexus; in case of pneumonia, as a result of the toxic effect on the nervous system of the “intestinal tube”, paralysis of the gastrointestinal tract of varying intensity may occur; acutely developed congestive heart failure by systemic circulation in general and acute stretching of the Glissonian capsule in particular.In kidney diseases, PAS develops due to the common innervation and reflex connections between the renal-ureteric nerve plexus and the gastrointestinal plexus.
Since the main symptom of PAS is pain, the main diagnostic technique for finding out its causes is the method of differential diagnosis. The research program is formed depending on the symptoms included in a particular syndrome. The main symptoms of PAS, in addition to pain, may include:
- increasing anemia
- drop in blood pressure
- increase in body temperature
- persistent constipation
- vomit
- diarrhea
- change in urinary sediment
- jaundice
- changes in the biochemical spectrum of blood.
Thus, acute abdominal pain and fever can occur with acute pneumonia, basal pleurisy, acute pericarditis, rheumatic carditis, thyrotoxic crisis, periodic illness, non-suppurating panniculitis (Weber-Christian disease - visceral cutaneous, visceral, abdominal variants), acute mesadenitis , pyelonephritis, herpes zoster, hemorrhagic vasculitis and inflammatory diseases of the abdominal organs; acute abdominal pain and a drop in blood pressure - observed in acute myocardial infarction, acute pancreatitis, dissecting hematoma of the abdominal aorta, acute adrenal insufficiency, rupture of a tubal pregnancy, perforation of a gastric ulcer, acute disturbance of mesenteric circulation, etc. Each symptom complex makes it possible to limit the range of nosological forms and make the diagnosis probable, and since each symptom complex includes acute diseases of the abdominal organs, the research program should be structured in such a way as to either confirm them or reject them. In all cases, after conducting a generally accepted study, the use of instrumental methods should begin with ultrasound, which should be carried out as follows:
- “Exploratory examination - floor by floor” (upper, middle, lower abdomen. This determines the pathology of the gallbladder, pancreas; free fluid in the abdominal cavity; determination of the diameter of blood vessels - inferior vena cava, aorta; determine the pathology of the kidneys (stones, incl. including ureter, kidney carbuncle) or reject it; establish pathology of the uterus, appendages, some rare changes, etc.
- Taking into account the results of the exploratory examination, a detailed study of the pathological focus should be carried out. In a certain clinical situation, it is possible to search for abscesses, subhepatic and suprahepatic infiltrates and ulcers. If jaundice is present, determine its nature (mechanical, parenchymal; if there is hepatomegaly, then determine or reject its “stagnant” nature.
The second, most logical method of investigation (if the diagnosis remains unclear) should be considered “emergency laparoscopy”. The method allows for differential diagnosis of acute appendicitis, acute cholecystitis, perforated gastroduodenal ulcer, acute pancreatitis, intestinal infarction, and acute diseases of the pelvic organs. In this case, if there are indications, drainage of the abdominal cavity, omental bursa, and cholecystectomy can be performed simultaneously. These two instrumental studies, as a rule, are sufficient to confirm or reject an “acute abdomen”, confirm the diagnosis of PAS, largely determine its cause and choose the most rational path for further diagnosis (ECG, EchoCG; X-ray examination, CT; special laboratory, serological, morphological studies - in specialized hospitals).
Third group
diseases that cause abdominal pain are: systemic diseases; general diseases that occur with severe intoxication; chronic and acute intoxication; some forms of functional disorders that occur with pain (irritable bowel syndrome - a variant that occurs with “bloating”).
When considering this group of diseases, you should keep in mind:
Precomatose states
in patients with diabetes mellitus (hyperglycemia, acetouria, hypoglycemia).
Thyrotoxic crisis
. Increased body temperature to febrile levels, hyperemia and cyanosis of the skin, especially the cheeks, neck and limbs, tachycardia up to 150–160 beats per minute, increased pulse pressure, increased breathing, the appearance or worsening of mental disorders. Very often, abdominal pain occurs, accompanied by vomiting and diarrhea, which is the reason for the diagnosis of acute abdomen. Often a thyrotoxic crisis is accompanied by jaundice, which is a sign of increasing liver failure. A screening test for thyrotoxic crisis can be determined by determining the concentration of protein-bound iodine (BPI) in the blood plasma, which, being elevated during thyrotoxicosis, increases sharply during a crisis. The second test is ex juvantibus therapy: intravenous administration of thyroid hormone synthesis blockers - thiamazole at a dose of 100 mg and b-blockers at a dose of 2-10 mg (effect about 3-4 hours).
Hypothyroid coma:
a) “intestinal form”
, is formed due to atony of intestinal smooth muscles;
b) “gallbladder”
– due to atony of the gallbladder, which results in the formation of a clinical picture of hepatopancreatic syndrome.
Diagnosis is aided by identifying hypercholesterolemia, reducing the level of SBI below 3.5 mg%; from clinical data - low blood pressure, bradycardia, hypothermia, decreased breathing, oliguria-anuria.
Chronic adrenal insufficiency
(crisis): pigmentation of the skin and mucous membranes attracts attention; As a rule, there are always provoking moments.
Lead toxicity
. The abdomen may be tense, but still palpable; There are no signs of peritoneal irritation. In diagnosis, it is necessary to take into account medical history, look for a “lead” border, basophilic punctuation of red blood cells, pay attention to the excretion of coproporphyrin in feces, increased excretion of lead in feces and urine. The serious condition of the patient in the absence of instrumentally obtained signs of pathology (including ultrasound, etc.) is important.
Porphyria
(acute intermittent). Abdominal colic, muscle paresis, tachycardia, fever, high-amplitude arterial hypertension; urine is reddish followed by darkening - this important phenomenon is almost always “obtained” by accident. Young people (usually women) are affected, and the disease manifests itself soon after puberty (20–30 years). In diagnosis, it is important to remember that urobilinogen, uroporphyrin, and porphobilinogen are always determined.
Secondary porphyria
(the classic picture is based on paresis of the capillaries of the abdominal cavity). Only corpoporphyrin is detected.
Waist poisoning
. Severe abdominal pain, recurrent vomiting, diarrhea - like “rice water” mixed with blood, dehydration, blood thickening, oliguria, anuria. In diagnosis, one should especially take into account medical history and the use of mouse poison. In general, diagnosis is extremely difficult, and time is limited, therefore, if suspected, unithiol should be administered, orally - an aqueous suspension of burnt magnesia and activated carbon, to combat dehydration and collapse.
Tetany
(develops with a decrease in calcium levels, two clinical variants are known: the first - with difficulty breathing like suffocation and the second - with abdominal pain associated with intestinal paresis (expressed to varying degrees). In diagnosis - Chvostek’s symptom, prolongation of the Q-T interval on the ECG, a decrease in calcium levels.Clinical manifestations are relieved by intravenous administration of a calcium solution.
Essential hyperlipidemia
.
Easily reproduces the clinical picture of an “acute abdomen” of any variant (right hypochondrium, left hypochondrium; hepatosplenomegaly). Diagnosis is simple - the whey has a “milky appearance” with a high fat content.
Chronic renal failure.
Hemochromatosis.
Hemolytic anemia.
In general, their diagnosis is not difficult; the main and necessary condition is a reminder that they should be included in the circle of nosological forms that are similar in symptoms.
Systemic vasculitis
(abdominal variant of nodular arteritis, capillary toxicosis). When diagnosing them, it should be remembered that hemorrhagic rashes can also be on the skin; high arterial hypertension, arthralgia, bloody vomiting, blood in the stool and the absence of organic changes are noted during a program examination.
Weber-Christian disease
(non-suppurating panniculitis). The main substrate of the disease is adipose tissue, in which aseptic infiltrates are formed from time to time, followed by their dynamics and the formation of a “retracted scar” on the skin - this is the visible part of the disease. There is a cutaneous variant; cutaneous-visceral; visceral (thoracic and abdominal). The path to diagnosis is difficult, often through repeated laparoscopy. Diagnosis requires a biopsy of the omentum, adipose tissue that is suspicious for “unusuality.”
Tabes
. Knowing it has recently acquired a certain meaning, because syphilis is growing steadily. If analysis of abdominal pain raises suspicion of the presence of tabes dorsalis, other symptoms of this suffering should be looked for: ocular symptoms (anisocoria, ptosis, reflex immobility); impaired reflexes (lowered knees, absent); ataxia phenomena; optic nerve atrophy.
The diagnosis of tabes is absolutely reliable in the presence of 4 symptoms and is very likely in the presence of 3. Laboratory confirmation requires the Wasserman reaction and cerebrospinal fluid examination.
Periodic illness
(abdominal version). Suspicion should always arise when it comes to the peoples of the Mediterranean. At the height of the disease, lymphocytosis can be detected in the blood, an adhesive process in the abdominal cavity in the absence of visible causes; Colonoscopy shows “pale swelling” of the colon mucosa.
Functional disorders
, which have recently developed into “irritable bowel syndrome”.
Unlike other dyskinetic disorders, it always occurs with pain - this is its difference. Most often, patients are admitted to the surgical hospital with a variant characterized by pain and bloating of the abdomen, and its bloating can be paroxysmal. Diagnosis is carried out by excluding organic pathology and the absence of laboratory changes. In the treatment of functional disorders, “antispasmodics” are used, because pain is largely formed due to spasm. Of the drugs that have attracted attention recently, it should be noted Duspatalin (mebeverine)
, which in therapeutic doses has a direct blocking effect on sodium channels. This reduces the influx of sodium and prevents the sequence of events that leads to muscle spasm (restricting the entry of calcium into the cell), which virtually eliminates the development of unwanted effects inherent in anticholinergic drugs that work through muscarinic receptors. We have experience in treating patients with irritable bowel syndrome and functional disorders of the gallbladder and biliary tract with Duspatalin, including comparative ones. The treatment effect, according to our data, was 90% and was confirmed by studying intestinal and gallbladder motility, which is very important in the absence of undesirable effects.
We are aware that the listed nosological forms are not a complete list of diseases that give a clinical picture of abdominal pain (“acute abdomen”), but still make up the majority of the diseases encountered, and we hope that the provided clinical, pathogenetic and diagnostic information will be useful for practicing doctors (generalist, gastroenterologist, surgeon).
Literature:
1. Smagin V.G., Minushkin O.N. – “Acute stomach”. Ter. archive No. 11, 1983, 86–91.
2. Minushkin O.N., Sokolov L.K., Savrasov V.M. and others - “The importance of ultrasound and x-ray methods in the diagnosis of acute surgical diseases of the abdominal organs.” Surgery No. 2, 1989, 28–32.
3. Briskin B.S., Vertkin A.L., Vovk E.I. and others - “Prehospital care for surgical diseases of the abdominal organs: acute abdominal pain.” Attending Physician, No. 6, 2002, 72–77.
4. Henderson D.M. – “Patophysiology of the digestive organs.” St. Petersburg, 19976 (translation from English)
5. Minushkin O.N., Elizavetina G.A., Ardatskaya M.D. – “Treatment of functional disorders of the intestines and biliary system, occurring with abdominal pain and flatulence.” Clinical pharmacology and therapy, 2002, 11, 24–26.
Treatment
The only effective treatment for retroperitoneal tumors is surgery. When choosing a technique, a number of factors are taken into account:
- localization of the tumor, its location relative to neighboring organs and vital structures;
- histological type of formation;
- spread to other organs and tissues.
For benign tumors of the retroperitoneum, surgery is performed within healthy tissue. In case of a malignant process, in the presence of metastases, surgical treatment can be supplemented with antitumor therapy.
Palliative treatment of peritoneal carcinomatosis
Unfortunately, even the most modern advances in medicine are not able to defeat some advanced forms of cancer. In such cases, the patient may be prescribed palliative or supportive treatment, the goal of which is not to completely remove foci of cancer from the body, but to improve well-being and alleviate the symptoms of the disease. With its help you can control:
- Pain.
- Abdominal bloating - ascites.
- Edema is the accumulation of fluid in tissues.
- Depression and anxiety.
- Weight change.
- Nausea and vomiting.
- Constipation.
- Loss of appetite.
- Fatigue and weakness.
Edema, lymphedema, ascites
Edema
is a common problem that cancer patients often face. They can be caused by salt and water retention in the body due to certain medications, damage to the heart, liver or kidneys, infection, poor diet, tumor growth or other reasons. If the lymph nodes, which act as “filters” that retain and neutralize dangerous substances, are affected by cancer or removed, patients may experience lymphedema, a serious swelling of the limb. It develops due to a violation of the circulation of lymph, which washes all the cells of the body, delivers necessary substances to them and takes away waste. These symptoms can be relieved by taking diuretics—diuretics that help the kidneys remove sodium and water—and limiting salt intake.
Ascites
– excessive accumulation of fluid in the abdominal cavity caused by damage to the tissues and lymph nodes located in them. It leads to an increase in the size of the abdomen, nausea, vomiting, increased fatigue and difficulty breathing. To improve the well-being of its owners, doctors may prescribe surgery or chemotherapy. In most cases, paracentesis is performed - draining excess fluid, which provides temporary relief for several weeks or days.
Difficulty breathing
Shortness of breath, or shortness of breath, is one of the most common symptoms of advanced cancer. It can be caused either by the disease itself or by its treatment. It is often caused by ascites, which restricts the movement of the diaphragm, the thin, dome-like muscle that separates the chest from the abdomen. Normally, during breathing, it moves up and down, allowing the lungs to increase and decrease in volume, but the accumulated fluid puts pressure on it and does not allow a person to receive enough oxygen. This extremely unpleasant sensation seriously affects quality of life, limits opportunities and worsens fatigue, anxiety and depression. Methods of treatment and relief of this condition depend on the cause that caused it. You can cope with mild shortness of breath on your own - just sit or lie down, raising your upper body at an angle of 45° with the help of pillows, inhale deeply through your nose and exhale slowly through pursed lips. Some patients benefit from various relaxation techniques, distraction by music, reading and television.
If you experience serious difficulty breathing, pale or blue discoloration of the skin, mucous membranes of the mouth and nail bed, pain, tightness and heaviness in the chest, problems with speech, dizziness or weakness, you should immediately seek medical help.
Intestinal obstruction
Tumors located in the abdominal cavity often block the intestines and prevent the passage of stool. This leads to severe cramping, abdominal pain and vomiting. This situation requires urgent intervention, since the contents accumulated in the digestive tract can damage its walls. It can escape through the hole into the abdominal cavity and cause a serious infection. In such cases, an operation is performed to install a stent - a small rigid tube that does not allow the lumen to narrow, or a colostomy - removal of a healthy part of the colon through an opening in the skin of the abdomen. If surgery is not possible, doctors remove the stomach contents using a special tube inserted through the nose.
Urinary tract obstruction
Some abdominal tumors block the ureters, which drain urine into the bladder. This blockage leads to fluid accumulation in the kidneys and disruption of their function. In such situations, specialists install stents or nephrostomy - they insert a flexible tube into the kidney, allowing its contents to flow into a special container - a reservoir located on the body.
Surgery for a tumor of the retroperitoneum
Depending on the location of the retroperitoneal tumor, removal can be performed using open surgery or through a laparoscopic approach. There are several types of incisions; access can be transperitoneal, extraperitoneal lumbar, abdominal-perineal, or perineal. Compared to open surgery, laparoscopy has great advantages.
- All actions are performed through several small incisions. Due to the absence of a large incision (as with an open approach), healing occurs much faster, hospitalization usually takes from two to five days.
- The ability to visualize when using video endoscopic equipment allows you to perform all manipulations as accurately as possible. The likelihood of damage to thin vascular structures, nerve fibers and other elements located in the operation area is practically absent.
- In the postoperative period, painful manifestations are either absent or minimal and short-lived, and can be easily relieved with analgesics.
- After 7-10 days, patients return to their normal lifestyle;
- After healing, only almost imperceptible puncture marks remain on the skin.
Author's technique for removing a retroperitoneal tumor
The critical stages of the operation are isolation of the tumor, establishment of its connection with surrounding organs and vital structures, revision and mobilization of the tumor. I always give preference to the laparoscopic approach, which is less traumatic and effective.
A special feature of my laparoscopy technique is the method I developed for installing trocars, which allows me to place surgical instruments at an optimal manipulation angle. Excision of pathological formations in this complex area is thus quick and safe.
During surgery, I also use modern ultrasonic scissors and a device for dosed electrothermal tissue ligation “LigaSure” (USA), which eliminates the need to use surgical threads and clips. The absence of bleeding in the surgical area ensures the safety of the intervention and maximum precision when manipulating the smallest structures. In the case of a primary retroperitoneal tumor and the presence of damage to adjacent structures, radical surgery is performed as a single block. The removed tissues are sent for histological examination, which is important for further treatment and prognosis.
I have been performing laparoscopic interventions since 1997; I have performed more than 200 operations to remove retroperitoneal tumors using laparoscopic access. Any patient who contacts me can count on my knowledge and experience. Based on the examination results, I select treatment tactics in such a way as to achieve the most effective result.
Treatment of peritoneal carcinomatosis
Fighting cancer that has spread throughout the body is a very difficult task. Until recently, the only method of influencing it was chemotherapy - taking or injecting into a vein special drugs that destroy rapidly dividing cells, including tumor cells. Unfortunately, most peritoneal cancers only shrink slightly in size or do not respond at all to such treatment.
Today doctors use the following tactics:
- Cytoreductive surgery
is the surgical removal of the maximum amount of affected tissue and altered cells. - Intraperitoneal hyperthermic chemoperfusion
, or
HIPEC
, is the injection of a chemotherapy agent heated to more than 40 degrees directly into the peritoneum. It requires expensive high-tech equipment, a well-equipped operating room and a whole team of doctors of various specialties. According to many researchers, the combination of cytoreductive interventions and HIPEC has revolutionized the treatment of carcinomatosis. The method has a number of contraindications that limit its use: The presence of metastases - additional cancerous tumors located outside the peritoneum. - The patient's general health is poor.
- A negative reaction to chemotherapy is the growth of a tumor or deterioration in health.
- A large number of lesions of the visceral peritoneum - the layer that envelops the internal organs.
is a complete or partial removal of the parietal peritoneum covering the inner surface of the abdominal wall.
of internal organs
damaged by oncology - for example, the uterus, its tubes, ovaries or affected parts of the intestine.
is the introduction of special drugs that affect only certain changes in cancer cells and cause virtually no harm to normal tissues.
For some patients with peritoneal carcinomatosis, the following may be suitable: Monoclonal antibodies:
deliver molecules that kill it to the tumor cell.
: prevent the growth of new vessels that the tumor needs for nutrition and further development.
substances that block the restoration of DNA of altered cells - molecules in which all information about the body is encrypted.
All such interventions are carried out only by experienced doctors in a specialized clinic. Any treatment for peritoneal carcinomatosis can be done at our oncology department. Our doctors are candidates and doctors of medical sciences with extensive experience in the fight against life-threatening tumors and extensive work experience in major federal institutions. We quickly carry out a complete diagnosis, take tests and receive their results from our own laboratory in the shortest possible time. In our center, all necessary procedures are performed using the most modern equipment using only original drugs that give predictable results.