Symptoms of the disease
As soon as the first symptoms of erosive gastritis are detected, treatment should begin as soon as possible, then their effectiveness will be most noticeable.
The main symptom of this pathology is a feeling of heaviness in the stomach, which occurs after each meal and does not go away for a long time. This is facilitated by frequent heartburn after eating, nausea (and in the acute stage - vomiting) and abdominal pain, which can be acute and require a visit to the hospital. Often chronic erosive gastritis can even cause anemia.
NON-STEROID GASTROPATHY
Currently, in the practice of treating patients suffering from various diseases (musculoskeletal system and connective tissue, so-called “rheumatic” diseases, osteochondrosis, osteoarthritis, ankylosing spondylitis, gout, etc.), non-steroidal anti-inflammatory drugs (NSAIDs) are widely used.
One of these drugs is acetylsalicylic acid (ASA), which is used to reduce fever and improve the general condition of patients with many diseases (for preventive purposes, the drug is often prescribed for coronary heart disease). Other positive qualities of ASA are known, which determine its use in the treatment of certain diseases. In particular, it is known that even irregular intake of ASA [9] reduces by 90% the incidence of esophageal cancer associated with exposure to various chemicals. Systematic intake of ASA in dosages usually recommended for the prevention of cardiovascular diseases reduces the risk of developing colon and rectal cancer [5]. However, this positive effect of ASA appears only 10 or more years after starting to take this drug. There are known observations of some researchers [6], indicating that the use of NSAIDs for more than 5 years reduces the risk of developing colorectal adenomas [7], which confirms the hypothesis of a certain protective effect of NSAIDs.
Among the significant reasons for the widespread use of NSAIDs in the treatment of patients, one can name the high prevalence of many diseases (neuritis, neuralgia of various origins, ankylosing spondylitis, arthrosis, rheumatoid arthritis, osteochondrosis, etc.) and the high effectiveness of the use of NSAIDs in the treatment of these ailments (as symptomatic agents, without which successful treatment of patients is often impossible). Many people often take NSAIDs [15] without any medical supervision. Some researchers [4] believe that NSAIDs are used without a prescription 7 times more often than prescribed by a doctor; It is especially popular among patients with ASA. This primarily applies to elderly and senile people (more than 40–45%).
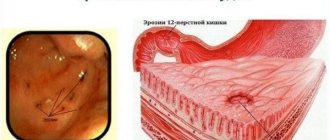
NSAID gastropathy (nonsteroidal gastropathy). A specific syndrome usually associated with the treatment of patients with NSAIDs is NSAID gastropathy, predominantly manifested by damage to the stomach (usually its antrum), somewhat less commonly, the duodenum with the appearance of erythema, erosions and/or ulcers [1], which has become increasingly attractive in recent years attention of researchers.
The main risk factors for the development of NSAID gastropathy are old age, a history of peptic ulcer disease, and male gender. Some importance in the occurrence of NSAID gastropathy is also given to such factors as the duration of patients taking NSAIDs, simultaneous treatment of patients with several NSAIDs, and increasing their dosages. There is a significant “dependence” [5] between the use of NSAIDs and subsequent emergency hospitalization of patients for diseases of the upper gastrointestinal tract. At the same time, women are most often admitted to hospitals; and their share compared to men increases with age.
Pathogenetic aspects of NSAID gastropathy . It is now known that NSAIDs inhibit the enzyme cyclooxygenase (COX), which results in a blockade of prostaglandin synthesis in the gastrointestinal mucosa. This enzyme has two isomers - COX-1 and COX-2. It is believed that COX-1 is an enzyme that regulates the synthesis of prostaglandins involved in cytoprotection, regulation of vascular tone and other processes; this enzyme also promotes the formation of prostacyclin, which provides the cytoprotective properties of the gastric mucosa. COX-2, an enzyme more closely associated with the synthesis of prostaglandins in the inflammatory zone, affects the activation of the inflammatory process. The anti-inflammatory effect of NSAIDs depends on the inhibition of COX-2, the appearance of side effects depends on the inhibition of COX-1.
Currently, more than 35 names of various NSAIDs are known. Some differences in the chemical structure of NSAIDs do not affect their underlying mechanism of action. All NSAIDs are characterized by the ability to inhibit the synthesis of prostaglandins, the main physiological effects of which are: stimulation of the secretion of protective bicarbonates and mucus, activation of cell proliferation in the processes of normal regeneration and increased local blood flow in the mucous membrane. NSAIDs can have a pathological effect (varying in the depth of the lesion) on the condition of the mucous membrane of the stomach and duodenum. In particular, according to some researchers [11], among NSAIDs, according to the results of a systematic review of epidemiological studies: ibuprofen (Brufen) is associated with a lower risk compared to diclofenac (ortofen, voltaren); azapropazone, tolmetin, ketoprofen and piroxicam have a higher risk of gastrointestinal complications, while indomethacin (metindole), naproxen occupy an intermediate position. However, increasing the dosage of one of these drugs (particularly ibuprofen) leads to more frequent complications.
The effect of various NSAIDs on the formation of ulcers and erosions in the stomach and duodenum depends on the degree of their inhibitory effect on one or another isomer. Other factors that contribute to their formation also play a role in the appearance of ulcers and erosions (imbalance between the factors of aggression and defense, including a decrease in the production of mucus and bicarbonates, a decrease in the intensity of blood flow, etc.). The main factors of aggression most often include exposure to hydrochloric acid, pepsin, phospholipids, a number of drugs (including NSAIDs), alcohol, tobacco, etc.; to protective factors - secretion of mucus and bicarbonates by the gastric mucosa, blood supply, etc.
Frequent use of NSAIDs in the treatment of patients with various diseases, often the need for prolonged, including constant or periodic use of these drugs, along with possible pathological effects on various human organs, is among the main factors leading to various side effects [4]. including damage to the liver, kidneys and skin with the appearance of corresponding clinical symptoms.
Erosion of the stomach and duodenum associated with the use of NSAIDs often does not manifest any clinical symptoms, or patients experience only mild, occasional pain in the epigastric region and/or dyspeptic disorders, to which patients often do not attach importance and therefore do not seek treatment. for medical help.
In some cases, patients become so accustomed to their minor abdominal pain and discomfort that when they go to the clinic about their underlying disease, they do not even report them to their doctor (the underlying disease worries patients much more). Obviously, therefore, in patients visiting outpatient clinics for examination and treatment for the underlying disease, it is often not possible to identify clinical symptoms considered characteristic of diseases of the upper gastrointestinal tract. Apparently, this is also explained by the fact that NSAIDs reduce the intensity of the symptoms of gastrointestinal lesions due to their local and general analgesic effect.
An exact correlation has not been established between the presence and severity of focal pathological lesions of the stomach and duodenum (erosions and ulcers) associated with NSAID treatment and the symptoms of these diseases. 45–55% of patients with erosive and ulcerative lesions of the stomach and duodenum do not have any symptoms indicating damage to these organs. A significant proportion of patients taking NSAIDs may experience pain in the epigastric and/or pyloroduodenal region and/or dyspeptic disorders in the absence of any focal pathological changes in the stomach and duodenum.
A survey of patients taking NSAIDs and admitted to the hospital for further treatment showed that in patients complaining of abdominal pain and/or dyspeptic disorders, pain in the epigastric region is observed in 75% of cases; the most common dyspeptic symptoms are heartburn (44.2%), nausea (37.2%) and belching (35.7%), less often - vomiting (5.7%) [2].
The most common and dangerous manifestations of NSAID gastropathy are the formation of stomach and duodenal ulcers (the latter develop 2 times less often); their appearance, along with the progression of the disease, can lead to bleeding, penetration and perforation of ulcers, stenosis of the duodenum and stomach, which are possible in 1–2% of cases [14]. Relatively often, the first clinical symptoms of a patient having erosive and ulcerative lesions of the stomach and duodenum are the appearance of minor or heavy bleeding, weakness, sweating, pale skin, vomiting and melena. This appears to be largely due to the analgesic effect of NSAIDs themselves. Much less frequently, patients with erosive and ulcerative lesions of the stomach and duodenum associated with NSAIDs experience intense pain in the epigastric region and dyspeptic disorders. Most often they develop in patients with deep ulcers.
According to some observations [3], gastrointestinal bleeding develops in more than half of patients taking NSAIDs. According to other researchers [16], the use of NSAIDs in the treatment of patients is directly related to the incidence of bleeding from the upper gastrointestinal tract.
There is also evidence [17] that long-term ASA therapy is associated with a significant increase in the incidence of gastrointestinal bleeding. There is no clear evidence that reducing the dose of ASA or using modified dosage forms can reduce the incidence of gastrointestinal bleeding. Repeated attempts have been made to create NSAIDs that would not have such a pronounced damaging effect on the mucous membrane of the gastrointestinal tract. Thus, great hopes were associated with the creation, in particular, of ASA with an enteric coating and in a buffer form. However, it turned out [12] that taking even small doses of this form of ASA increases the risk of massive gastrointestinal bleeding. The assumption that these forms are less dangerous compared to regular ASA is apparently erroneous.
Taking NSAIDs and older age, as observed by other researchers [18], are risk factors for bleeding from gastric ulcers, in contrast to “isolated” Helicobacter pylori (HP) infection. When using NSAIDs in the elderly, there is an increased risk of bleeding from gastric ulcers associated with HP infection, suggesting a possible interaction between these factors. However, in old age and senility, the likelihood of bleeding and perforation increases. The development of bleeding in such patients may be facilitated by concomitant diseases of the cardiovascular system and liver, and concurrent treatment with corticosteroid drugs and anticoagulants.
According to our observations, the appearance of bleeding in patients treated with NSAIDs is possible at different times from the start of systematic use of non-steroidal anti-inflammatory drugs for the underlying disease, often even with small doses of these drugs, regardless of the state of the acid-forming function of the stomach and the contamination of the mucous membrane with NP stomach. The greatest risk of bleeding is observed in the first month of treatment of patients with NSAIDs, a slightly lower risk later (during the first year). Then the patient’s body somehow “adapts” and the likelihood of bleeding decreases (why this happens is still unclear). Apparently, the mucous membrane of the stomach and duodenum in some patients may acquire some resistance to the damaging effects of NSAIDs.
The greater resistance of the mucous membrane of the stomach and duodenum to the damaging effects of NSAIDs, as the duration of their use by patients increases, is to a certain extent evidenced by the following facts [2].
- Most often, erosive and ulcerative lesions of the stomach and duodenum are observed in the first year from the start of systematic use of NSAIDs by patients (73.3%), less often in later periods (26.7%) - from one year to 10 years.
- There is no tendency to increase the frequency of HP contamination of the gastric mucosa as the duration of patients taking NSAIDs increases. Reducing the frequency and intensity of pain in the epigastric region and dyspeptic disorders.
- Less pronounced increase in lipid peroxidation processes compared to patients with peptic ulcer.
- Less significant inhibition of prostaglandin synthesis (compared to patients with peptic ulcer), which indicates less damage to the mucosal barrier.
Treatment of gastric and duodenal ulcers associated with NSAIDs
Observations show that in recent years, for the treatment of patients with NSAID gastropathy, gastroenterology hospitals have been receiving mainly patients with stomach ulcers and, less often, with duodenal ulcers associated with NSAIDs.
Before prescribing NSAIDs (especially primary) for the underlying disease, it is necessary to find out the presence or absence of a history of peptic ulcer. This disease is a relative contraindication to the use of NSAIDs. In doubtful cases, endoscopic examination of the esophagus, stomach and duodenum (EGD) is indicated (Pentax, EXERA, Olimpus). Identification of an ulcer or cicatricial ulcerative deformity of the stomach and duodenum (taking into account the medical history) based on the results of endoscopy and/or x-ray examination (before treatment of patients with NSAIDs) indicates the presence of a peptic ulcer in the patient.
It is advisable to prescribe NSAIDs after meals, if possible excluding their combined use with other drugs that have a pathological effect on the mucous membrane of the digestive tract. Indications for endoscopic examination of the upper gastrointestinal tract, including the esophagus:
- the appearance of abdominal pain and dyspeptic disorders during treatment of patients with NSAIDs;
- absence of complaints in patients, especially elderly and senile patients, who have been systematically taking NSAIDs for a long time.
If focal lesions of the esophagus, stomach and duodenum, including reflux esophagitis, are detected, a control endoscopic examination of the esophagus, stomach and duodenum (Pentax, EXERA, Olimpus) is performed before treatment. It is advisable to carry out control endoscopic examinations in patients who have begun to be systematically treated with NSAIDs in the following periods: one month from the start of taking NSAIDs, and then once a year. Detection of erosions and ulcers of the stomach and duodenum during endoscopic examination during treatment of patients with NSAIDs requires clarification of the tactics of treating patients (taking into account the presence and underlying disease).
Experience shows that in the treatment of patients with NSAID gastropathy, positive results in the treatment of the underlying disease, as well as the frequency of possible side effects and complications, largely depend on the dosage of these drugs, the timing of their use and individual tolerance by patients. The use of NSAIDs in lower dosages in the treatment of patients reduces the likelihood of side effects and complications.
Typically, when treating patients with erosive and ulcerative lesions of the stomach and duodenum associated with NSAIDs, when patients are forced to continue taking NSAIDs, they are based on two principles:
- canceling the prescribed drug or replacing it with another NSAID that is less “ulcerogenic”;
- prescribing medications, the use of which helps eliminate pain and dyspeptic disorders, and if erosions and ulcers are detected, then their healing.
For patients with gastric or duodenal ulcers or those with a history of peptic ulcers, as well as elderly and senile patients, NSAIDs are indicated only in cases where other treatment options are ineffective. If erosions and ulcers of the stomach and duodenum occur in patients receiving NSAIDs, if possible, it is advisable to discontinue these drugs and prescribe “anti-ulcer” treatment. In cases where NSAIDs cannot be discontinued, it is advisable, if the condition of the patients allows, to reduce the dosage of these drugs or transfer patients to less “ulcerogenic” drugs. Recently, it has often been proposed to use paracetamol (daleron, calpol, sanidol, efferalgan) for this purpose.
To eliminate clinical manifestations considered characteristic of lesions of the stomach and duodenum, and to heal erosions, as well as to prevent their occurrence, various drugs are currently offered: most often - misoprostol (Cytotec), H2-histamine receptor antagonists (ranitidine, famotidine) and inhibitors proton pump (omeprazole, rabeprazole, esomeprazole), antacid drugs (almagel neo, phosphalugel, talcid, maalox, rennie, magalfil, etc.).
The advisability of using misoprostol, H2-histamine receptor antagonists and proton pump inhibitors in the treatment of erosive and ulcerative lesions of the stomach and duodenum is evidenced by the following facts. Misoprostol suppresses the secretion of acid and pepsin by the stomach, increases the amount of mucus and the density of the mucous gel, increases the secretion of bicarbonates and improves blood supply in the gastric mucosa, promotes the restoration of cells of the gastric mucosa and reduces the reverse diffusion of hydrogen ions, which is one of the cytoprotective properties of misoprostol. Proton pump inhibitors and histamine H2 receptor antagonists inhibit gastric acid formation and have some cytoprotective effects.
It is not recommended to take misoprostol, as well as other medications, simultaneously with antacids (the latter significantly reduce the concentration of misoprostol in plasma).
Typically, these drugs are prescribed as monotherapy and in usual therapeutic dosages: misoprostol 200 mcg 4 times a day, ranitidine (acidex, acylok, gistac, zantac, zoran, ranitin) 150 mg 2 times a day or famotidine (gastrosidine, quamatel, ulfamide, ulceran, famonite, famocid) 20 mg 2 times a day (or 300 mg or 40 mg, respectively, once a day), omeprazole (Losec, Omizak, etc.), rabeprazole (Pariet) or esomeprazole (Nexium) also respectively, 20 mg 2 times a day. During the period of healing of stomach and duodenal ulcers, the effectiveness of proton pump inhibitors in these dosages is slightly higher.
The advantage of H2-histamine receptor antagonists and proton pump inhibitors over misoprostol (Cytotec), according to our observations, is the faster elimination of pain in the epigastric and/or pyloroduodenal region and heartburn, as well as better tolerability of these drugs by patients. When taking misoprostol, some patients note a short-term burning sensation behind the sternum (along the esophagus) and in the epigastric region.
As our observations have shown, in the treatment of patients with gastric and duodenal ulcers associated with NSAIDs, generics of omeprazole (Losec, Omizak, Gastrozol, Omez, Omitox, Ultop) also have a positive effect.
Information given in the literature about the effectiveness of a particular drug in the treatment of patients with erosions and ulcers of the stomach and duodenum associated with NSAIDs is usually based on the results of treating patients with the above “standard” dosages of these drugs. Increasing the dosage of famotidine to 40 mg 2 times a day, as our observations have shown, can increase the effectiveness of treatment for such patients. In most patients, this dosage of famotidine not only promotes healing, but also helps prevent the occurrence of ulcers and erosions associated with NSAIDs.
The presence of intense pain in the epigastric region, dyspeptic disorders and/or large ulcers of the stomach and duodenum, according to our observations, serves as an indication for complex drug treatment of patients - the combined use of misoprostol with H2-histamine receptor antagonists, antacids or proton pump inhibitors ( in therapeutic dosages). Our observations [1] allowed us to establish that misoprostol (Cytotec) 400 mcg 4 times a day in combination with ranitidine 300 mg or famotidine (quamatel) 40 mg once a day is more effective in the treatment of gastric and duodenal ulcers associated with NSAIDs, compared with misoprostol at the same dosage in combination with ranitidine, prescribed 150 mg 1 time per day. In the absence of severe pain in the epigastric region (and with small ulcers of the stomach and duodenum), you can limit yourself to the use of H2-histamine receptor antagonists, proton pump inhibitors, misoprostol in therapeutic dosages, and antacids.
Antacid drugs (Almagel neo, phosphalugel, talcid, Maalox, Rennie, Magalfil, etc.) have been used for a long time in the treatment of patients suffering from various gastroenterological diseases. Some of the antacid drugs (in particular, those containing aluminum hydroxide, for example Almagel Neo) also have a cytoprotective effect, which consists in enhancing the secretion of mucus and the synthesis of prostaglandins.
The undoubted advantage of antacid drugs is the rapid elimination (reduction of intensity) of heartburn (burning) behind the sternum and/or in the epigastric region and other gastrointestinal symptoms caused by the disease itself, for which treatment is being carried out, taking medications and intoxication. Most often, antacid drugs are prescribed in the following cases: with so-called “on-demand” therapy to quickly eliminate (reduce the intensity) symptoms of dyspepsia, especially heartburn and pain (at any time of the day); during a course of treatment 30 - 40 minutes before or 30 - 60 minutes after a meal (if necessary and before bedtime) as monotherapy or in complex treatment, in combination primarily with prokinetics and/or with H2-blockers of histamine receptors (frequency and the duration of taking antacid medications are determined by the general condition of the patient).
It is known that antacid drugs have an adsorbing ability, due to which it is possible to reduce the activity and bioavailability of some medications taken by the patient (for example, H2-blockers of histamine receptors, non-steroidal anti-inflammatory drugs, antibiotics, etc.). Therefore, when prescribing antacid drugs in combination with other drugs, it is advisable to recommend that patients observe the time interval between taking antacid drugs and taking other drugs (about 2–2.5 hours), i.e., indicate the time when patients take specific drugs during the day.
NSAIDs and Helicobacter pylori. The question of the feasibility/inexpediency of carrying out eradication therapy for HP is periodically discussed. There are conflicting opinions about the advisability of anti-Helicobacter therapy in the treatment of patients with gastric and duodenal ulcers associated with NSAIDs. It is possible that the presence of neutrophils in the gastric mucosa [19] increases the incidence of ulcers in patients taking NSAIDs for a long time (there is a correlation between neutrophils and HP). Taking into account this fact, it can be assumed that in some patients, eradication of HP can prevent the occurrence of ulcers caused by taking NSAIDs.
The appearance of dyspepsia symptoms during treatment with NSAIDs, which are considered characteristic of lesions of the upper gastrointestinal tract, is sometimes associated with conditions and lifestyle, with the presence of HP in the patient, believing that in such patients taking non-steroidal anti-inflammatory drugs is associated with a high risk of various complications . According to other information, eradication of HP does not provide advantages in the treatment of patients taking NSAIDs for a long time; on the contrary, it prolongs the healing period of ulcers. In particular, according to some data [10], eradication of HP in patients who have (or previously had) peptic ulcers and/or dyspeptic disorders and continue to take NSAIDs for a long time complicates the healing of gastric ulcers and does not affect the incidence of peptic ulcers or dyspeptic disorders. disorders arising by the end of 6 months. Apparently, this is due to the fact that HP and NSAIDs are independent risk factors for the occurrence of gastric and duodenal ulcers.
This difference of opinion may be due to the fact that researchers do not differentiate between patients taking NSAIDs. In our opinion, ulcers in patients taking NSAIDs can be divided into two categories:
- ulcers of the stomach and duodenum, the appearance of which is directly related to the use of NSAIDs (in patients who do not have a history of peptic ulcer);
- ulcers of the stomach and duodenum, present in patients who had a history (before starting NSAIDs) of a peptic ulcer (in such cases it remains unclear whether we are talking about an exacerbation of a peptic ulcer or the appearance of an ulcer is associated with exposure to NSAIDs on the patient’s body - the latter option remains subject of debate).
The occurrence of erosions and ulcers in itself is only a stereotypical response of the body to various influences; Essentially, the ability of the human body, in the process of evolution, to develop a minimum of responses to various influences helped it survive (as well as the entire animal and plant world).
Our observations of patients taking (taking) NSAIDs who had stomach or duodenal ulcers showed the following. Carrying out 7–10 days of eradication therapy (followed by treatment with the basic drug for 2.5–3 weeks) in the treatment of patients with gastric or duodenal ulcers is justified in cases where patients have a history of peptic ulcer disease, and the latest examination using at least 2-3 methods showed, in addition, the contamination of the gastric mucosa with HP.
Currently, it is often hypothesized that eradication of HP reduces the incidence of gastric and duodenal ulcers associated with NSAIDs, if it was carried out before the start of treatment of patients with NSAIDs.
Prevention of gastric and duodenal lesions associated with NSAIDs
The issues of reliable prevention of lesions of the stomach and duodenum that arise during the treatment of patients with NSAIDs remain the subject of debate. There is a generally accepted point of view on which drugs prescribed simultaneously with NSAIDs (H2-histamine receptor antagonists, proton pump inhibitors or misoprostol), taking into account their effectiveness and cost-effectiveness, duration of treatment courses, NSAID dosages, specific diseases, are advisable to use in patients with Unfortunately, no. Therefore, attempts are being made to develop the most optimal options for preventive treatment of patients. It has been established [13] that misoprostol in the majority of patients more effectively prevents the development of gastric ulcers caused by taking NSAIDs; Misoprostol and H2-histamine receptor antagonists are successfully used to prevent duodenal ulcers in most patients.
Proton pump inhibitors, according to our observations, are somewhat more effective in preventing the appearance of gastric and duodenal ulcers associated with NSAIDs. One of the significant advantages of H2-histamine receptor antagonists not only over misoprostol, but also over proton pump inhibitors is their lower cost.
Unfortunately, after 6 months [8], relapses of ulcers occur in 3.5% of cases. Therefore, after healing of gastric and duodenal ulcers associated with NSAIDs, it is advisable (if possible) to prescribe less “ulcerogenic” NSAIDs to patients who are forced to take NSAIDs for the underlying disease; It should also be additionally recommended to carry out preventive courses of treatment with histamine H2 receptor antagonists, misoprostol or proton pump inhibitors (omeprazole, rabeprazole and esomeprazole) in patients with gastric and duodenal ulcers, regardless of the presence or absence of a history of these diseases. It is not advisable to reduce the therapeutic dosage of these medications. Thus, reducing the dosage of omeprazole even to 20 mg/day (when carrying out preventive treatment of patients) reduces the effectiveness of the drug.
It is equally important when choosing one or another treatment option for patients in inpatient or outpatient settings, as well as when carrying out preventive measures, to take into account the availability of drugs chosen by the doctor in the pharmacy network, the financial capabilities of the hospital or a particular patient.
The timing of repeated preventive courses of treatment for patients taking NSAIDs is determined by the general condition of the patients, the presence or absence of symptoms that are considered characteristic of diseases of the gastrointestinal tract, and the results of dynamic endoscopic studies of the stomach and duodenum.
For questions regarding literature, please contact the editor.
Yu. V. Vasiliev, Doctor of Medical Sciences, Professor TsNIIG, Moscow
Complex treatment
If erosive gastritis is diagnosed, it is necessary to harmoniously combine treatment and diet, folk remedies and medications. Therefore, even the best drugs will not help with this disease if a person does not change his diet. The same applies to folk remedies, which in this case will also not work. Food should not be hot, portions should be small, and meals should be frequent. You cannot eat anything fatty, spicy, salty or pickled, fried or smoked, chocolate or cookies. You should also give up alcohol, carbonated drinks, coffee and black tea, and definitely stop smoking.
It is interesting that doctors themselves often recommend symptomatic alternative treatment and prescribe therapeutic therapy. This is because these recipes contain foods and herbs with anti-inflammatory and regenerative properties that can return stomach acidity to normal. If gastroduodenitis (that is, inflammation of the pylorus of the stomach and duodenum) is still in a superficial form, therapy with folk remedies can even completely cure, in other cases it will simply significantly alleviate the patient’s condition, which is also very important.
Prevention and prognosis
To avoid the development of the disease, you need to carefully plan your menu, adhere to the correct diet, and do not eat too hot or cold food. When taking NSAIDs and glucocorticosteroids, you must strictly adhere to the dosage and follow your doctor's recommendations. When the first symptoms of the disease appear, you should contact a gastroenterologist and undergo testing for the presence of Helicobacter pylori.
The prognosis of erosive gastroduodenitis is favorable with timely treatment. Otherwise, there is a high risk of the patient developing gastric and duodenal ulcers.
Author of the article:
Gorshenina Elena Ivanovna |
Gastroenterologist Education: Diploma in General Medicine received from the Russian State Medical University named after. N. I. Pirogova (2005). Postgraduate course in the specialty "Gastroenterology" - educational and scientific medical ]Our authors[/anchor]
Decoctions and infusions
Erosive or antral gastritis is well treated with oats. To prepare a medicinal decoction, take “Extra” oatmeal, add one large spoon to a liter of water and simmer for half an hour. After this time, the broth should be allowed to cool, then strain and drink in a mug in the morning on an empty stomach.
You can also drink it as a second breakfast and late dinner, or take it 10 minutes before your main meal. The course of such treatment: at least a week.
Flax, or rather an infusion of its seeds, can also help with gastritis. Lingerie relieves inflammation and allows you to quickly restore the gastric mucosa, so this recipe should definitely be in the arsenal of every person with gastrointestinal problems. To make a flax infusion, pour a large tablespoon of flax seeds into a cup of warm water and set aside in a warm place overnight. Drink 30 minutes before breakfast and repeat this action until the end of the procedure. By the way, in the morning you can drink a tablespoon of flaxseed oil.
Erosive gastroenteritis is also treated with herbal infusions. Here are their options:
- When acidity is low. 4 parts dried wormwood herb and 1 part dried yarrow herb. One large tablespoon of the prepared harvest should be poured with a glass of boiling water and boiled for 3 minutes. After an hour, strain and take 80 ml an hour before meals for about a month and a half.
- When acidity is high. Dried herbs of chamomile, St. John's wort, peppermint and yarrow in equal parts. The preparation method is the same, but the resulting broth should be mixed with a small teaspoon of honey and 100 ml should be drunk. The time and duration of use are also the same - before meals and for at least a month.
You can also collect fresh birch leaves in the spring and pour a handful into a glass of water, preferably filtered. Then everything should be boiled, boiled for several minutes and cooled, then strain the broth and drink half a glass an hour after eating.
Diagnostics and necessary examinations
A gastroenterologist makes a diagnosis based on medical history, examination, clinical test data, and endoscopic examination.
An external examination reveals signs of anemia - pale skin, disruption of the structure of hair and nails. When palpating the stomach area, painful sensations are possible. A blood test reveals signs of iron deficiency anemia, and a stool test reveals occult blood.
The doctor receives detailed information when performing EGDS (esophagogastroduodenoscopy). The diagnostic procedure helps to establish the degree of damage to the mucous membrane, the localization of erosions and areas of hemorrhage. To exclude the oncological nature of mucosal defects, a targeted biopsy is performed in parallel.
The gastroenterologist may prescribe additional tests: PCR diagnostics or urease breath test to detect Helicobacter pylori, pH-metry to determine the level of acidity of gastric juice.
Propolis tincture
If stomach erosion begins to show severe pain, propolis tincture is a good home remedy. It can usually be purchased at a pharmacy in the form of an alcohol solution, which must be diluted with water before use.
To treat gastritis, you need to mix 20 drops of the tincture with a mug of clean boiled water and drink the resulting medicine every five hours. The pain decreases almost immediately, but the effect persists after 3 weeks of continuous use of propolis tincture.
Vegetable juices
Only freshly squeezed juices from neutral (acidity) vegetables are intended. They cannot harm the stomach in any way, but will only bring benefits:
- Cabbage juice. It should be prepared by peeling the juiciest cabbage leaves and squeezing 70-80 ml of juice from them, which should be drunk orally 2-3 times a day.
- Potato juice. Only the freshest tubers without roots and green parts are suitable for this juice. One large teaspoon is enough an hour before meals every morning.
- Pumpkin juice. This juice not only solves stomach problems, but also supports intestinal function. This juice can be consumed as a regular drink.
- Celery and carrot juice. Take 0.4 kg of carrots and 100 g of celery stalks per serving and drink half a glass before lunch and dinner.
Clinical examination
- Collection of information about the patient.
- Analysis of complaints and patient's condition.
- Inspection and palpation.
Based on the data obtained, a further diagnostic plan is drawn up. Then laboratory tests are carried out:
- Blood test: general, biochemistry.
- Urine examination.
- Assessment of the characteristics of feces: comprogram for occult blood.
Return to contents
Gastroscopy with biopsy
A probe with a camera, lighting equipment and a biopsy probe at the end is inserted into the stomach through the mouth. The internal condition of the walls is examined, the nature and extent of damage, and the location of hemorrhages are assessed. A sample is taken from the most damaged area of the mucosa and sent for histological analysis. As the mucous membrane is examined, swollen areas with redness and erosive single or multiple lesions from which blood oozes can be detected.
Return to contents
Ultrasound
Ultrasound scans all the organs of the abdominal cavity. The liver, pancreas, and gallbladder are especially carefully examined, disturbances in which can provoke hemorrhagic inflammation of the mucous membrane. The method allows you to detect a tumor in time.
Return to contents
- Erosive-hemorrhagic gastritis - symptoms, treatment and diet
Electrogastroenterography
A study of the motor-evacuation function of the digestive organ is being conducted. The process of moving food through the gastrointestinal tract with its mixing and processing by gastric juice is analyzed. The quality of the stomach is assessed.
Return to contents
X-ray
The method is used as a differential diagnosis of gastritis with separation from ulcers and cancer. The degree of development of gastritis cannot be determined using this method. If ulcers and tumors are not detected, other methods for diagnosing gastritis are used.
Return to contents
Treatment with aloe and honey
Honey is traditionally considered a product that helps with a variety of ailments and has a beneficial effect on the entire body. For erosive gastroenteritis, the combination of honey and aloe vera is very effective - it accelerates the healing of the irritated mucous membrane and all the unpleasant symptoms of the disease disappear.
To prepare the remedy, first prepare the aloe vera leaves by placing them in the freezer for 24 hours. Leaves from a plant that is already 4 years old are suitable; younger leaves have less beneficial properties.
Crush the prepared aloe, squeeze out the juice (a few leaves are enough) and mix with 300 grams of honey. The finished medicine should be stored in the refrigerator and consumed with a large spoon every morning before meals. The duration of this therapy is approximately 21 days.
Another recipe from aloe and honey: 200 gr. juice (by the way, you can buy at the pharmacy) and the same amount of honey, as well as 0.5 liters of natural red wine. The thoroughly mixed mixture should be kept in a dark place for 2 weeks, and then taken three times a day before meals. Gastritis treatment should not be used continuously.
Diagnostics
The best method for diagnosing erosive gastroduodenitis is esophagogastroduodenoscopy, or EGDS. The study is carried out using an endoscope equipped with a microscopic camera. The purpose of endoscopy is to determine changes in the mucous membrane associated with the inflammatory process, as well as to assess the size and location of erosions.
What the doctor sees during the examination:
- Hyperemia and swelling of the mucous membrane of the stomach and duodenum;
- Looseness of the mucous membrane and increased sensitivity to touch;
- Bleeding in the area of erosion;
- Minor hemorrhages;
- Gray coating on erosions in the form of a film;
- The size of the defects is 0.3-0.5 mm.
During endoscopy, the doctor performs a biopsy of an area of the mucosa for histological examination and clarification of structural changes.
Diagnosis of the presence of Helicobacter pylori:
- Microscopic examination of biopsy material from the stomach and upper intestine;
- PCR test - search for bacterial DNA by the presence of DNA polymerase;
- Breathing test – collection of air exhaled by the patient before and after exercise;
- The ELISA method is a test of blood serum for the presence of antigens to a bacterial agent.
Anemia is diagnosed using a complete blood test. When hemorrhagic anemia is confirmed, the color indicator sharply decreases, the level of hemoglobin and red blood cells drops.
Other recipes for the treatment of erosive gastritis
Traditional medicine offers many other recipes for the treatment of erosive gastritis, each of which has a rational grain. Therefore, it is worth taking a closer look at them:
- Wheat germination. Two-thirds of a glass of wheat grain should be poured with water and left in this form for 24 hours. When the beans sprout, drain the water and grind them together with the sprouts in a blender or meat grinder. Add a tablespoon of oil and eat.
- Onions fried in milk. Bake a peeled medium-sized onion in the oven until golden brown (it should be soft). After cooking the onion, transfer it to a blender or meat grinder and pour milk into a bowl so that you can drink the mixture. It is recommended to eat this milk on an empty stomach, in small sips every day.
- Raw quail eggs. This product reduces acidity in the stomach and improves digestion. Every morning on an empty stomach you can drink 2 quail eggs or mix them with porridge or vegetable puree if this process is difficult.
When treating erosive gastritis at home, you should remember that this is not a quick treatment and the effects will appear only after long-term complex therapy (that is, drug therapy, etc.). However, the prognosis for this disease is still favorable, if not ignored.
Causes of erosive gastroduodenitis
The pathological process is based on the aggressive influence of hydrochloric acid against the background of its excessive secretion. The epithelial layer of the mucous membrane does not have the ability to regenerate, as a result of which erosions and ulcers appear on it.
Negative factors provoking the development of erosive gastroduodenitis:
- Hereditary predisposition;
- Infection with the bacterium Helicobacter pylori;
- Poor nutrition;
- Frequent stress and psycho-emotional shocks;
- Intestinal infections;
- Poisoning from poor quality products;
- Diseases of neighboring organs of the gastrointestinal tract (liver, pancreas);
- Reflux (backflow) of acid from the duodenum into the stomach;
- Side effects of drugs from the group of NSAIDs, antibiotics, glucocorticosteroids;
- Eating spicy, rough, too hot or too cold food;
- Alcoholism.
Infection with the bacterium Helicobacter pylori is the most common cause of the development and progression of the disease.