02/16/2022
68 676
18 minutes
Author, editor and medical expert – Klimovich Elina Valerievna.
Editor and medical expert – Harutyunyan Mariam Harutyunovna.
The term “tonsillitis” or “acute tonsillitis” refers to an infectious inflammatory disease that occurs with damage to one or more tonsils of the pharyngeal lymphoid ring.
The pharyngeal lymphoid ring surrounds the entrance to the respiratory tract and digestive tract and performs a protective function. It participates in the formation of immunity, neutralizes viruses, bacteria and other microorganisms that enter the body from the external environment through the mouth and nasal openings.
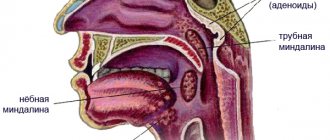
The pharyngeal ring includes six large accumulations of lymphoid tissue - tonsils:
- 2 palatine (tongs), located on both sides of the entrance to the pharynx;
- 1 lingual, located at the root of the tongue,
- 1 pharyngeal - in the upper part of the nasopharynx on its back wall,
- 2 tubes - directly at the entrances of the auditory tubes.
Sore throat is usually called inflammation of the tonsils, although the term is also applicable to other localizations of the inflammatory process1.
Up to contents
Causes of sore throat in children
The disease is more common in school-age children and teenagers2. Sore throat in a child under 2 years of age is rare and is caused by insufficient development of the lymphoid tissue of the pharynx2.
In the vast majority of cases, tonsillitis develops as an infectious process2.
- Primary (banal) it can be caused by:
- beta-hemalytic streptococcus A;
- streptococci C G;
- staphylococci, pneumococci and other bacteria;
- viruses: respiratory parainfluenza viruses, adenoviruses, coronaviruses, respiratory syncytial viruses, roto- and enteroviruses, Coxsackie viruses, herpeviruses, etc.2
- Secondary inflammation can develop:
- for childhood infections (measles, rubella, scarlet fever);
- for syphilis, tuberculosis;
- as one of the symptoms of leukemia or agranulocytosis2.
The high susceptibility of children to viruses and streptococcus causes the widespread prevalence of tonsillitis. The source of infection is always a person – a patient or a carrier of the pathogen.
In the case of viral processes, these are patients with ARVI, measles, rubella, etc., in the case of catarrhal or purulent tonsillitis caused by streptococci, these are patients with tonsillitis.
The route of transmission of pathogens is airborne droplets or contact. Microbes are transferred from the patient into the environment along with sputum when sneezing and coughing. They are introduced into the body of a healthy baby with dirty hands, when using shared dishes, household items and hygiene items, during close contact, for example, when kissing.
The development of tonsillitis is promoted1,2:
- hypothermia, which often happens in the autumn-winter period and early spring;
- overwork, in particular excessive loads associated with training, attending numerous clubs and studios;
- unbalanced diet - predominance of carbohydrate foods in the diet, lack of vegetables and fruits rich in vitamins and essential microelements,
- the presence in the body of a focus of chronic infection (runny nose, sinusitis, caries, otitis media and others);
- decreased immunity after acute respiratory viral infections and other diseases suffered the day before;
- primary immunodeficiency.
Up to contents
Forms of the disease in children
All types of acute tonsillitis occur in children, but their prevalence depends on age.
Sore throat in a child 1-3 years of age is more likely (44% of cases) associated with a herpetic infection2. Only 35% of cases of the disease are the result of the activity of streptococci2.
In children aged 3 to 7 years, tonsillitis is more often bacterial, but streptococci are found only in 28% of cases2. Further, the picture changes towards the predominance of streptococcal infection and in adolescents it already accounts for up to 52% of cases of inflammation.
According to the picture of pathological changes in the tonsils1, inflammation of the tonsils can be:
- Erythematous (catarrhal), accompanied by redness of the tonsils and palatine arches. Viral tonsillitis, streptococcal (in the initial stages of development) or atypical, caused by Yersinia, mycoplasma, chlamydia, have such a clinical picture.
- Vesicular, characterized by the appearance of vesicles with turbid liquid on the tonsils, after opening of which small erosions form on the mucous membrane. This is how herpetic sore throats, tonsillitis with measles, and chickenpox occur.
- Membranous, in which purulent or necrotic films appear on the tonsils1. In lacunar forms, the film forms pus flowing from the lacunae, which is easily removed with a swab2. True films in diphtheria are firmly connected to the underlying tissue of the tonsils2.
According to the severity of the course, acute tonsillitis in children can be:
- light,
- moderate severity,
- heavy.
With the flow:
- without complications,
- with complications.
Up to contents
Why does the temperature rise
Fever accompanies most infectious diseases, including acute tonsillitis2,3. The processes that cause an increase in body temperature are quite well studied. They are triggered by special substances pyrogens, which can enter the body from the outside (exogenous pyrogens) or be synthesized inside it (endogenous pyrogens).
Endogenous pyrogens are substances that enter the bloodstream during the destruction of immune cells and cells of the inflamed mucous membrane of the throat2,3.
Exogenous pyrogens in the case of tonsillitis can be various microorganisms: viruses, bacteria, fungi3. In children aged 3 months to 3 years, tonsillitis most often develops with mixed herpesvirus infections3. When a child reaches the age of 3-7 years, viruses give way to bacteria, and in 30% of cases the disease is caused by group A3 beta-hemolytic streptococcus. In addition, the tonsils are often affected by streptococci of other groups, staphylococci, etc.1 In adults, acute tonsillitis is often viral and accompanies ARVI1.
Exogenous and endogenous pyrogens affect the thermoregulation center located in the brain2,3. As a result, he begins to perceive normal body temperature as lower and increases the level of heat production, which leads to an increase in body temperature2,3.
Up to contents
Symptoms of the disease
Despite the variety of forms, the signs of tonsillitis in children are largely similar. Let us analyze the clinical picture of the disease using the example of the most dangerous streptococcal inflammation1,2.
The incubation period ranges from several hours to 4-5 days - on average 2-4 days3. The onset of the disease is acute - symptoms of infection appear and develop quickly. The introduction of microbes into the tissue of the tonsils leads to their inflammation and the formation of a large amount of toxins. Their absorption causes poisoning of the body and the appearance of general symptoms of intoxication.
General symptoms:
- From the nervous system, weakness, drowsiness, lethargy, tearfulness and headaches are noted. A child of 2-3 years old during a sore throat usually becomes lethargic, begins to be capricious, cry for no reason, goes to bed in the daytime, although he usually refuses to sleep during the day. Older children complain of fatigue.
- Fever occurs as a result of irritation of the thermoregulation center by streptococcal toxins2,4. Sore throat in children is usually characterized by a rapid rise in temperature to 390 C and above, accompanied by chills, pale skin and lips, and cold extremities4.
- Febrile seizures in children (usually under 3 years of age) can occur against the background of a rapid rise in temperature4. They are expressed in twitching of individual muscle fibers or muscles, or in the form of a general seizure, in which the baby’s entire body tenses and bends in an arc.
- Nausea and vomiting, abdominal pain indicate a severe course of the disease1.
- Body aches, muscle and joint pain : Young children may complain of pain in their arms and legs1.
Local symptoms
These are the visible changes occurring in the throat and the sensations they cause. Depending on their nature, catarrhal, follicular, lacunar tonsillitis, as well as necrotic (ulcerative-necrotic, membranous-necrotic) acute tonsillitis are distinguished.
Catarrhal inflammation develops in all cases as the initial stage of the pathological process 1.3. If the immune system is strong and antibacterial treatment of a child’s sore throat is started on time, the disease can stop at this stage and then begin its reverse development3.
The tonsils, arches, soft palate and uvula look red and swollen. There are no raids on them. The baby develops a foreign body sensation, sore throat and sore throat when swallowing, and drooling.
Follicular tonsillitis is characterized by purulent melting of the follicles of the tonsils. Through the inflamed bright red mucous membrane of the tonsils, whitish-yellowish islands, the size of a grain of rice (3-4 mm), are visible. In this case, there is no pus on the surface of the tonsils - it is located inside under the mucous membrane.
In the case of lacunar tonsillitis, yellowish-white pus is secreted from the lacunae onto the surface of the tonsils and covers them with a thin layer, forming easily removable films. The smell from the mouth becomes sweetish-sweet, putrid, the pain in the throat becomes constant, independent of food intake. The baby's appetite decreases and he refuses to eat.
With necrotic sore throat in children, the throat looks uniformly red, large, 1-2 cm in size, areas appear on the tonsils, covered with a “pearly” dirty gray coating. The plaque is tightly bound to the underlying tissues. After its rejection, deep bleeding ulcers form on the surface of the tonsils. The development of necrotic processes indicates a severe course of the disease.
In all cases, streptococcal inflammation spreads to nearby (regional) lymph nodes. They are felt on the neck, below the corners of the lower jaw in the form of painful round formations, the size of which depends on the severity of the disease.
Severity
The disease can occur in mild, moderate and severe forms.
| 1. Light | A sore throat in a child over 5 years old can occur without pronounced symptoms of intoxication with mild weakness, low-grade fever (below 380 C) for 1-5 days, mainly with catarrhal changes in the tonsils, some pain and enlarged lymph nodes up to 1 cm3. This type of flow is considered mild . In children in the first years of life, the disease is often more severe. |
| 2. Medium-heavy | The moderate severity of the disease is indicated by the moderate severity of the general symptoms of angina: temperature above 38.50 C, weakness, headaches and body aches last for 6-8 days3. The tonsils are covered with purulent films and clear no earlier than after 4-6 days3. The lymph nodes are enlarged to 2 cm, but, despite the severity of the condition, there are no complications3. |
| 3. Heavy | A severe course is characterized by the appearance of severe symptoms of intoxication, including vomiting, abdominal pain, and diarrhea. A temperature above 39.50 lasts up to 9 days, exhausts the little man, and is often accompanied by febrile convulsions. In the pharynx there is a picture of filmy or ulcerative necrotic tonsillitis. Lymph nodes reach 3 cm in size. The tonsils are cleared after a week or even later. |
Up to contents
Fever as an indicator of the severity of sore throat
The level of fever in sore throat is related to the nature of the infection, the severity of inflammation and the general condition of the body1.
- With a mild course of acute tonsillitis, the temperature is subfebrile (up to 38.50C) and does not last longer than 2-3 days. The sore throat is insignificant, the general condition suffers little - slight weakness and drowsiness may be noted. Sore throat is more often catarrhal, that is, it is limited to redness and swelling of the tonsils.
- Symptoms of follicular tonsillitis and a temperature of 38.5-390C in an adult indicate a moderate course of the disease . Fever lasts 4-6 days, accompanied by severe weakness, chills, headache, aches in muscles and joints, indicating significant intoxication. Severe pain in the throat when swallowing. The tonsils are red, enlarged in size with a scattering of pus-filled follicles or purulent deposits. The cervical lymph nodes enlarge up to 2 cm and become painful when touched.
- In severe tonsillitis, the fever reaches 390C or higher. Intoxication is severe, sometimes it leads to functional disruptions in the functioning of the heart and kidneys. The sore throat becomes constant, squeezing the throat. Lymph nodes reach a size of 3 cm. Complications often develop, such as peritonsillar abscess and otitis media.
Fever can be one of the first symptoms of a sore throat. Thus, with streptococcal tonsillitis, fever up to 390C, chills, headache first appear, and only then, after 2 days, sore throat and other symptoms typical of inflammation of the tonsils1.
The level of temperature rise depends on age. Thus, due to physiological characteristics in young children and the elderly, the febrile reaction may be less pronounced than in young people1,3. High numbers on the thermometer should not be expected either in patients with weakened immune systems3.
Up to contents
Diagnostics
Inflammation of the palatine tonsils is sometimes accompanied by severe swelling, which can spread to the underlying parts of the respiratory tract and lead to severe difficulty breathing. Against the background of intoxication, cardiovascular failure and shock may develop3. Therefore, it is impossible to treat sore throat in children at home without consulting a doctor.
The clinical picture of angina is obvious. Whether or not there is inflammation can be seen when examining the throat. The main question that the doctor has to answer before starting treatment is what infection caused the inflammation.
- Viral tonsillitis caused by respiratory viruses is usually catarrhal1 and is accompanied by other symptoms of ARVI: discharge from the nasal passages, sneezing, nasal congestion, cough, conjunctivitis and others2. In the herpetic form, small blistering rashes are visible on the mucous membrane of the palate, uvula and tonsils.
A viral infection does not require antibacterial therapy; it can be treated with symptomatic means1,2.
- Diphtheria is the main danger2. Its main feature is the discrepancy between the severity of intoxication and sore throat and the changes occurring in the tonsils2. By the end of the first day of the disease, against the background of malaise, low-grade fever and mild sore throat, the tonsils become covered with a white-gray “pearly” film. In this case, the surrounding mucosa looks more bluish than red, and the lymph nodes practically do not enlarge.
As the pathological process develops, the temperature increases to 400 C, the baby begins to become delirious, and plaque covers not only the tonsils, but also the palate and uvula2. Swelling can spread to the airways and neck, making breathing very difficult.
Treating such a sore throat in a child at home is strictly prohibited!
- Candidal tonsillitis is one of the manifestations of a common fungal infection that accompanies HIV and other severe immunodeficiency conditions2. Since they are rare in childhood, candidal tonsillitis in a child 4-7 years old is more of a casuistry than a reality.
With candidiasis, the plaque is curdled; it covers not only the tonsils, but also other areas of the mucous membrane of the oral cavity and pharynx. There is no fever, the lymph nodes are not enlarged. Treatment primarily includes antifungal drugs2.
To accurately determine the causes of the disease, laboratory diagnostics are performed. It includes:
- microbiological analysis of a smear from the surface of the tonsils and the back wall of the pharynx to identify the causative agent of infection and determine its sensitivity to antibiotics1 (result after 1-2 days);
- rapid tests for streptococcus, allowing diagnosis within 10-15 minutes1,2;
- swab from the throat on a Lefler stick (to exclude diphtheria).
Based on the results obtained, treatment for acute tonsillitis is prescribed.
Up to contents
A little anatomy
The pharynx is part of the respiratory tract and digestive tract. It contains a whole complex of lymphoid formations called the Pirogov-Waldeyer pharyngeal ring. The ring includes the palatine, pharyngeal, lingual, tubal tonsils, as well as lymphoid granules and ridges that are located on the lateral walls of the pharynx.
The tissues of the pharynx are penetrated by a huge number of blood vessels. Their superficial location provides warming or cooling of the air inhaled through the mouth and nose. In contact with the mucous membrane, the air is cleared of dust, chemical impurities and various microorganisms. Dust particles, substances and microbes settled on the mucous membrane irritate it, which sometimes causes inflammation and redness of the throat1.
Up to contents
Treatment of sore throat in children
Mild forms of the disease can be managed at home, under the supervision of a local doctor3. An exception is sore throats in children under one year of age: they need to be treated only in a hospital3.
Moderate and severe tonsillitis at any age is an indication for hospitalization, as are any forms of inflammation in children with immunodeficiencies, developmental defects and diseases of the nervous system3.
Mode
In the first 3-4 days of illness, bed rest is indicated2.
Diet
The diet is gentle, with a predominance of dairy and vegetable dishes, limiting salt, sugar, and excluding spices and herbs.
Drink plenty of fluids
It prevents dehydration due to fluid loss during fever and helps reduce symptoms of intoxication.
Antibacterial and antiviral therapy
Bacterial inflammation requires treatment with antibacterial drugs in the form of tablets, injections or intravenous infusions - it is prescribed by a doctor. Regardless of how long the temperature lasts, if a child has a sore throat, the duration of treatment with antibiotics is at least 10 days2,3.
It makes no sense to give your baby antiviral drugs, since respiratory viruses, which most often cause tonsillitis, are practically insensitive to them1. In addition, viral forms of the disease are mild1,2.
Antipyretic drugs
WHO recommends the use of antipyretic drugs in previously healthy children only if the temperature rises above 390 C, and if heat is poorly tolerated: headache, aching muscles and joints2. For babies under one year of age, as well as children prone to seizures, fever medicine should be given earlier - as soon as the temperature reaches 380 C.
In other cases, you need to use physical methods to combat the fever: light clothing, a fan, rubbing, cold compresses on the forehead, armpits and groin area2.
Local treatment
It includes gargling with special solutions, irrigating the tonsils, and sucking special tablets containing antiseptic, anti-inflammatory and analgesic components.
To gargle with a sore throat, children from the age of three can use HEXORAL® SOLUTION for gargling based on hexethidine5. Hexetidine is active against bacteria, including beta-hemolytic streptococcus, respiratory viruses and fungi, and has a mild analgesic effect, so it can be used as an adjunct to the main treatment of tonsillitis5.
HEXORAL® SOLUTION is not suitable for children who, due to age and lack of skill, simply do not know how to gargle. For such cases, there is HEXORAL® in the form of an AEROSOL, which is evenly sprayed over the entire surface of the pharyngeal mucosa and provides the necessary therapeutic effect6.
For a 4-year-old child, HEXORAL® TABS7 is suitable, and for sore throat in a child 6 years of age and older, HEXORAL® TABS CLASSIC8. HEXORAL® TABS7 contains, in addition to the antiseptic component, the local anesthetic benzocaine, which helps fight sore throat and facilitate swallowing7,8. The composition of HEXORAL® TABS CLASSIC8 includes two antiseptic components, amylmetacresol and dichlorobenzyl alcohol, which enhance the antiseptic effect of each other. The pleasant orange, lemon, honey-lemon, and blackcurrant taste of the tablets is usually liked by children and encourages them to undergo treatment8.
HEXORAL® TABS EXTRA is intended for children over 12 years of age9. It contains lidocaine, a powerful pain reliever that helps fight even the most severe sore throat9.
Please note that after using the drugs, the patient should not be allowed to eat or drink for half an hour.
Up to contents
Why does ARVI selectively affect people?
Having been chilled outside, we try to warm up at home with hot tea and take a bath, but, unfortunately, these simple but effective procedures do not help everyone. This fact is explained by the general health of a particular person. Hypothermia of the body only triggers the mechanism of a cold, but the nature of the further development of the disease is determined by other reasons.
- A hypothermic body is easily affected by respiratory viruses, including the influenza virus. Entering into a favorable environment, pathogenic microflora begins to actively multiply.
- Susceptibility to infection is largely determined by the state of the immune system. For example, chronic diseases significantly weaken the body’s ability to fight viruses and bacteria that have entered it.
- Patients with enlarged tonsils or with constantly inflamed sinus mucosa are much more likely to be exposed to ARVI. Hypothermia will cause an exacerbation of chronic diseases in them.
- The state of the gastrointestinal tract also affects the level of immunity. The likelihood of catching a cold increases significantly with dysbiosis caused by taking antibiotics or internal causes.
- It is no secret that the likelihood of contracting ARVI increases when a person is in a stressful situation and experiences strong psycho-emotional stress.
The body's reaction to the active activity of pathogenic microflora will also be different.
Complications of sore throat
The reason for the development of complications is often a late start of treatment, incorrect selection of antibiotics and a sharp weakening of the immune system2.
- Streptococcus has an allergenic effect on the body3, creates the preconditions for the development of nephritis (inflammation of the kidneys), myocarditis (inflammation of the heart muscle), rheumatism, manifested by the development of heart defects and inflammation of the joints, systemic connective tissue diseases, such as systemic lupus erythematosus, Sjogren's syndrome, systemic vasculitis , scleroderma.
- Aggressive streptococcus can penetrate from the tonsils into the surrounding tissues, causing the formation of paratonsillar and retropharyngeal abscesses, periadenitis (inflammation of the lymph nodes), phlegmon - diffuse purulent inflammation of the tissues.
- The list of complications of tonsillitis includes otitis (inflammation of the middle ear), sinusitis (damage to the paranasal sinuses).
- The infection can enter the blood, spread throughout the body and cause the formation of purulent foci in other organs (septicopyemia).
Sore throat and acute tonsillitis in children should be taken seriously.
Consultation with a pediatrician and ENT doctor is necessary in any case, even if at first glance the patient’s condition does not cause much concern!
Self-medication is fraught with the development of complications - all parents should understand this.
Up to contents
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Literature
- T.I. Garashchenko. Sore throats in children and their systemic antibacterial therapy. Consilium Medicum. Pediatrics. (Add.) 2008; 02: 14-20.
- E. I. Krasnova, N. I. Khokhlova. Differential diagnosis and treatment tactics for acute tonsillitis (angina) at the present stage. Attending physician No. 11/2018; Page numbers in the issue: 58-63.
- Clinical recommendations (treatment protocol) for providing medical care to children with tonsillitis (acute streptococcal tonsillitis), FSBI NIIDI FMBA of Russia, 2015.
- Tatochenko V.K.. Once again about antipyretics. Issues of modern pediatrics. Volume 6 No. 2 2007, p. 128-130.
- Instructions for the drug HEXORAL® SOLUTION.
- Instructions for the drug HEXORAL® in AEROSOL form.
- Instructions for the drug HEXORAL® TABS.
- Instructions for the drug HEXORAL® TABS CLASSIC.
- Instructions for the drug HEXORAL® TABS EXTRA.
Up to contents
Causes of red throat
Redness of the throat may be due to factors unrelated to infection2:
- Mechanical injuries to the mucous membrane of the pharynx due to solid food and bones.
- Eating hot food that can cause thermal burn2.
- Irritation or burn of the pharynx with chemicals (acids, alkalis, alcohol-containing liquids)2.
- Eating excessively spicy foods (hot pepper, ginger, horseradish, mustard can cause irritation of the mucous membranes).
- Inhalation of tobacco smoke, dust or air contaminated with mechanical and chemical impurities.
Eating food containing red food dyes. In this case, the throat is red, but does not hurt.
Up to contents