Chronic cholecystitis is an inflammation of the walls of the gallbladder, which is accompanied by disorders of the biliary system of a motor-tonic nature. This disease occurs quite often. In order to recognize it in time and take appropriate measures, you need to know its main symptoms and methods for diagnosing chronic cholecystitis.
Causes of chronic cholecystitis
Chronic cholecystitis is based on opportunistic microflora:
- staphylococci,
- streptococci,
- Escherichia,
- Pseudomonas aeruginosa,
- enterococci
Sometimes the cause may be bacterial pathogenic microflora, in particular salmonella, shigella, protozoal or viral infection. There are three main ways for microbes to enter the body:
- hematogenous,
- contact,
- lymphatic.
Parasites also provoke cholecystitis. Damage to giardiasis, opisthorchiasis, ascariasis, fascioliasis, strongyloidosis. These parasites lead to partial obstruction of the bile duct. Ascariasis provokes a cholangiogenic process, fascioliasis leads to cholangitis, and with giardiasis the function of the bile ducts is impaired.
Cholecystitis always begins with disturbances in the outflow of bile. It stagnates, in connection with this, cholelithiasis, GIVP, which are the immediate precursors of chronic cholecystitis, can develop. But there is also a reverse movement of this process. Due to chronic cholecystitis, pancreatic motility slows down, bile stagnation develops, and stone formation increases.
In the development of this pathology, nutritional disorders play an important role. If a person eats large portions with significant intervals between meals, if he gorges himself at night, eats fatty, spicy foods, or eats a lot of meat, then he is at risk for developing cholecystitis. He may develop a spasm of the sphincter of Oddi, and bile stagnation may occur.
Causes
Doctors identify several main risk factors for the incidence of chronic calculous cholecystitis:
- middle and old age;
- pregnancy and childbirth;
- overweight and obesity;
- too sudden loss of body weight;
- starvation;
- total parenteral nutrition;
- family history, heredity;
- taking a number of medications (fibrate derivatives, contraceptive steroids, estrogens during the postmenopausal period, progesterone, octreotide and its analogues, ceftriaxone);
- Crohn's disease, diabetes mellitus, liver cirrhosis, biliary system infections, choledochal and duodenal diverticula.
Signs of cholecystitis
Taking certain medications can trigger the development of cholecystitis
Any signs of cholecystitis do not appear immediately. They make themselves felt gradually. First, atony or hypotension of the neuromuscular base of the gallbladder develops. Inflammation of its mucous membrane begins after the spread of microbes.
Then the inflammation affects the submucosal layer and moves to the muscle layer. Thus, inflammation gradually affects all layers of the wall of the pancreas. Infiltrates are formed there, connective tissues grow pathologically.
If the transition to the serous membrane is allowed, adhesions with the liver capsule and other organs will appear. Inflammation will affect the intestines, duodenum, and stomach. This condition is usually called pericholecystitis. In this situation, the condition may not be limited to catarrhal inflammation; phlegmous or gangrenous manifestations appear.
In advanced cases, the integrity of the walls of the gallbladder is compromised due to abscesses, ulcerations, and foci of necrosis. The gangrenous form is the rarest development of this pathology. Its cause is an anaerobic infection. This form ends with putrefactive destruction of the walls of the bladder.
With chronic cholecystitis, the disease lasts a long time. Periodically, the symptoms appear more clearly, and periodically subside.
All manifestations of cholecystitis are due to the fact that this pathology leads to difficulty in the outflow of bile from the gallbladder. This is accompanied by dyskinesia, which leads to the inability of bile to enter the duodenum.
Acute cholecystitis - symptoms and treatment
Patients with acute cholecystitis are subject to emergency hospitalization in the surgical department of the hospital. After carrying out the necessary diagnostic measures, further treatment tactics are determined. In the presence of severe complications - perivesical abscess, destructive cholecystitis with peritonitis - patients are subject to emergency surgery after short-term preoperative preparation.[1]
Preparation consists of restoring the volume of circulating blood, detoxification therapy by infusion of crystalloid solutions in a volume of 2-3 liters. If necessary, correction of cardiac and respiratory failure is carried out. Perioperative antibiotic prophylaxis is performed (before, during and after surgery).
The surgical approach is selected depending on the technical capabilities of the clinic, the individual characteristics of the patient and the qualifications of the surgeon. The most commonly used is the laparoscopic approach, which is the least traumatic and allows for full inspection and sanitation.[12]
The mini-access is not inferior to the laparoscopic approach in terms of morbidity and has the advantage of eliminating the need to apply pneumoperitoneum (limit the mobility of the diaphragm).[10] If technical difficulties arise, severe adhesions in the abdominal cavity and diffuse peritonitis, it is more advisable to use a laparotomic approach: upper midline laparotomy, Kocher, Fedorov, Rio Branca access. In this case, the upper midline laparotomy is less traumatic, since in this case the muscles are not intersected, however, with oblique subcostal approaches, the subhepatic space is more adequately opened for surgical intervention.
The operation consists of performing a cholecystectomy. It should be noted that the presence of perivesical infiltrate implies certain technical difficulties in mobilizing the neck of the gallbladder. This leads to an increased risk of damage to elements of the hepatoduodenal ligament.[13] In this regard, one should not forget about the possibility of performing cholecystectomy from the fundus, which allows for more clear identification of the elements of the cervix.[16]
There is also the “Pribrama” operation, which consists of removing the anterior (lower) wall of the gallbladder, suturing the cystic duct in the neck area and mucoclasia (removal of the mucous membrane) by electrocoagulation of the posterior (upper) wall. Performing this operation with a pronounced infiltrate in the area of the bladder neck will avoid the risk of iatrogenic damage. It is applicable for both laparotomic and laparoscopic approaches.
If there are no severe complications of acute cholecystitis, then upon admission of the patient to the hospital, conservative therapy , aimed at unblocking the gallbladder. Antispasmodics, anticholinergics, infusion therapy are used to relieve intoxication, and antibiotics are prescribed.
An effective method is to block the round ligament of the liver with a solution of novocaine. The blockade can be performed either blindly using a special technique, or under the control of a laparoscope when performing diagnostic laparoscopy and under ultrasound guidance.
If conservative therapy is ineffective within 24 hours, the question of radical surgery—cholecystectomy—is raised.
Of no small importance for determining treatment tactics is the time that has passed since the onset of the disease. If the interval is up to five days, then cholecystectomy is feasible; if it is more than five days, then it is better to adhere to the most conservative tactics in the absence of indications for emergency surgery. The fact is that in the early stages the perivesical infiltrate is still quite loose, it can be divided during surgery. Later, the infiltrate becomes dense, and attempts to separate it may result in complications. Of course, a period of five days is quite arbitrary.
If there is no effect from conservative treatment and there are contraindications for radical surgery - severe pathology of the cardiovascular and respiratory systems, five days have passed since the onset of the disease - it is better to resort to decompression of the gallbladder by applying cholecystostomy.[4]
Cholecystoma can be performed in three ways: from a mini-access, under laparoscopic control and under ultrasound control.[9] The most minimally traumatic procedure is to perform this operation under ultrasound guidance and local anesthesia.[3] Single and double punctures of the gallbladder with sanitation of its lumen under ultrasound guidance are also effective.[7] A necessary condition is the passage of the puncture channel through the liver tissue to prevent bile leakage.
After stopping the acute inflammatory process, radical surgery is performed in a cold period after three months. Usually this time is enough for the perivesical infiltrate to resolve.
Pain syndrome with cholecystitis
You can recognize this disease by its rather characteristic pain. They are felt in the right hypochondrium. Sometimes they are well felt in the epigastric region. The pain often radiates to the scapula, shoulder, and collarbone on the right. Very rarely the pain reaches the left hypochondrium. Pain manifests itself if the diet is disrupted. When a sick person eats fatty, fried, spicy, eggs or drinks beer, carbonated drink, wine, cholecystitis will manifest itself with severe pain. Such manifestations are caused by severe cooling, stress, and physical overexertion.
Pain manifests itself depending on where the source of inflammation is located, what size it is, and how severely dyskinesia has developed.
If inflammation occurs in the cervix or in the duct, the pain will be very severe and manifest itself in separate attacks. If the lesion affects the body of the bladder itself or its bottom, then the pain will be permanent.
If dyskinesia is hypotonic in nature, then the pain will not be very acute, but it will become annoying, nagging, and almost constant. With pericholecystitis, the pain becomes aching and does not leave the patient for a second. If the patient is disturbed (driving in a shaking car, bending, turning), it will be felt more clearly.
Diagnostics
Diagnosis of cholelithiasis is based on the clinical picture, as well as data obtained during an instrumental examination. To make a diagnosis with sufficient accuracy, it is enough to perform an ultrasound of the upper abdominal cavity. With its help, you can identify stones in the ducts, gall bladder, determine the size of the bladder, its walls, the condition of the pancreas and liver. Gastroduodenoscopy is also performed to determine the condition of the mucous membrane of the stomach, esophagus and duodenum. If there are complications, retrograde cholangiography or transgastric ultrasound of the bile ducts is prescribed to detect choledocholithiasis.
Dyspeptic syndrome
With cholecystitis, dyspeptic syndrome often manifests itself. It makes itself felt by a bitter taste in the mouth and regular bitter belching. This is accompanied by unpleasant sensations of a bloated abdomen, stools are disturbed, and the intestines are distended. Sometimes it starts to feel nauseous, and there may be bitter vomiting. If the gallbladder is in a state of atony or hypotension, then after vomiting relief may occur: relief of heaviness, reduction of pain.
If dyskinesia is hypertensive in nature, then vomiting only makes it worse and the pain becomes stronger. By the amount of bile in the vomit, you can determine the degree of bile stagnation. Its quantity directly depends on this. The greater the stagnation, the more bile there will be in the vomit.
Vomiting occurs after strong experiences, against the background of eating prohibited foods, or due to physical overload.
Causes of acute phlegmonous calculous cholecystitis
The formation of stones in the gall bladder provokes acute phlegmonous calculous cholecystitis
The causes of this condition can be divided into two groups: those that provoke the appearance of stones and those that promote the accumulation of pus.
There are also factors that equally influence both of these processes. In general, stones play a dominant role in the formation of phlegmonous cholecystitis.
Reasons for their formation:
Inflammatory-intoxication syndrome in cholecystitis
If cholecystitis worsens, body temperature rises. The temperature rises slightly: to subfebrile levels. This happens in the case of catarrhal inflammations. If cholecystitis becomes destructive or complications begin, the temperature rises to febrile levels.
With purulent inflammation, the condition worsens sharply. Weakness, sweating, chills are observed, and a hectic temperature curve is formed. This condition occurs with gallbladder epiema or liver abscess.
If the body’s reactivity is reduced (this happens with general weakness, as well as in old age), then even with a purulent lesion, the temperature may not rise at all or rise only to subfebrile levels.
Description of the disease
Symptoms of the disease appear suddenly
Cholecystitis is an inflammation of the gallbladder. It can be acute, when symptoms of the disease appear suddenly, or chronic, when the disease is present and progresses for the rest of the patient's life.
Calculous cholecystitis or cholelithiasis is a disorder of the processes of bile formation, in which water is excessively absorbed and stones are formed. They can cause serious digestive disorders and biliary colic.
Infection provokes purulent cholecystitis, and its most dangerous type is phlegmonous cholecystitis, in which pus accumulates in the gallbladder.
In combination with gallstones, this leads to severe symptoms and a serious condition for the patient. There is a risk of serious complications from both the digestive system and the liver.
Atypical cholecystitis
In a third of all patients with cholecystitis, the disease proceeds according to a non-standard pattern. There is a cardiological form. It manifests itself in severe pain in the areas of the heart. Moreover, such sensations appear after eating. This is especially often felt when you lie down to rest after eating. Arrhythmias, in particular extrasystoles, are possible. The ECG shows flattening and even inversion of the T wave.
There is also an esophagalgic form. It causes heartburn and a dull pain behind the sternum. Patients complain that after eating they get a “stake” behind their sternum. The pain may not go away for quite a long time. It may even be difficult to swallow food.
An intestinal form is also found. The pain in this case is not severe, does not have a clear localization, and can be felt throughout the abdomen. Patients complain of constipation and bloating.
2. Symptoms of the disease
Cholangitis is characterized by a sudden onset. The patient may quickly develop the following symptoms of cholangitis:
- A sharp increase in body temperature, accompanied by chills;
- Spasmodic pain in the right side of the abdomen;
- A sharp drop in blood pressure;
- Nausea and vomiting;
- Weakness.
In addition, with cholangitis, liver failure develops, which is characterized by impaired consciousness, skin itching and jaundice.
Visit our Hepatology page
Laboratory methods for diagnosing chronic cholecystitis
When the exacerbation stage occurs, signs of an inflammatory process appear in the blood test: ESR increases, neutrophilic leukocytosis appears, and the leukocyte count shifts to the left. Eosinophilia develops. If the disease is complicated, then increased cholesterol and bilirubin will be observed.
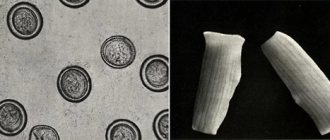
Duodenal intubation allows you to examine bile and get a more accurate picture of what is happening. If the bile is cloudy, contains mucus, flakes, cellular detritus, columnar epithelium, then inflammation is occurring. True, the signs do not speak of cholecystitis itself, but of duodenitis, which always accompanies this disease. If during a bile microscope a huge number of eosinophils are noted, one can assume that there are parasites in the internal organs.
If cholesterol or calcium bilirubinate crystals are detected, this indicates that stone formation, which is associated with a predisposition to cholestasis, can be predicted.
A bacteriological examination of bile is required. It allows you to determine which infection caused the disease, as well as determine how sensitive the flora is to antibiotics.
4. Treatment of cholangitis
Treatment for cholangitis is surgical. First, the cause of bile stagnation is eliminated and its outflow is restored. The operation is usually performed laparoscopically.
After this, it is necessary to remove the intoxication. If cholangitis is caused by bacteria or parasites, then antibiotics or antiparasitic drugs are prescribed.
For primary sclerosing cholangitis, treatment consists of taking ursodeoxycholic acid drugs.
To ensure that cholangitis does not have to be treated at all, prevention is recommended. First of all, timely treatment of pancreatitis, cholecystitis and cholelithiasis is necessary.
Popular questions about calculous cholecystitis
What is calculous?
The term means that the cause of an acute or chronic inflammatory process lies in stones formed inside the gallbladder.
How much water should you drink if you have cholecystitis?
During an attack, it is recommended to drink as much mineral water as possible without carbon. Water is especially useful after a bout of vomiting.
What can you eat with acute cholecystitis?
Doctors recommend limiting food intake and eating foods that do not cause increased bile secretion.
Treatment
If acute cholecystitis is diagnosed, how to treat it
? Under no circumstances should you self-medicate. If symptoms appear, you should immediately seek help from a specialist. After all, improper relief of pain can lead to further diagnostic errors. This will dull the pain and the doctor may miss the development of peritonitis. Often the inflammatory process affects muscle tissue, which subsequently leads to the development of gangrenous cholecystitis and peritonitis. Peritonitis quite often leads to the death of the patient.
treatment of acute cholecystitis
The main method of treatment is surgery with removal of the entire gallbladder.
To become a client of the EL Clinic clinic, you just need to call our contact number. Experts will identify the causes of acute cholecystitis
and prescribe effective treatment.