- home
- Gynecology
- Ovarian cancer
- Treatment of ovarian cancer stages 3-4
My experience in laparoscopic surgical interventions for cysts, tumors and ovarian cancer is more than 800 operations, which is summarized in numerous scientific papers and monographs. I regularly conduct master classes on this topic for gynecologists and oncologists.
Three specialists are involved in choosing treatment tactics for patients with stage 3-4 ovarian cancer: a surgeon, an oncologist and a chemotherapist, with the obligatory participation of a highly qualified morphologist.
An effective approach in the treatment of ovarian cancer. Interval chemotherapy and laparoscopy. Professor Puchkov K.V.
Watch a video of my operations
You can ask questions and sign up for a consultation by phone: +7 (495)222-10-87
or fill out the form below
Thank you, your question has been sent successfully, we will contact you soon!
Ask a new question
Possible complications
With a significant accumulation of fluid in the abdomen, the functionality of the internal organs is impaired.
This applies not only to the abdominal organs, but also to the respiratory system. Restricted mobility of the diaphragm leads to pulmonary insufficiency and the formation of effusion in the pleural cavity. An increase in pressure in the hepatic portal vein system entails the passage of bacteria from the intestine into ascitic fluid, provoking the development of spontaneous bacterial peritonitis.
The terminal (last) stages of ascites entail a serious complication - hepatorenal syndrome. The concept implies a dysfunction of the excretory system up to renal failure. The exact reason for the development of this condition is not fully understood. Doctors believe that it occurs due to damage to the renal bloodstream, excessive use of diuretics and intravenous contrast.
What causes ascites to develop in cancer?
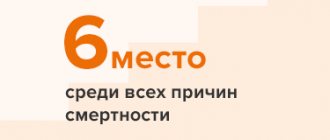
Pathological fluid accumulates in the peritoneum when the following organs are affected by the oncological process:
- appendages, ovaries;
- mammary gland;
- uterus;
- stomach;
- large intestine (mostly large intestine).
Ascites in oncology occurs due to the fact that the inner layer of the abdominal cavity (peritoneum) and the membrane covering the organs located in it are affected.
Malignant cells attach to the parietal and visceral layers of the peritoneum, which leads to impaired lymphatic drainage and impaired fluid absorption. The main causes of the pathological condition are neoplasms of the gastrointestinal tract (gastrointestinal tract) and tumors of the female reproductive system.
When liver tissue is damaged by cancer cells, another mechanism for the development of dropsy occurs. The venous system of the liver is pinched, disrupting venous circulation in the intestinal area. This option is more difficult and takes much longer. A sixth of the cases of fluid accumulation in the abdominal cavity in oncological pathologies occur in the form described above.
The cause of ascites in abdominal lymphoma is blockage and leakage of lymph from the intra-abdominal ducts.
Publications in the media
Ascites is an accumulation of fluid in the abdominal cavity. It can occur in any condition accompanied by generalized edema. In adults, ascites most often occurs with liver cirrhosis, heart defects, and nephrotic syndrome. In children, ascites is more often observed with nephrotic syndrome and malignant neoplasms.
Etiology and pathogenesis • Increased hydrostatic pressure •• Liver cirrhosis •• Hepatic vein occlusion (Budd-Chiari syndrome) •• Obstruction of the inferior vena cava •• Constrictive pericarditis •• Congestive heart failure •• Heart defects (stenosis or tricuspid valve insufficiency) • Decrease colloid osmotic pressure (albumin content <20 g/l) •• End-stage liver disease with decreased protein synthetic function •• Nephrotic syndrome with protein loss •• Nutritional disorders •• Enteropathies with protein loss •• Protein starvation • Increased permeability of peritoneal capillaries • • Tuberculous peritonitis •• Bacterial peritonitis •• Malignant diseases of the peritoneum •• Metastases into the peritoneum (ovarian, colon, pancreatic cancer, etc.) •• Obstruction of the lymphatic tract (leukemia, lymphoma) • Leakage of fluid into the abdominal cavity •• Chylous ascites (secondary to rupture of the lymphatic duct due to lymphoma or trauma) •• Urinary ascites • Other causes •• Myxedema •• Meig's syndrome •• Chronic hemodialysis.
Type of fluid contained in the abdominal cavity • Transudate (for congestive heart failure, constrictive pericarditis, liver cirrhosis, nephrotic syndrome, hypoalbuminemia) •• Indicators characteristic of transudate: ••• Protein <2.5 g% • Relative density 1.005–1.015 ••• Albumin/globulin ratio: 2.5–4.0 ••• Leukocytes up to 15 per field of view ••• Rivalta test is negative • Exudate (for tumor, tuberculosis, pancreatitis, myxedema, biliary pathology, Budd-Chiari syndrome) •• Indicators characteristic of exudate: ••• Protein >2.5 g% ••• Relative density >1.015 ••• Albumin/globulin ratio: 0.5–2.0 ••• Leukocytes over 15 in the field of view • •• The Rivalta test is positive.
Clinical picture • Discomfort or pain in the abdomen • Increased abdominal volume • Increased body weight • Anorexia, nausea, heartburn • Quick satisfaction of hunger while eating • Increased body weight • Dilated veins on the anterior abdominal wall (portocaval and cavacaval anastomoses) • Dullness to percussion sound in the lateral parts of the abdomen, moving when the body position changes (with a volume of ascitic fluid of at least 2 liters) • Edema of the penis, scrotum, lower extremities • Formation of umbilical, inguinal, femoral hernia • With tense ascites - a positive symptom of fluctuation • Shortness of breath, sometimes orthopnea • Formation of pleural effusion, wheezing in the lungs may be heard • Swelling of the neck veins.
Diagnostics. Ascites is indicated by abdominal enlargement, a positive symptom of fluctuation, or moving dullness detected by physical methods. An ultrasound scan reveals fluid in the peritoneal cavity. Paracentesis can be performed followed by analysis of ascitic fluid • The diagnostic sign of exudative ascites is an increase in the total protein content in the serum of more than 2.5 g%; usually seen with tumors, infections and myxedema. The difference between the level of albumin in the serum and the protein content in ascitic fluid less than 1 g/l indicates a high probability of the malignant nature of ascites, more than 1.1 g% indicates the presence of portal hypertension • With pancreatic ascites, the amylase content in the exudate is increased • With chylous ascites, it is increased concentration of fat (in the form of chylomicrons), chylous ascites develops with cirrhosis of the liver or lymphoma • Malignant tumors are detected by cytological studies of ascitic fluid, malignant ascites is also characterized by an increase in cholesterol content above 50 mg% • The number of leukocytes in ascitic fluid, exceeding 500 / μl, suggests presence of infection. A predominance of neutrophils suggests a bacterial infection, a predominance of lymphocytes is most likely due to tuberculosis or fungal infection • A red blood cell count greater than 50,000/µl indicates hemorrhagic ascites, usually due to malignancy, tuberculosis or trauma. Hemorrhagic pancreatitis, ruptured aortic aneurysm or liver tumors can cause overt bleeding into the abdominal cavity • The presence of a bacterial infection is confirmed by bacteriological examination of the exudate • A pH of ascitic fluid <7 suggests the presence of a bacterial infection.
Laboratory tests • Ascitic fluid •• Indicators that must be determined: ••• Total number of cells ••• Number of neutrophils ••• Total protein ••• Culture for cultivation (at least 10 ml) •• Indicators that facilitate diagnosis: • •• LDH content ••• Amylase content ••• Cultivation of acid-resistant and fungal flora ••• Cytology ••• Triglyceride content •• Additional studies of ascitic fluid ••• Helminths, talc granules ••• Presence of urine, blood ••• Embryonic oncological Ag >10 ng/ml (10 μg/l) • Blood - creatinine (<1.4 mg%), electrolytes • Urine •• sodium content in one sample: ••• <10 mEq/l (diuretics are ineffective) • •• 10–70 mEq/L (diuretics prescribed) ••• >70 mEq/L (diuretics not indicated).
Special studies • Laparoscopy • Ultrasound or CT • Diagnostic paracentesis.
TREATMENT depends on the cause of ascites.
A low sodium diet bread, etc.) •• Pickles, marinades, canned food, ham, pates, sausages, cheeses, sauces, mayonnaise, ice cream •• Candies, marshmallows, milk chocolate •• All cereals, except semolina and rice • Allowed •• Salt-free bread and butter •• Beef, rabbit meat, chicken, fish (100 g/day), one egg/day •• Sour cream, milk (1 glass/day) •• Fresh vegetables and fruits or in the form of compote.
Drug therapy
• If the daily sodium excretion is 5–25 mmol, potassium-sparing diuretics are prescribed: spironolactone 100–200 mg/day • After 4 days of treatment, it is necessary to consider the indications for prescribing furosemide 80 mg/day.
• When daily sodium excretion is less than 5 mmol, potassium-sparing and loop diuretics are prescribed - furosemide 40-160 mg/day every other day in combination with potassium chloride - 50 mmol potassium per day.
• While the patient has edema, daily diuresis of up to 3 liters is safe (weight loss of no more than 1.0 kg/day is acceptable) • After the edema disappears, daily diuresis should not exceed 800–900 ml (optimal weight loss is about 0.5 kg/day).
• In case of tense ascites, it is necessary to consider the indications for therapeutic paracentesis •• Tense ascites •• Ascites with edema • Contraindications to therapeutic paracentesis •• Cirrhosis of the Child group C liver •• Blood bilirubin above 170 µmol/l •• Prothrombin index (PTI) below 40 % •• Platelet count less than 40´109/l •• Blood creatinine above 3 mg% •• Daily sodium excretion less than 10 mmol.
• Therapeutic paracentesis •• The volume of fluid removed is 5–10 liters •• Simultaneously with the removal of fluid, salt-free albumin must be administered intravenously - 6 g per 1 liter of fluid removed.
Surgery. For chronic ascites that cannot be treated, abdominal-jugular shunting (Levine shunt) is possible, but there is a high risk of infection and disseminated intravascular coagulation.
Complications and their treatment • Spontaneous bacterial peritonitis •• Develops in 8% of patients with liver cirrhosis with ascites •• 70% of patients develop abdominal pain, fever, abdominal tenderness on palpation, sharp deterioration of condition •• Protein concentration in ascitic fluid is usually less than 1 g% •• Most often caused by a gram-negative pathogen from the intestinal group •• Immediate administration of antibacterial therapy is necessary when the number of neutrophils in ascitic fluid is more than 250 per μl •• Parenteral administration of third-generation cephalosporins, oral fluoroquinolones is effective • Development of hepatorenal syndrome (see Hepatorenal syndrome) .
Prevention • Do not force diuretic therapy!
Course and prognosis • The prognosis depends on the cause of ascites • In liver cirrhosis, the prognosis is unfavorable (two-year survival rate - 40%) • The presence of hepatic cell failure significantly worsens the prognosis • Mortality in spontaneous bacterial peritonitis reaches 50%, developed hepatorenal syndrome - 95%.
ICD-10 • R18 Ascites
Diagnostic methods in Medscan
The Medscan clinic implements the latest diagnostic techniques for visualization and clinical analysis of the test fluid. The clinic’s doctors use the following methods in their work:
- Physical examination. Examination of the patient allows you to determine the approximate level of accumulated fluid.
- Biochemical blood test - assesses the condition of the hepatobiliary system (liver functionality) and kidneys. A blood test gives an idea of its coagulability and the level of electrolytes.
- X-ray and ultrasound examinations of the abdominal organs visualize the accumulated fluid.
- CT and MRI will clarify the presence of ascites.
- Laparocentesis - the doctor pierces the abdominal wall with a special needle and analyzes the ascitic fluid. The procedure helps to determine the cause of ascites. It also determines whether the fluid is infected and whether abnormal cells are present in it.
Treatment methods in Medscan
Conservative therapy with diuretics is appropriate for the treatment of mild ascites. Up to 1 liter of fluid per day is removed in this way.
The main method of treating ascites in oncology is laparocentesis for therapeutic purposes (removal of pathological fluid). An exception is ovarian cancer. In such a case, cytoreductive surgery (removal of the maximum volume of the tumor and metastases) and chemotherapy are indicated.
For patients who are contraindicated for repeated laparocentesis, Medscan specialists prescribe peritoneal port systems and catheters. For people suffering from portal hypertension (with metastasis or carcinoma), doctors recommend diuretics - diuretics.
Literature on the topic “Laparoscopic operations for cancer and benign ovarian tumors”
- Puchkov K.V., Fumich L.M., Politova A.K., Kozlachkova O.P., Ryazantsev M.E., Osipov V.V. Surgical treatment of tumors and tumor-like formations of the ovaries using laparoscopic access // 50 years of Ryazan State Medical University: scientific results and prospects. - Ryazan, 2000. - Part 2. - P. 171-172.
- Puchkov K.V., Fumich L.M., Kozlachkova O.P., Politova A.K., Osipov V.V. Surgical treatment of tumors and tumor-like formations of the ovaries using minimally invasive technologies // Endoscopy in the diagnosis, treatment and monitoring of women's diseases / ed. IN AND. Kulakova, L.V. Adamyan. – M., 2000. – P.132-134.
- Puchkov K.V., Kulikov E.P., Fumich L.M., Kozlachkova O.P., Politova A.K., Osipov V.V. Modern approaches to surgical treatment of ovarian formations // Endoscopic surgery. – 2001. – T.7, No. 3. – P. 69.
- . Puchkov K.V., Fumich L.M. Laparoscopic approach in the surgical treatment of ovarian neoplasms: adequacy and prospects // Pacific Med. magazine - 2002. - No. 2 (special issue). – P.39-41.
- Puchkov K.V., Kulikov E.P., Fumich L.M., Politova A.K. Laparoscopic approach in the treatment of ovarian neoplasms. Does it solve the problems set by oncologists? // Laparoscopy and hysteroscopy in gynecology and obstetrics / ed. IN AND. Kulakova, L.V. Adamyan. – M.: PANTORI, 2002. – P.462-463.
- Puchkov K.V., Ivanov V.V., Tyurina A.A., Fumich L.M. Population composition and functional activity of immunocompetent cells in women with ovarian tumor formations during complex surgical treatment // New technologies in gynecology / ed. IN AND. Kulakova, L.V. Adamyan. – PANTORI. – M., 2003. – P.89-90.
- Puchkov K.V., Kolesov V.Yu., Kolesnikova N.O. Radiation diagnostics today - search, solution, prospect // Magnetic resonance imaging in a multidisciplinary clinical hospital. - Ryazan: GUZ ROKB, 2004.- P.3-7.
- Puchkov K.V., Ivanov V.V.. Technology of dosed ligating electrothermal effects at the stages of laparoscopic operations: monograph. - M.: ID MEDPRACTIKA, 2005. - 176 p.
- Puchkov K.V., Chernousova N.M., Andreeva Yu.E., Granilshchikova I.G., Politova A.K., Fumich L.G. Laparoscopic approach in staging and treatment of patients with malignant ovarian tumors. Surgeon’s tactics in non-specialized hospitals // 20 years of Clinical Hospital No. 1: Sat. scientific-practical works / State Unitary Enterprise “Medical Center”. Management of the affairs of the Mayor and the Government of Moscow. - M.: ID "MEDPRACTIKA-M", 2008. - P.51-55.
- Puchkov K.V., Chernousova N.M., Andreeva Yu.E., Politova A.K., Fumich L.G., Biryukov A.S. Staging and treatment of patients with malignant ovarian tumors using laparoscopic access. Questions of surgeon tactics in non-specialized hospitals // Moscow Surgical Journal. - 2008. - No. 4. — P.10 — 14.
- Puchkov KV, Podzolkova NM, Andreeva JE, Dobychina AV, Korennaya VV Laparoscopic treatment of rare forms of endometriosis. // 21st ESGE Annual Congress (Paris, 11-14 September 2012), p. 16-17.
- Puchkov K., Podzolkova N., Andreeva Y., Korennaya V. Laparoscopic minimally invasive surgical treatment for rare forms of endometriosis // Abstracts from the 1 European Congress on Endometriosis, 29 November- 1 December, 2012, Siena, Italy. Journal of Endometriosis, 2012; 4(4): – P.204-205.
- Puchkov K., Podzolkova N., Andreeva Y., Korennaya V., Dobychina A. Laparoscopic treatment of rare forms of endometriosis // Abstracts book of the 17th World Congress on controversies in obstetrics gynecology & infertility, 8-11 November, 2012, Lisbon, Portugal. – P.194.
- Vergote I, Trope CG, Amant F, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N.Engl. J. Med. 2010; 363:943-953.
- Kehoe S, Hook J, Nankivell M, et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomized, controlled, non-inferiority trial. Lancet 2015; 386: 249-257.
- Chi DS, Eisenhauer EL, Zivanovic O, et al. Improved progression-free and overall survival in advanced ovarian cancer as a result of a change in surgical paradigm. Gynecol. Oncol. 2009; 114: 26-31.
- Meyer L, Cronin A, Sun C, et al. Use and effectiveness of neoadjuvant chemotherapy for treatment of ovarian cancer. J Clin Oncol, published online before print September 6, 2016. doi:10.1200/JCO.2016.68.1239.
- Vergote I, Tropé CG, Amant F, Kristensen GB, Ehlen T, Johnson N, Verheijen RH, van der Burg ME, Lacave AJ, Panici PB, Kenter GG, Casado A, Mendiola C, Coens C, Verleye L, Stuart GC, Pecorelli S, Reed NS; European Organization for Research and Treatment of Cancer-Gynecological Cancer Group; NCIC Clinical Trials Group. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer.
Puchkov K.V., Politova A.K. Laparoscopic operations in gynecology: monograph. - M.: MEDPRACTIKA, 2005. - 212 p.
Puchkov K.V., Bakov V.S., Ivanov V.V. Simultaneous laparoscopic surgical interventions in surgery and gynecology: Monograph. - M.: ID MEDPRACTIKA - M. - 2005. - 168 p.
Puchkov K.V., Ivanov V.V.. Technology of dosed ligating electrothermal effects at the stages of laparoscopic operations: monograph. - M.: ID MEDPRACTIKA, 2005. - 176 p.