Pharmacological properties of the drug Eglonil
Neuroleptic drug. Sulpiride is a selective antagonist of dopamine D2/D3 receptors. In patients with psychosis with negative symptoms, sulpiride is effective at a dose of 150–600 mg/day; at this dose, sulpiride has virtually no effect on positive symptoms. At a dose of 0.6–1.6 g/day, it improves the condition of patients with acute or chronic psychosis with positive symptoms. Only very high doses of sulpiride have a sedative effect. After intramuscular administration at a dose of 100 mg, the maximum concentration of the drug in the blood plasma (about 2.2 mg/l) is achieved after 30 minutes. When taken orally, sulpiride is absorbed in the digestive tract within 4.5 hours, the maximum concentration of the drug in the blood plasma ranges from 0.5–1.8 mg/l after taking a dose of 200 mg. Bioavailability of oral forms is 25–35% with wide individual variations; the concentration of sulpiride in blood plasma is proportional to the dose. Sulpiride is rapidly distributed in body tissues, mainly in the kidneys and liver; a small amount penetrates the BBB. Less than 40% of the drug binds to plasma proteins; the distribution ratio of erythrocytes and blood plasma is 1. The amount of the drug that passes into breast milk is 1/1000 part of the daily dose. Sulpiride is poorly metabolized in the body. The half-life is 7 hours; volume of distribution at steady state is 0.94 l/kg (0.6–1.5 l/kg) body weight. Total clearance - 126 ml/min. Sulpiride is excreted mainly by the kidneys by glomerular filtration.
The use of antacids in the complex therapy of severe gastroesophageal reflux disease
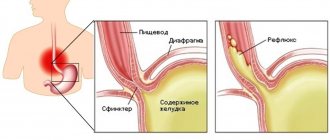
In the standard of care for gastroesophageal reflux disease (GERD), non-absorbable antacids are considered as an adjunct to course and maintenance treatment with proton pump inhibitors (PPIs). Antacids are recommended as an independent remedy only for minimally expressed symptoms of the disease [2, 7].
However, according to statistics, in 15% of patients, who often suffer from the most severe lesions of the esophagus, the use of PPIs in adequate doses does not lead to complete regression of symptoms and pronounced endoscopic dynamics. Upon closer examination of this category of patients, two reasons were identified that could explain the above phenomenon:
- resistance to the antisecretory agent used;
- the presence of severe duodenogastroesophageal reflux (DGER).
Resistance to modern PPIs is relatively low and, according to various authors, ranges from 1 to 3.5% [6]. The second component seems to us to be more significant, since bile reflux accompanies a wide range of gastroenterological diseases, in particular gastric and duodenal ulcers, dysfunction of the biliary system, cholelithiasis, chronic cholecystitis, chronic pancreatitis, and intestinal diseases accompanied by persistent flatulence.
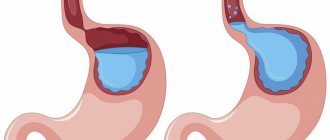
Components of duodenal contents act as aggression factors due to bile acids and lysolecithin. It is known that lysolecithin is a product of the hydrolytic breakdown of bile lecithin by phospholipase A. Further metabolism of lysolecithin is catalyzed by phospholipase B, which is inhibited by bile acids. Thus, the simultaneous presence of bile acids and lysolecithin in the refluxate leads to the accumulation of the cytotoxic effect of both substances in relation to the mucous membranes of the esophagus and stomach. Prescribing a PPI can reduce the total volume of secretion and thereby, to some extent, reduce the severity of DGER. Antacids containing aluminum and magnesium have a high adsorbing capacity and bind bile acids and lysolecithin by 59–96%, which makes it advisable to include them in complex treatment regimens for patients with severe BGE [3, 4, 8].
In addition, the use of antacid drugs in the form of a suspension promotes clearance (cleaning) of the esophagus. Along with this and the above properties, antacids also have a cytoprotective effect on the mucous membrane of both the esophagus and the stomach, which makes it possible to quickly achieve positive clinical and endoscopic dynamics of the disease [5, 9].
A separate, extremely difficult therapeutic group consists of patients who have undergone total gastrectomy. Due to the severity and constant presence of DGER, they often develop severe erosive and ulcerative lesions of the esophagus. Standard treatment regimens for GERD are ineffective in them, since in the case of total gastrectomy, PPIs do not have a point of application due to the lack of an anatomical substrate - parietal cells. To reduce the irritating effect of duodenal reflux, it is advisable to prescribe antacid, prokinetic and cytoprotective agents.
As an example, we give our own clinical observation.
Patient R., 51 years old, was admitted to the gastroenterology department of the State Clinical Hospital of the Ministry of Internal Affairs of the Russian Federation with complaints of constant heartburn, a feeling of bitterness in the mouth, weight loss, poor sleep, frequent awakenings at night due to a feeling of sourness in the mouth, and periodic bloating. Over the past month, I have developed a feeling of discomfort when swallowing food. Follows the 1st table diet.
In 2002, he underwent a total gastrectomy for moderately differentiated adenocarcinoma of the subcardial stomach. Since 2004, there have been complaints of periodically occurring persistent heartburn and a feeling of bitterness in the mouth in the morning. Esophagogastroduodenoscopy (EGDS) revealed slight hyperemia of the lower third of the esophagus and anastomositis. A monthly course of omeprazole 40 mg per day and motilium 30 mg per day was administered with a positive clinical effect; a control endoscopy was not performed. Since 2005, heartburn became permanent, and therefore the patient sought medical help at the clinic at his place of residence. Courses of omeprazole and motilium were prescribed, which brought relief while taking the drugs, but the clinical effect was not long-lasting. After 3 weeks from the start of conservative therapy, endoscopy revealed a linear erosion measuring 0.3 cm, which corresponded to GERD grade A according to the Los Angeles classification. Prescribed omeprazole 40 mg/day, motilium 30 mg/day, stricter adherence to the diet, split meals up to 6 times a day. During the control endoscopy performed after 3 weeks, negative dynamics were noted - three non-confluent erosions were identified at the tops of the mucosal folds up to 0.4–0.6 cm, covered with fibrin; the surrounding mucosa is swollen, moderately hyperemic. The endoscopic picture made it possible to diagnose GERD grade B. The gastroenterologist decided to intensify the therapy: esomeprazole 40 mg/day was prescribed, the dose of motilium was increased to 40 mg/day. A control endoscopy performed 2 weeks later showed an increase in the size of erosions to 0.6–1.0 cm, persistence of swelling and hyperemia of the esophageal mucosa. Rabeprazole 40 mg/day was prescribed, the patient continued to take Motilium at a dose of 40 mg/day. The patient did not notice any improvement in his state of health during the therapy. 2 weeks after the control endoscopy, the appearance of confluent erosions of the esophagus was noted, which corresponds to GERD grade C. The patient was sent to hospital for examination and selection of therapy.
On examination: the patient is very anxious, exhausted by constant heartburn, expresses cancer-phobic ideas, and does not believe in the possibility of successful therapy. Asthenized. The condition is assessed as moderate. The patient has the correct physique and low nutrition. The skin is clean, pale, with a grayish tint. Above the lung area there is a percussion-pulmonary sound. Breathing is vesicular, no wheezing. Heart sounds are muffled, the rhythm is correct. Blood pressure - 105/70 mm Hg. Art., pulse 68 beats/min. The tongue is moist, thickly coated with a white-yellow coating. The abdomen is soft and painless on palpation in all parts. The liver and spleen are not palpable. Physiological functions are normal.
In blood tests (general and biochemical), general urine analysis, no changes in indicators were noted.
Chest X-ray, ultrasound examination of the abdominal organs, genitourinary system and thyroid gland, colonofibroscopy, and osteoscintigraphy revealed no diagnostically significant abnormalities.
With endoscopy dated January 30, 2006: the esophagus is freely passable, from a distance of 28 cm from the teeth and to the esophageal-small intestinal anastomosis, confluent erosions with fibrin deposits and pronounced contact bleeding of the mucous membrane can be traced along all walls. The anastomosis is freely passable, the anastomosed colon is not changed. There is massive reflux of bile into the esophagus. Conclusion: condition after gastrectomy, erosive fibrinous esophagitis.
X-ray examination: the act of swallowing is not impaired. The anastomosis is freely passable. Severe reflux of contrast material into the esophagus. The folds of the distal esophagus are dilated and swollen. No changes were detected in the small intestine. Conclusion: condition after gastrectomy; pronounced reflux of contrast into the esophagus; esophagitis.
The patient was prescribed the following therapy: domperidone (Motilium) 10 mg - 4 times 30 minutes before meals, Relzer - 10 ml 6 times according to the scheme: in the morning on an empty stomach, 4 times 20-30 minutes after meals and at night, sucralfate (Venter ) 1 tablet 4 times between meals. Particular attention was paid to sedative therapy, since it is known that the instability of the patient’s psycho-emotional status provokes aggravation of motor disorders of the gastrointestinal tract. The patient was also observed by a psychotherapist. Sulpiride (eglonil) 100 mg 2 times a day and phenazepam 0.5 mg at night were prescribed.
During endoscopy, performed 10 days after the start of therapy, certain positive dynamics were noted - the erosive fields in the esophagus decreased. Contact trauma to the mucous membrane became less pronounced. Peristalsis is slightly reduced, but no zones of akinesia are noted. Therapy was intensified by taking Relzer 8 times, 10 ml, and tofisopam (Grandaxin) 50 mg 2 times a day.
During endoscopy performed before discharge, foci of mucosal hyperemia were visualized in the patient's esophagus at the site of healed erosions. The peristaltic wave in the esophagus is active, covering all the walls of the esophagus.
Achieving and maintaining stable remission of GERD in patients with a resected stomach is an extremely difficult therapeutic problem. The prescription of PPIs, which form the basis of standard regimens, should be carried out strictly individually, taking into account the scope of surgical intervention and the preservation of the acid-producing function of the stomach. In cases of total gastrectomy, their use is unjustified.
Often patients are neurotic due to debilitating, intractable heartburn. Therefore, treatment regimens must be comprehensive, including drugs with adsorbent, prokinetic, cytoprotective activity, as well as agents that normalize the condition of both the central and peripheral nervous systems.
A special place in therapy is occupied by non-absorbable antacid drugs, characterized by a combination of several therapeutic effects, which is especially important for patients with a resected stomach. This is a pronounced adsorbing ability, which causes a decrease in the cytotoxic effect of bile components, as well as a cytoprotective effect, enhanced in the case of Relzer due to flavonoids, saponins, phenocarbolic acids and selenium compounds contained in licorice glabra. The use of antacids in suspension form promotes esophageal clearance. The therapeutic effect of antacids can be enhanced through their combined use with drugs belonging to the group of cytoprotectors (sucralfate, bismuth tripotassium dicitrate, misoprostol) and act as an additional barrier to the action of aggressive components of the duodenum [10, 11].
The choice of the antacid drug Relzer in the patient described above is determined by both the composition of the drug and the form of release. The content of aluminum and magnesium hydroxides determines the rapid onset and pronounced duration of action of the drug, as well as high adsorbing capacity.
Simethicone introduced into the retzer adsorbs intestinal gases, which further reduces intra-abdominal pressure in patients suffering from flatulence, and, as a result, serves as the prevention of pathological reflux. But the main distinctive feature of the drug is the inclusion in its composition of licorice root powder, the plant ingredients of which make a significant contribution to the total pharmacological effect of the reltser. Terpenoids and higher fatty acids reduce gas formation in the stomach, significantly complementing the effect of simethicone. Flavonoids and saponins, along with a wide range of microelements that make up licorice, have an antioxidant effect, which accelerates the regeneration processes of the mucous membrane. Various polysaccharides contained in licorice enhance the enveloping effect of Relzer and, along with flavonoids and terpenoids, neutralize the hydrochloric acid of gastric juice in patients with preserved acid-forming function.
The drug correction of the psycho-emotional status in the clinical observation we presented was due to the fact that sulpiride, being a selective antagonist of dopamine receptors, has moderate neuroleptic activity in combination with some stimulating and thymoleptic (antidepressive) effects. This drug has been widely used in gastroenterology for a long time due to its pronounced prokinetic activity, realized through a “regulating” effect on the central nervous system. Phenazepam, which is an active tranquilizer, also has vegetotropic activity. Subsequently, the treatment regimen was supplemented with tofisopam (Grandaxin), which has an anxiolytic effect and is a psychovegetative regulator.
The given clinical example illustrates the role of duodenal reflux in the formation of pathological changes in the esophageal mucosa in patients who have undergone total gastrectomy, as well as the importance of including antacids in therapeutic regimens in this category of patients.
Literature
- Biliary sludge: from pathogenesis to treatment: method. recommendations // Center. Institute of Gastroenterology / Comp. Ilchenko A. A. et al. M., 2004. 32 p.
- Ivashkin V. T. et al. Diagnosis and treatment of gastroesophageal reflux disease: a manual for doctors. Ministry of Health of the Russian Federation. M., 2003. 30 p.
- Tkachenko E. I., Lisovsky V. A. Errors in gastroenterology. St. Petersburg: Nevsky Dialect, 2002. 397 p.
- Leuschner U. Practical guide to biliary tract disease. M.: GEOTAR-MED, 2001. 264 p.
- Minushkin O. N., Litvishchenko Yu. F., Digilova N. D., Minushkina L. O., Vydrych L. A. Modern aspects of antacid therapy. M., 1998. 59 p.
- Rapoport S. I., Lakshin A. A., Rakitin B. V., Trifanov M. M. pH-metry of the esophagus and stomach in diseases of the upper digestive tract / ed. Academician of the Russian Academy of Medical Sciences F.I. Komarov. M.: Publishing House Medpraktika-M, 2005. 208 p.
- Rational pharmacotherapy of diseases of the digestive system: a guide for practitioners / edited by. ed. V. T. Ivashkina. M.: Litterra, 2003. 1046 p.
- Guide to gastroenterology / edited by. ed. F.I. Komarova et al. T. 2: Diseases of the liver and biliary system. M.: Medicine, 1995. 528 p.
- Belousov Yu. B., Moiseev V. S., Lepakhin V. K. Clinical pharmacology and pharmacotherapy: a guide for doctors. M.: Universum, 1993. 398 p.
- Drug therapy for gastrointestinal and liver diseases. Ed. By M.Farting. 2001: 7–10.
- Scarpignato C. Antacids in treatment of gastroesophageal reflux disease. Basel. 1992: 153–181.
I. V. Mayev, Doctor of Medical Sciences, Professor D. T. Dicheva , Candidate of Medical Sciences, Associate Professor V. V. Krasnikov T. A. Buragina MGMSU, Glenmark Pharmaceuticals LTD, Moscow
Use of the drug Eglonil
Initial treatment is carried out with intramuscular administration of the drug, after which it is switched to oral administration. For neurotic, psychofunctional and psychoaffective disorders associated with somatic conditions: Adults - 100–200 mg/day. Children over 6 years of age: 5 mg/kg body weight per day (if necessary, this dose can be increased to 10 mg/kg). In acute and chronic psychosis, the dose is set in accordance with the prevailing symptoms: negative - 200-600 mg/day, positive - 800-1600 mg/day.
Eglonil (in gastroenterology)
Eglonil
(eng.
Eglonil
) - an antipsychotic, a dopamine receptor blocker, used in gastroenterology as a prokinetic agent.
Dosage forms and composition of Eglonil
Eglonil is (was) approved in Russia in the form of the following dosage forms:
- tablets containing 200 mg of active substance - sulpiride
- capsules containing 50 mg sulpiride
- solution for intramuscular administration, in the form of ampoules containing 100 mg of sulpiride each
- oral solution in 200 ml glass bottles containing 1 mg of sulpiride (5 mg of sulpiride in 1 ml of solution)
In addition, Eglonil tablets contain excipients: potato starch, magnesium stearate, talc, lactose monohydrate, colloidal silicon dioxide, hypromellose.
Indications for use of Eglonil
In psychiatry and neurology:
- all forms of schizophrenia
- acute delirious states
- depression and neuroses
In psychiatry and neurology (50 mg capsules):
- children over 6 years of age: severe behavioral disorders (agitation, self-harm, stereotypy), especially in combination with autism syndromes
In gastroenterology (only as an additional remedy):
- psychosomatic symptoms in peptic ulcers of the stomach and duodenum, hemorrhagic rectocolitis and other diseases.
Method of use of Eglonil and dose in the treatment of the digestive system
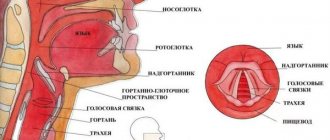
In the treatment of gastroenterological diseases, Eglonil is used only as part of complex therapy. Eglonil in the treatment of GERD
. One of the main reasons leading to an increase in spontaneous relaxations of the lower esophageal sphincter is an increase in the level of neuroticism in patients suffering from GERD; testing is relevant to assess the personality profile and correct the identified disorders. To assess the personality profile of patients with pathological gastroesophageal reflux identified by pH-metry, psychological testing is carried out, on the basis of which the dependence of the nature and severity of gastroesophageal reflux on individual personality characteristics is revealed and, along with standard therapy, patients with a depressive personality type are prescribed Eglonil 50 mg 3 times a day, which improves the prognosis of the disease (Maev I.V. et al.). In the presence of psychoform disorders in the form of anxiety, fear, irritability, masked and overt depression, Eglonil 50 mg 2-3 times a day for 3-4 weeks is widely used for GERD. Eglonil is an atypical analeptic; it has a prokinetic effect on the motility of the esophagus of the stomach and intestines due to the blockade of dopaminergic receptors, which explains its antiemetic effect. In addition, eglonil has axiolytic (anti-anxiety) and antidepressant effects (Degtyareva I.I.).
Egonil in the treatment of duodenostasis in combination with hypomotor dyskinesia of the gallbladder
. For compensated and subcompensated duodenostasis, the prokinetic agents metoclopramide or domperidone are prescribed, in addition to which it is possible, especially in the presence of depressive states, to use Eglonil 50 mg 2-3 times a day or 2 ml of a 5% solution intramuscularly 1-2 times a day (Maev I .V., Samsonov A.A.).
In the treatment of peptic ulcer with symptoms of vegetative neurosis in children
Eglonil 0.005 mg per kg of the child’s weight in 2 doses, morning and afternoon, gives a good effect (Shabalov N.P.).
Comparison of Eglonil with other drugs regarding the effect on the electrical activity of the upper gastrointestinal tract
Using the Gastroscan-GEM gastroenteric monitor, a comparative study of the effect of Eglonil, the “classical” prokinetic agent Motilium and the myotropic antispasmodic Duspatalin on the electrical activity of the upper gastrointestinal tract was carried out. The data obtained is shown in the table below:
| A drug | Group affiliation | Pi/Ps | Kritm | Ai/As | Pi/Pi+1 | |||
| stomach | DPK | stomach | DPK | stomach | DPK | stomach/duodenal | ||
| Eglonil | antipsychotic | pad | pad | pad | pad | pad | pad | No |
| Motilium | prokinetic | height | pad | height | height | height | height | norm |
| Duspatalin | myotropic antispasmodic | pad | pad | No | No | No | No | No |
Abbreviations: growth
- the indicator of peripheral electrogastrography increases after taking the drug,
decline
- decreases,
no
- the drug does not affect the indicator,
normal
- taking the drug normalizes the indicator. For indicators of electrical activity—peripheral electrogastrography indicators Pi/Ps, Kritm, Ai/As and Pi/Pi+1, see “Electrogastroenterography: study of the electrical activity of the stomach and intestines.” Duodenum - duodenum.
Eglonil reduces the electrical activity Pi/Ps, the rhythmicity of Kritm and the amplitude of contractions Ai/As of both the stomach and duodenum. Prokinetic Motilium increases the electrical activity of the stomach Pi/Ps and reduces the electrical activity of the duodenum, increases the rhythmicity of Kritm contractions of the upper gastrointestinal tract and normalizes the coordination of contractions of the stomach and duodenum Pi/Pi+1. The myotropic antispasmodic Duspatolin reduces the electrical activity of the stomach and duodenum Pi/Ps and does not affect the rhythm of Kritm and the coordination of contractions Pi/Pi+1 of the upper gastrointestinal tract (Smirnova G.O.).
Eglonil, like other prokinetics, have a predominantly stimulating effect on the smooth muscles of the gastrointestinal tract. In particular, it increases the tone and contractile activity of the stomach and duodenum, improves antroduodenal coordination, accelerates the evacuation of gastric contents and small intestinal transit (Avdeev V.G.):
Rice.
The effect of Eglonil on the motor function of the duodenum (Avdeev V.G.) a - motility on an empty stomach, b - motility after administration of Eglonil; 1 — manometry in the upper horizontal part of the duodenum; 2 — pH-metry in the upper horizontal part of the duodenum; 3 — pH-metry in the distal part of the duodenum. On the website gastroscan.ru in the literature catalog there is a section “Prokinetics”, containing medical articles concerning the treatment of diseases of the gastrointestinal tract with various prokinetics, including Eglonil.
general information
According to the pharmacological index, Eglonil belongs to the group “Neuroleptics”.
According to ATC, Eglonil is included in the group “N05A Antipsychotic drugs” and has the code “N05AL01 Sulpiride”. Eglonil is available from pharmacies with a prescription.
Other drugs containing the active ingredient sulpiride
The following drugs with the active substance sulpiride are (have been) registered in Russia: Betamax, Vero-Sulpiride, Prosulpin, Sulpiride, Sulpiride Belupo, Eglek.
In the USA, Canada and Australia, sulpiride is not approved for use. In many countries of the European Union, Latin America and Southeast Asia it is sold under the trade name Dogmatil. In the UK - Dolmatil, Sulpiride and Sulpor. In Japan - Abilit, Betamac T, Dogmatyl, Keityl, Margenol, Miradol, Pyrikappl, Skanozen, Sulpiride Choseido, Sulpiride Kyowa Yakuhin, Sulpiride Taisho, Sulpiride Taiyo, Sulpiride Towa Yakuhin, Youmathyle, as well as under many other trade names in various countries around the world .
Eglonil has contraindications, side effects and application features; consultation with a specialist is necessary.
Back to section
Side effects of the drug Eglonil
Sedation, drowsiness, early dyskinesia (spasmodic torticollis, oculogyric crises, trismus, which decrease with the administration of anticholinergic antiparkinsonian drugs), extrapyramidal symptoms, the severity of which partially decreases with the administration of anticholinergic antiparkinsonian drugs, tardive dyskinesia, which develops with long-term use of antipsychotics (anticholinergic antiparkinsonian drugs are ineffective and can worsen the patient’s condition), postural hypotension, impotence, frigidity, amenorrhea, galactorrhea, gynecomastia, hyperprolactinemia, weight gain.
Special instructions for the use of the drug Eglonil
If hyperthermia develops, sulpiride should be discontinued. Hyperthermia may be a manifestation of neuroleptic malignant syndrome (pallor, hyperthermia and autonomic dysfunction). This precaution is especially important when using the drug in high doses. Caution should be exercised when treating elderly patients who are more susceptible to the effects of the drug. Since sulpiride is excreted by the kidneys, in patients with severe renal failure the drug should be used in reduced doses and an intermittent treatment regimen should be used. Patients with epilepsy require more careful monitoring (clinical and, if necessary, EEG), since sulpiride reduces the seizure threshold. In patients with Parkinson's disease, sulpiride is prescribed with caution according to strict indications. In patients with aggressive behavior or agitation with impulsivity, sulpiride should be prescribed together with sedatives. In children whose mothers took low doses of sulpiride (approximately 200 mg/day) during pregnancy, no increase in the incidence of birth defects was observed. There is no experience with using the drug in higher doses. There is also no data on the potential effect of antipsychotic drugs taken during pregnancy on fetal brain development. It seems advisable, if possible, to reduce the dose and reduce the duration of treatment with the drug during pregnancy. In newborns whose mothers underwent long-term treatment with antipsychotics in high doses, several cases of the development of extrapyramidal syndrome have been described. It is recommended to monitor the neurological status of children born to mothers receiving the drug for some time after birth. Since sulpiride passes into breast milk, breastfeeding should be discontinued during treatment with the drug. Drivers of vehicles and persons working with potentially dangerous mechanisms should be warned about the possibility of developing drowsiness while taking the drug.
Antipsychotic drugs in the practice of a gastroenterologist: to be wary of or to prescribe
The mechanism of action of neuroleptics (antipsychotics) is complex and diverse, so their scope of use is not limited to the treatment of psychosis. Drugs of this group can be useful in somatic medicine, in particular gastroenterology, but are currently underused. The article discusses the indications for the use of antipsychotics in patients with gastroenterological diseases, provides recommendations on the choice of drug, determining its dose and duration of treatment. Particular attention is paid to potential side effects and prevention of their development.
The main antipsychotic drugs recommended for use in gastroenterological practice
It would not be an exaggeration to say that every practicing gastroenterologist asks himself the question: Should patients be prescribed antipsychotic drugs? Even if the effectiveness (often the necessity) of antipsychotics in gastroenterological practice is confirmed by clinical experience and they are included in the specialist’s treatment resource, this question arises in many clinical situations.
Concerns about antipsychotics stem from their wide range of “unusual” side effects. They can be overcome or minimized only through a careful assessment of the indications for use and the optimal choice of drug.
Indications for the use of antipsychotics in gastroenterological practice
Neuroleptics are a group of drugs whose main property is an antipsychotic effect aimed at reducing psychomotor agitation, emotional stress and aggressiveness [1]. In this regard, in recent years the term “antipsychotics” has been adopted in psychiatry. Neuroleptics are especially effective in relieving productive psychopathological disorders (delusions, hallucinations) and it is no coincidence that they occupy a central place in the treatment of schizophrenia and other psychoses. In somatic practice, including gastroenterology, it is advisable to leave the term “neuroleptics”. In contrast to the term “antipsychotics,” the term “neuroleptics” evokes less fear and rejection of the very idea of prescribing psychopharmacological drugs.
The mechanism of action of antipsychotics is complex and diverse, since it affects a large number of neurotransmitters (dopaminergic, cholinergic, adrenergic, serotonergic, GABAergic) that change neurochemical processes in various brain structures [2]. As a consequence, the scope of action of these drugs is not limited to the treatment of psychosis. Unlike psychiatric practice, in somatic medicine, antipsychotics are used in lower doses. In particular, in gastroenterological practice there are clinical situations that can only be resolved with the help of antipsychotics. We are talking primarily about diseases in which a variety of gastroenterological symptoms (abdominal pain, nausea, vomiting, diarrhea, etc.) are due to the somatic manifestation of mental disorders. It is believed that the incidence of mental disorders in gastroenterological patients is 50–60%. In such cases, mental spectrum diagnoses are justified: somatoform disorder, conversion disorder, anxiety-depressive disorder, somatogenically caused hypochondriacal personality development. However, being convinced of the presence of diseases of the digestive system, patients insist on observation and treatment by gastroenterologists and refuse consultation with a psychiatrist. More often in such situations, a gastroenterologist makes a diagnosis of a functional disorder in the digestive system. In addition to gastroenterological drugs, neuroleptics are introduced into the treatment regimen, without which it is almost impossible to achieve a positive result.
One more circumstance should be noted - the possibility of comorbidity between mental pathology and chronic diseases of the digestive system. As clinical observations show, it is not uncommon for patients to seek gastroenterological help and at the same time take antipsychotics if they have appropriate prescriptions from a psychiatrist. The drugs are used for a long time in monotherapy or in combination with antidepressants. In such situations, the gastroenterologist needs to know about the characteristics of the drug taken by the patient, its interaction with gastroenterological drugs and, most importantly, the early manifestations of possible side effects.
In addition, in small doses, antipsychotics can be a valuable addition to the treatment of exacerbation of any somatic disease, when the patient’s personality traits (excessive emotional intensity, fixation on negative aspects, tendency to aggressive reactions) negatively affect clinical dynamics [3].
It should be noted the properties of neuroleptics, which are of interest specifically in gastroenterological practice. These drugs are characterized by antiemetic (effective not only for vomiting, but also for debilitating nausea or persistent hiccups) and analgesic effects (in combination with analgesics, they relieve abdominal pain).
The anticholinergic (cholinergic or anticholinergic) effect of neuroleptics deserves special attention. When prescribed in adequate doses, this effect can be extremely useful in the treatment of functional pathology of the gastrointestinal tract (GIT) (esophagospasm, functional inflexion of the stomach, pylorospasm, duodenal dyskinesia, spastic type sphincter of Oddi dysfunction, biliary dyskinesia, intestinal dyskinesia) .
Functional symptoms are a consequence of hypertonicity of the parasympathetic division of the autonomic nervous system, the mediator of which is acetylcholine. Excessive release of acetylcholine causes hypertonicity of the smooth muscles of the gastrointestinal tract (spasm of different parts of the intestinal tube), acceleration of intestinal motility (diarrhea) and increased secretion of digestive juices (in particular, hypersecretion of gastric juice with all the ensuing consequences in the form of erosions and ulcers of the mucous membrane of the stomach and duodenum) . Neuroleptics are more effective than peripheral M-anticholinergics (methacin, platifillin, Buscopan), since not only the level of neuromuscular transmission in the periphery is affected, but also the central mechanisms of regulation of gastrointestinal tract functions.
Taking into account the above, the validity of the use of antipsychotics in gastroenterological practice is beyond doubt.
Potential side effects of antipsychotics
Relatively small doses of antipsychotics used in gastroenterological practice allow their use without the threat of serious complications. Unfortunately, the above does not apply to long courses of therapeutic doses of antipsychotics in psychiatric practice. In addition, it must be remembered that patients sometimes independently change the dosage regimen. In this case, increasing the dose of the drug is especially dangerous from the point of view of side effects.
Extrapyramidal disorders
Extrapyramidal disorders are considered the most dangerous [4, 5]. The minimum doses of drugs accepted in gastroenterological practice lead to these complications in the full clinical version extremely rarely. However, minimal neurological manifestations in the form of tension in individual muscles or difficult to explain general bodily tension or discomfort cannot be excluded, especially at the beginning of taking the drug.
Extrapyramidal disorders are usually divided into early (occurring during the first days or weeks after taking an antipsychotic or against the background of increasing its dose) and late (developing as a result of taking a drug of this group for several months or years).
The main extrapyramidal symptoms associated with the use of antipsychotics in psychiatric practice include kinetic disorders: involuntary contractions of various muscle groups throughout the body (acute dystonia), an irresistible need to move and change posture to reduce the feeling of internal discomfort (akathisia), various manifestations of bradykinesia ( stiffness and tension of muscles, slow pace of movements, disturbance of fine movements of the hand - neuroleptic parkinsonism).
Early dyskinesias are completely curable. With minor severity, in most cases their manifestations regress after discontinuation of the drug. When analyzing the response to neuroleptic therapy, it should be borne in mind that the development of early extrapyramidal disorders is a risk factor for the subsequent occurrence of late extrapyramidal disorders, which are much more severe in terms of treatment and prognosis.
Neuroleptic malignant syndrome
A special place among complications is occupied by neuroleptic malignant syndrome - a rare but life-threatening disorder in the form of acutely developed neurological (muscle rigidity), autonomic (hyperthermia with an increase to febrile values) and mental disorders of varying severity.
In general somatic practice, the only cause of the development of neuroleptic syndrome may be drugs that were forced to be used to relieve symptoms that developed as acute psychosis. Fortunately, such episodes are unlikely.
Endocrine and metabolic disorders
This type of disorder is due to the presence of a prolactin-stimulating effect in many neuroleptics, which develops due to the blockade of dopamine receptors. Hyperprolactinemia often develops in women and is manifested by menstrual irregularities (up to amenorrhea), lactorrhea of varying severity. External manifestations of hyperprolactinemia in men are gynecomastia, decreased potency, and rarely, lactorrhea. Such violations cause anxiety, reduce adherence to treatment and often lead to spontaneous drug withdrawal. It should be borne in mind that hyperprolactinemia associated with taking antipsychotics may be asymptomatic.
Possible side effects include impaired carbohydrate metabolism and metabolic disorders such as weight gain and dyslipidemia. However, they directly depend on the dose and duration of taking antipsychotics and rarely develop in somatic practice [6, 7].
Anticholinergic effect
The positive manifestations of the anticholinergic effects of antipsychotics were discussed above. Unfortunately, as its strength increases, side effects may develop [8], which are not always controllable. In such cases, slow motility can reach the level of persistent constipation. The most negative option is the development of dynamic intestinal obstruction. But that rarely happens. Discomfort can also be caused by a significant decrease in the secretion of the salivary glands, which is manifested by a feeling of dry mouth. By the degree of its severity in a particular patient, one can indirectly judge the strength of the anticholinergic effect of the drug.
The anticholinergic effect of neuroleptics is not limited to the gastrointestinal tract. Due to potential side effects in other organs and systems, contraindications to the use of these drugs are angle-closure glaucoma and prostate adenoma.
Sedative effect
Sedation is one of the typical unwanted (sometimes desirable) manifestations of neurolepsy. Sedation is usually observed in the first days of drug use and can sometimes adversely affect patient compliance. Antipsychotics with no pronounced sedative effect include tiapride and sulpiride.
Comparative characteristics of the main groups of antipsychotics
Currently, the most widespread division of this pharmacological group of drugs into first-generation (typical antipsychotics) and second-generation (atypical antipsychotics) antipsychotics [5, 9]. This division is not absolute, since there is no single expert opinion on this matter.
Modern atypical antipsychotics differ from their predecessors in the presence of a multireceptor profile, that is, binding to different types of receptors, and, most importantly, a lower degree of affinity for dopamine D2 receptors. Thanks to these physiological properties, the likelihood of developing side effects (neurological, endocrine, mental) is reduced, which improves drug tolerability. However, this is also not absolute. An example is tiapride (from the group of typical antipsychotics), which practically does not cause extrapyramidal disorders and hyperprolactinemia, and risperidone (an atypical antipsychotic), which leads to the development of hyperprolactinemia even to a greater extent than typical antipsychotics.
The group of atypical antipsychotics also has negative properties. In particular, metabolic disorders leading to obesity, diabetes mellitus and dyslipidemia are more often recorded with the use of these drugs. It should be emphasized that these undesirable effects develop only with long-term use of large doses of drugs that are used in psychiatric practice.
The difference in therapeutic properties is due to the peculiarities of the influence of individual drugs on the metabolism of neurotransmitters and, as a consequence, interaction with receptors in different brain structures. A deep understanding by a gastroenterologist of all aspects of antipsychotic therapy is hardly possible, but an understanding of the mechanisms of therapeutic action and side effects of various drugs is necessary.
Recommendations for prescribing antipsychotics in gastroenterological practice
Taking into account the presented recommendations, the likelihood of developing side effects of antipsychotics (especially severe ones) in gastroenterological practice is low. Nevertheless, the gastroenterologist must approach the prescription of antipsychotics responsibly.
Choice of drug
The Collection of instructional and methodological materials for primary care physicians on providing care to patients with non-psychotic mental disorders (2012) contains recommendations for non-psychiatrist physicians on the use of two antipsychotics: thioridazine (Sonapax) and tiapride (Tiapridal). At the same time, it is clarified that internists, in the absence of special knowledge, should not use other drugs [10]. However, actual clinical practice indicates that, in addition to these drugs, gastroenterologists often prescribe sulpiride (Eglonil) and alimemazine (Teraligen). The use of sulpiride is justified by its gastroprotective properties and moderate activating effect. When prescribing it, especially in daily doses exceeding 100 mg, it is necessary to take into account the possibility of extrapyramidal disorders (and the frequent development of hyperprolactinemia even when using small doses). In this regard, in most cases, it is advisable to replace sulpiride with tiapride, which has a similar spectrum of action and is practically free of such side effects.
Indications for the use of alimemazine (except for the usual ones for antipsychotics) are autonomic disorders. The addition of chlorprothixene to the recommended drugs is due to its pronounced sedative effect. This drug is especially effective for sleep disorders in the absence of results from the use of anxiolytic drugs.
Determination of the drug dose and duration of treatment
It is advisable to start treatment with a single dose. After five days, the dose should be increased. Average daily doses are presented in the table.
When treating gastroenterological patients, they usually focus on the lower level of daily doses, divided into two or three doses. If it is necessary to increase the dose, it is better to consult a specialist.
When prescribing an antipsychotic with a sedative effect (for example, chlorprothixene, thioridazine), it is necessary to warn patients about the possibility of developing sedation (in such cases, driving vehicles and working with machinery, which requires increased attention, is prohibited). You should also be warned about refusing to drink alcohol (due to the potentiation of its sedative effect).
Neuroleptics do not cause psychological addiction, addiction or dependence (like some anxiolytics and psychostimulants), or withdrawal syndrome [10]. On this basis, they can be taken for a long time. However, in gastroenterological practice, keeping in mind the potential side effects, it is better to limit yourself to short courses of 4–6 weeks. However, if necessary, the course of treatment can be extended or repeated.
Assessment of drug interactions between antipsychotics and gastroenterological drugs
Neuroleptics and drugs that stimulate gastrointestinal motility (prokinetics metoclopramide, domperidone) are similar in the mechanism of antiemetic action and the development of side effects. In this regard, their simultaneous administration is inappropriate.
The simultaneous use of neuroleptics and peripheral M-anticholinergics platiphylline, hyoscine butyl bromide (Buscopan), and belladonna preparations is contraindicated. This combination is fraught with serious anticholinergic complications of varying degrees of intensity (up to dynamic intestinal obstruction and acute urinary retention).
If antipsychotic therapy is necessary, along with taking antacids, activated charcoal or cholestyramine (which reduce the absorption of other drugs), it is recommended to take these drugs one hour or two hours after taking antipsychotics.
Situations requiring treatment adjustments
The prescription of antipsychotic drugs requires dynamic monitoring of the patient. At the same time, the focus should be not only on the assessment of therapeutic effects, but also on the timely identification of situations requiring treatment correction, namely:
- the occurrence of even minimal manifestations of extrapyramidal disorders or symptoms of hyperprolactinemia. This situation requires mandatory discontinuation of the drug; if the symptoms are severe, consultation with a psychiatrist is necessary;
- development of anticholinergic side effects. With minimal and moderate severity, you can limit yourself to reducing the dose of the drug, since these effects are dose-dependent. If the intensity of symptoms becomes alarming, the drug is discontinued;
- the occurrence of a sedative effect that interferes with the normal functioning of the body due to significant intensity. This effect can be minimized by shifting the daily dose of the drug to an evening dose or replacing the drug with an antipsychotic with less pronounced sedative properties.
Conclusion
Summarizing what has been said, it should be emphasized that in gastroenterological practice there are a number of situations when the prescription of antipsychotics can significantly increase the effectiveness of treatment. On this basis, drugs of this group can be considered an optimal (often underutilized) resource for the treatment of gastroenterological patients. The frequency of side effects of antipsychotics used in doses recommended for somatic practice is low (with the exception of frequent manifestations of hyperprolactinemia during sulpiride therapy). The risk of side effects can be reduced. To do this, when choosing a drug, one should take into account its potential undesirable effects in a particular patient, prescribe the minimum effective dose, gradually increasing it, and monitor the first manifestations of the negative effect of the drug. If questions arise, the gastroenterologist should seek help from a psychiatrist or psychotherapist.
Interactions of the drug Eglonil
Alcohol can potentiate the sedative effect of antipsychotic drugs, therefore, during treatment with sulpiride, patients should refrain from drinking alcohol and using medications containing ethyl alcohol. Levodopa has an antagonistic effect relative to antipsychotic drugs and vice versa. Patients with extrapyramidal symptoms due to the use of antipsychotic drugs should not be prescribed levodopa. If an antipsychotic drug is required in a patient taking levodopa for Parkinson's disease, it is recommended to choose a drug with mild extrapyramidal effects, in particular chlorpromazine or levomepromazine. Antihypertensive drugs may have additive hypotensive effects and increase the risk of postural hypotension. Drugs that cause central nervous system depression (morphine derivatives, most H1 receptor blockers, barbiturates, benzodiazepines, non-benzodiazepine tranquilizers, clonidine and related compounds) potentiate the depressing effect of sulpiride.
Eglonil®
Neuroleptic malignant syndrome
Neuroleptic malignant syndrome (NMS), which is a potentially fatal complication, and the occurrence of which is possible with the use of any antipsychotics, is characterized by pallor, hyperthermia, muscle rigidity, dysfunction of the autonomic nervous system, and impaired consciousness. Signs of autonomic nervous system dysfunction, such as increased sweating and lability of blood pressure and pulse, may precede the onset of hyperthermia and represent early warning symptoms. Cases with atypical manifestations of NMS without rigidity and increased muscle tone have been observed. In the case of hyperthermia of unknown origin, which can be regarded as either an early sign/symptom of NMS or atypical NMS, sulpiride should be immediately discontinued and medical monitoring of the patient should be established. The cause of the development of NMS remains unclear.
It is assumed that blockade of dopamine receptors in the striatum and hypothalamus plays a role in its mechanism; congenital predisposition (idiosyncrasy) cannot be ruled out. The development of the syndrome may be facilitated by intercurrent infection, dehydration, or organic brain damage.
QT prolongation
Sulpiride may cause QT prolongation. This effect is known to increase the risk of developing severe ventricular arrhythmias, such as torsade de pointes (see section "Side Effects").
Before using the drug, if the patient’s condition allows, it is necessary to exclude the presence of factors predisposing to the development of these severe rhythm disturbances (bradycardia less than 55 beats per minute; electrolyte disturbances, especially hypokalemia, hypomagnesemia; congenital prolongation of the QT interval, concomitant use of drugs that cause severe bradycardia (less than 55 beats per minute), hypokalemia, slowing of intracardiac conduction or prolongation of the QT interval) (see sections "Precautions", "Side effects").
Patients with the above risk factors should be careful when prescribing sulpiride.
Hypokalemia and hypomagnesemia should be corrected before starting the drug; In addition, medical supervision and regular monitoring of blood electrolytes and ECG should be ensured.
Except in cases of urgent intervention, patients requiring treatment with antipsychotics are advised to undergo evaluation and ECG monitoring.
Extrapyramidal syndrome
For extrapyramidal syndrome caused by antipsychotics, m-anticholinergic drugs (rather than dopamine receptor agonists) should be prescribed (see section “Interaction with other drugs”). In patients with Parkinson's disease or dementia with Lewy bodies, Eglonil® should be prescribed only when absolutely necessary (due to an increased risk of developing or exacerbating symptoms of extrapyramidal disorders).
Stroke
In randomized clinical trials comparing some atypical antipsychotics with placebo in elderly patients with dementia, a threefold increase in the risk of cerebrovascular events was observed. The mechanism of this risk is unknown. An increase in this risk cannot be ruled out with other antipsychotics or in other patient populations, so sulpiride should be used with caution in patients with risk factors for stroke.
Elderly patients with dementia
In elderly patients with dementia-related psychosis, an increased risk of death was observed when treated with antipsychotic drugs. An analysis of 17 placebo-controlled studies (average duration of more than 10 weeks) found that most patients treated with atypical antipsychotic drugs had a 1.6-1.7 times greater risk of death than patients treated with placebo.
In a 10-week placebo-controlled study, the death rate was 4.5% with atypical antipsychotics in these patients and 2.6% with placebo.
Although the causes of death in clinical studies with atypical antipsychotics varied, most causes of death were either cardiovascular (eg, heart failure, sudden death) or infectious (eg, pneumonia) in nature.
Observational studies have confirmed that, like treatment with atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may also increase mortality. The extent to which the increase in mortality may be due to the antipsychotic drug rather than certain patient characteristics is unclear.
Venous thromboembolic complications
Cases of venous thromboembolic complications, sometimes fatal, have been observed with the use of antipsychotic drugs. Therefore, sulpiride should be used with caution in patients with risk factors for the development of venous thromboembolic complications (see sections “With caution”, “Side effects”).
Mammary cancer
Sulpiride may increase the concentration of prolactin in the blood plasma. Therefore, when using sulpiride in patients with a history (including family history) of breast cancer, caution should be exercised (see section “With caution”). Such patients should be closely monitored.
Patients with epilepsy
Due to the fact that antipsychotics can lower the epileptogenic threshold, when prescribing sulpiride to patients with epilepsy, the latter should be under strict medical supervision.
Patients with Parkinson's disease taking dopamine receptor agonists
Except in exceptional cases, Eglonil® should not be used in patients with Parkinson's disease. If there is an urgent need for antipsychotic treatment in patients with Parkinson's disease taking dopamine receptor agonists, a gradual reduction in dosage of the latter should be carried out until complete discontinuation (abrupt withdrawal of dopamine receptor agonists may increase the patient's risk of developing NMS) (see sections "With caution", "Interaction" with other drugs").
Patients with impaired renal function
Reduced doses should be used (see section "Dosage and Administration").
Patients with diabetes mellitus or with risk factors for developing diabetes mellitus
Since the development of hyperglycemia has been reported in patients taking atypical antipsychotic drugs, patients with an established diagnosis of diabetes mellitus or with risk factors for its development who are prescribed treatment with sulpiride should monitor their blood glucose concentrations.
Ethanol consumption
The consumption of alcoholic beverages containing ethanol or the use of medications containing ethanol during treatment with Eglonil® is strictly prohibited.
Leukopenia, neutropenia and agranulocytosis
During therapy with antipsychotics, including Eglonil®, leukopenia, neutropenia and agranulocytosis were observed. The development of unexplained infections or an increase in body temperature may be signs of blood disorders, which require immediate hematological studies.
Overdose of the drug Eglonil, symptoms and treatment
Dyskinetic manifestations with spastic torticollis, tongue protrusion and trismus. Some patients sometimes develop severe manifestations of parkinsonism and coma. Eglonil is partially excreted during hemodialysis. Treatment is symptomatic: resuscitation measures, intensive care with constant monitoring of breathing and cardiac activity (with an increase in the Q-T ), which must be carried out until the patient’s complete recovery. If severe extrapyramidal symptoms develop, anticholinergic drugs should be used.