Competition "bio/mol/text"-2019
This work was published in the category “Visually about the beloved” of the “bio/mol/text” competition-2019.
The general sponsor of the competition and partner of the Skoltech nomination is the Skoltech Center for Life Sciences.
Competition sponsor: the largest supplier of equipment, reagents and consumables for biological research and production.
The audience award was sponsored by BioVitrum.
"Book" sponsor of the competition - "Alpina Non-Fiction"
Let's meet the heroes of our article
Shark is a T cell.
Squid - B cell.
The anglerfish is an APC (antigen presenting cell) with HLA I and HLA II (human leukocyte antigen).
Chimera is a DE cell (dual-receptor-expressing cell, “bi-receptor” cell) with a TCR (T-cell receptor) and a BCR (B-cell receptor).
In order to understand what the unique “bi-receptor” lymphocyte does in type I diabetes (T1DM), let’s briefly talk about how the immune system works.
Before us is a formidable predator of body tissues - the antigen-presenting cell ( APC ). It absorbs uninvited guests—pathogens, such as bacteria—by phagocytosis.
After digestion, it presents part of the pathogen protein - antigen . In addition to HLA II, there is HLA I. Their meaning and functions are described in more detail in the article “Immunity: the fight against strangers and... our own” [1]. The APC swims into the lymph follicle and attracts naïve T cells, which circulate freely throughout the body.
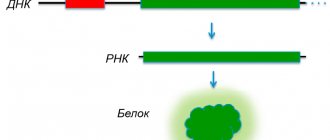
Normally, the main task of a T-lymphocyte is to bind an antigen that is not found in the body, but enters it during pathological processes. The diversity of T lymphocytes is very large. It is due to the diversity of T-cell receptors, which is obtained due to recombinations of several genomic regions and the insertion of random nucleotides into the TCR gene [2]. Each of the cells is slightly different from the others due to the hypermutability of a short fragment of the N-terminal domain of the receptor and is capable of recognizing its potential antigen. This means that there is a possibility that the APC will encounter a T cell whose TCR will bind to the antigen presented on the HLA. However, this also means that the TCR can also approach the peptide that is found in the body's own normal cells. But no. Such T cells usually die in the thymus during a process called negative selection.
Once HLA II binds to the TCR, the desired T cells proliferate and release cytokines that help them differentiate. In order for these T cells to bind to HLA II, they have a protein called CD4 that “confirms” and stabilizes the binding.
After differentiation, CD4+ T cells emerge from the follicle and assume their commander role. They release cytokines that attract other cells (basophils, eosinophils, mast cells, etc.) to the site of infection and activate macrophages.
Meanwhile, naïve B cells (B lymphocytes) wait in the follicle for the antigen to arrive so they can take part in the fight against the pathogen.
They act through surface receptor molecules - B-cell receptors. B cell receptors are created through highly variable gene rearrangements. The naïve B cell waits for its BCR to bind to the antigen. It takes up and presents the antigen on its HLA II, and waits to meet a CD4+ T cell that has already been activated to the same antigen. The beauty of B-cell receptors (BCRs) is that random gene rearrangement produces such a wide variety of B-cell surface receptors that virtually any foreign antigen that enters the body is recognized by them.
The T-lymphocyte helps the B-lymphocyte to proliferate and begin to produce antibodies, which will be able to bind antigens in the same way as B-cell receptors. Antibodies bind to antigens on the surface of bacteria, and the other end (Fc-end) binds to receptors on macrophages ( starfish in the picture above), after which they phagocytose the bacterium. In addition, antibodies on the surface of bacteria activate the complement system and also prevent bacteria from attaching to body cells.
In 90% of patients with type 1 diabetes, there is a special variant of HLA II (HLA-DQ8): it binds better to an antigen that carries a relative negative charge at certain positions (positions 1 and 9). Insulin is considered an autoantigen in type 1 diabetes, that is, it is recognized as a foreign agent by the immune cells of patients.
Typically, any protein is not presented in its entirety: cells show only its most immunogenic part. In insulin, this part is amino acids 9–23 on the B chain (B:9–23). However, presentation of B:9–23 by either normal or mutant (HLA-DQ8) HLA II to CD4+ T cells from T1DM patients does not lead to their activation.
It was recently discovered that the blood of people with T1DM, in comparison with a healthy sample, is enriched in chimeras of T and B cells ( X cells ) [3]. The antibodies of these cells have a charge order of amino acid residues similar to insulin. The antibody sites have a better affinity for insulin-specific T cells and activate them, inciting the development of an autoimmune response to the insulin-producing beta cells of the islets of Langerhans.
Unfortunately, it is currently unknown what the nature of the occurrence of T- and B-cell chimeras is. The involvement of X cells in the development of other diseases also remains a mystery.
The authors suggest screening more at-risk subjects and using X-cell clonal enrichment data as a prognostic indicator. Better RNA-seq analysis is also needed to determine whether X cells are a distinct new cell type or present in the body as a subpopulation of one of the already known cell types.
The number of people in whom this discovery was made is small, but if the results are confirmed, it will be an exciting step towards better understanding the autoimmune nature of type 1 diabetes. It will be interesting to see future results from these researchers.
Pancreas and hormones
One of the main functions (besides the fact that it takes an active role in digestion) is endocrine, that is, the production of very important hormones, the presence of which in the human body is simply necessary. The islets of Langerhans are those parts of the gland that are responsible for the production of hormones. Hormones produced by the pancreas include:
- Insulin. Almost everyone knows what role insulin plays in the human body and what consequences its deficiency can lead to. This hormone is involved in metabolic processes and also affects the absorption of amino acids, carbohydrates, and fats. In addition, thanks to insulin, all broken down substances are distributed throughout the blood, and each of these components becomes able to penetrate every cell in the body and perform its function. If there is a failure in the production of insulin, then the broken down nutrients will not be distributed throughout the body and will not reach the places where they are so needed. And this leads to intoxication of the body. One of the most common and well-known diseases that affects a person’s quality of life, and is caused by a lack or absence of insulin, is diabetes mellitus.
- Glucagon. The action of this hormone can be said to be that it is absolutely opposite to insulin, that is, the main function of glucagon is to activate all reserves of carbohydrates and convert them into energy, without which the body is not able to exist and function normally. Glucagon also maintains normal blood glucose levels even when a person is on strict diets and is not getting enough essential nutrients.
It should be noted that when the level of glucose in the blood increases, the work of insulin is activated and more of it is produced. If the blood glucose level decreases, then glucagon comes into play and its level increases.
The role of the pancreas in the production of hormones is simply undeniable, since everyone knows very well that with any failure the entire body immediately suffers.
And therefore, you need to carefully monitor the condition of the pancreas, eat properly and balanced to help it function as the human body requires.
Can type 1 diabetes be prevented?
More likely no than yes.
Autoimmune diseases are triggered at an unknown moment by an unknown combination of several “buttons”: for example, “stress + flu + milk”, “toxin + heredity + antibiotic”, “vaccine + vitamins + pregnancy” and other hypothetical options.
Having bypassed the protection, the “hacker” may not reveal himself, but hide for years and pass it on to posterity. Patients and their loved ones, looking back, rewinding events, thinking, delving into what happened, assume, guess about something, but their conclusions, like the hypotheses of researchers, are simply questioned.
However, there are known agents that, once ingested, will definitely destroy β-cells and cause T1D. For example, the drugs streptozocin, pentamidine, rat poisons pirinuron, pyriminil, vacor. Their danger has been proven, but production and use in some countries continues!
What are the islets of Langerhans?
The islets of Langerhans (OL) are polyhormonal microorgans consisting of endocrine cells located throughout the entire length of the pancreatic parenchyma, which performs exocrine functions. Their bulk is localized in the tail part. The size of the islets of Langerhans is 0.1-0.2 mm, their total number in the human pancreas ranges from 200 thousand to 1.8 million.
The cells form separate groups, between which capillary vessels pass. They are delimited from the glandular epithelium of the acini by connective tissue and nerve cell fibers running there. These elements of the nervous system and the cells of the islet form the neuroinsular complex.
The structural elements of the islets—hormones—perform intrasecretory functions: they regulate carbohydrate and lipid metabolism, digestive processes, and metabolism. The child's gland contains 6% of these hormonal formations of the total area of the organ. In an adult, this part of the pancreas is significantly reduced and accounts for 2% of the surface of the gland.
History of discovery
Clusters of cells, different in appearance and morphological structure from the main tissue of the gland and located in small groups mainly in the tail of the pancreas, were first discovered in 1869 by the German pathologist Paul Langerhans (1849-1888).
In 1881, the outstanding Russian scientist, pathophysiologist K.P. Ulezko-Stroganova (1858-1943) carried out fundamental physiological and histological work on the study of the pancreas. The results were published in the journal “Doctor”, 1883, No. 21 - article “On the structure of the pancreas under conditions of its rest and activity.” In it, for the first time at that time, she expressed a hypothesis about the endocrine function of individual pancreatic formations.
Based on her work in 1889-1892. in Germany, O. Minkovsky and D. Mehring found that when the pancreas is removed, diabetes mellitus develops, which can be eliminated by transplanting part of a healthy pancreas under the skin of the operated animal.
Domestic scientist L.V. Sobolev (1876-1921) was one of the first, based on research work, to show the importance of the islets discovered by Langerhans and named after him in the production of a substance related to the occurrence of diabetes mellitus.
Subsequently, thanks to a large number of studies conducted by physiologists in Russia and other countries, new scientific data on the endocrine function of the pancreas were discovered. In 1990, the first transplantation of islets of Langerhans into humans was performed.
Prevention: how to preserve the islet apparatus?
Since the function of the islets of Langerhans of the pancreas is to produce substances important for humans, lifestyle modification is necessary to maintain the health of this part of the pancreas. Key points:
- giving up alcohol and smoking,
- eliminating junk food
- physical activity,
- minimizing acute stress and neuropsychic overload.
Alcohol causes the greatest harm to the pancreas: it destroys pancreatic tissue and leads to pancreatic necrosis - the total death of all types of organ cells that cannot be restored.
Excessive consumption of fatty and fried foods leads to similar consequences, especially if this happens on an empty stomach and regularly. The load on the pancreas increases significantly, the number of enzymes that are necessary to digest large amounts of fat increases and depletes the organ. This leads to fibrosis and changes in the remaining cells of the gland.
Therefore, at the slightest sign of digestive dysfunction, it is recommended to consult a gastroenterologist or therapist in order to timely correct changes and early prevent complications.
Cell types
This diagram demonstrates the structural differences between the rat (top) and human (bottom) pancreatic islets: pars ventralis pancreas (abdominal part) - left; pars dorsalis pancreas (dorsal part) - on the right. Different types of cells are colored differently: alpha cells - red, beta cells - blue, delta cells - purple, PP cells - green, epsilon cells - yellow. Rodent beta cells, unlike humans, are grouped into a characteristic insulin core.
Alpha cells
Main article: Alpha cell
- Alpha cells make up 15...20% of the islet cell pool and secrete glucagon (a natural insulin antagonist).
Beta cells
Main article: Beta cell
- Beta cells make up 65...80% of the pool of islet cells - they secrete insulin (with the help of receptor proteins, they carry glucose into the cells of the body, activate the synthesis of glycogen in the liver and muscles, and inhibit gluconeogenesis).
Delta cells
Main article: Delta cell
- Delta cells make up 3...10% of the islet cell pool - they secrete somatostatin (inhibits the secretion of many glands);
PP cells
Main article: PP cage
- PP cells make up 3...5% of the pool of islet cells - they secrete pancreatic polypeptide (suppresses the secretion of the pancreas and stimulates the secretion of gastric juice).
Epsilon cells
Main article: Epsilon cell
- Epsilon cells make up <1% of the islet cell pool and secrete ghrelin (“hunger hormone” - stimulates appetite).