Crohn's disease
- inflammatory bowel disease, which belongs to the group of immune-mediated chronic diseases of the large intestine.
Inflammatory bowel diseases are one of the most complex pathologies in modern gastroenterology and coloproctology. The treatment of these diseases is based on an interdisciplinary approach, and its effect depends entirely on the mutual understanding and productive interaction of gastroenterologists and coloproctologists, who develop a treatment strategy during a multidisciplinary consultation.
Crohn's disease is a chronic immune-mediated granulomatous segmental inflammation of the gastrointestinal tract.
The disease is characterized by the development of inflammation of a segment of the intestine with the formation of strictures and intestinal fistulas as the pathology progresses.
Crohn's disease has a relapsing course.
The disease progresses mainly in the intestines, but all parts of the digestive tract (stomach, esophagus, tongue, oral cavity) can be involved in the process. Although in most cases the ileocecal region (the place where the small intestine enters the cecum) is affected.
In percentage terms, the disease most often affects:
- ileocecal region - about 40% of cases;
- ileum (terminal ileitis) – 30-35% of cases;
- large intestine, including the anorectal area – 20% of cases;
- small intestine – 5-10% of cases;
- upper parts of the digestive tract – 5% of cases.
Causes of the disease
The etiology of Crohn's disease has not been established. There is evidence linking the development of the disease with heredity. In close relatives, the pathology occurs 20 times more often than in the general population. A gene (NOD2 or CARD15) that is responsible for susceptibility to Crohn's disease has also been isolated. It suppresses the immune system's ability to respond to Mycobacterium paratuberculosis, which causes a disease similar to Crohn's disease in cattle.
Genetically determined defects in the barrier function of the intestinal mucosa also play an important role in the development of the disease. They facilitate the penetration of various bacterial antigens, triggering a chain of humoral and cellular reactions, which leads to transmural (piercing) inflammation of the intestinal wall with the formation of tissue changes characteristic of Crohn's disease.
Classification
Crohn's disease, like ulcerative colitis, has varied clinical manifestations. The classification of the European Society for the Study of Crohn's Disease and Ulcerative Colitis (ECCO) well reflects this diversity, highlighting possible variants of the course of the disease according to the localization of the inflammatory process, the form of the disease and the age of the patients (Table 3).
| Process localization | Form (phenotype) of the disease | Patient's age at diagnosis |
| L1 – terminal ileitis (with or without penetration into the cecum); L2 – colitis, without involvement of other parts of the digestive tract; L3 – ileocolitis (damage to the terminal section and colon); L4 – damage to the upper digestive tract (excluding the oral cavity), regardless of additional involvement of the small or large intestine. | B1 – luminal, without complications (may be combined with perianal manifestations (fistula or abscess); B2 – stenotic form; B3 – penetrating or fistulous (extraluminal) form. | A1 – 16 years or younger; A2 – 17-40 years old; A3 – over 40 years old. |
Table 3. European Society for the Study of Crohn's and Ulcerative Colitis (ECCO) classification of Crohn's disease.
It is also customary to distinguish between localized (less than 30 cm) and widespread (the sum of all affected areas more than 100 cm) Crohn's disease.
The course of Crohn's disease is characterized by two options:
- Acute course (less than 6 months from the onset of the disease). It can occur with a fulminant (quick) or gradual onset.
- Chronic relapsing course (presence of more than 6-month periods of remission). It can be either rarely recurrent (once a year or less) or frequently recurrent (2 or more times a year).
Intussusception
For a successful outcome, therapy should begin on the first day from the moment signs of intussusception appear. In the hospital, the child is given enemas, and surgical treatment methods are also available in some cases. Treatment methods may be different, depending on the situation, age of the patient, etc.
Air, saline, and barium enemas are effective for treating intussusception. An enema increases the pressure in the baby's intestines, so the intussusception straightens. This procedure is also called reduction. When using enemas to monitor the condition of the intestine, x-rays or ultrasound diagnostics are necessary.
An enema is effective in 75 cases out of 100. There is evidence that an enema with air is more effective than with barium or saline. ). The success of the procedure also depends on the duration of symptoms: the longer signs of intussusception are present, the less likely it is that the enema will be successful.
Bowel perforations occur in 25 out of 1000 cases of liquid enema use. With air enemas, the ratio of the number of perforations to the number of attempts to deliver an enema is 2 to 1000. This procedure is sometimes used again. But repetition more than 3 times is not recommended. This method of treatment is not used if there are signs of inflammatory processes in the abdominal wall, with sepsis (generalized infection), perforation, or gangrene of the intestine.
Surgery
Indications for surgical treatment of intussusception:
- the doctor suspected damage to the intestinal wall - in such cases, surgical treatment should be emergency
- the enema did not help even on the 3rd try
- the intestine has burst, feces penetrate into the abdominal cavity
Stages of surgery to treat intussusception:
- A skin incision is made on the anterior abdominal wall.
- The involved area of intestine is gently stretched to restore the normal shape of the intestine.
- The doctor removes the damaged areas.
- The appendix is also removed, even if it is healthy.
- The required number of stitches is placed on the wound.
If a large amount of intestine is removed or a severe infection develops, an ileostomy must be performed for a certain period. This is an operation to connect the lumen of the small intestine through the abdominal wall with a colostomy bag. Without treatment, intestinal obstruction occurs, and rupture of the intestinal wall is likely, which results in generalization of the infection, which in most cases entails death.
Intussusception can recur, which happens in some cases. If treatment with enemas was carried out, in 10 cases out of 100 a relapse is possible. Then the enema is repeated or surgery is performed. When surgical treatment is used, relapse is recorded in 2-5% of cases. Then the operation is repeated to straighten the intestine and find the causes of the disease. Sometimes the part of the intestine where the pathology occurs is removed.
What to do after surgery
After surgery, you should be careful for about 2-3 weeks to notice possible complications in the child:
- nausea and vomiting
- diarrhea
- temperature increase
- restlessness and frequent crying
You should take care of the seam. Maintain hygiene in this area and check for signs of post-operative wound infection:
- tissue swelling
- pain
- increase in temperature in that area
- redness in and around the suture
Manifestations of the disease
Patients with Crohn's disease most often complain of abdominal pain, chronic diarrhea, and weight loss. They also experience fever, anemia and intestinal bleeding.
Abdominal pain is associated with involvement of the parietal peritoneum (the serous lining of the intestine) in the process. The cramping nature of the pain may indicate the formation of intestinal obstruction. The constant nature of the pain that occurs against the background of fever may indicate the formation of an abscess. In this case, upon examination, the patient has an asymmetric abdomen, caused by the presence of an infiltrate (most often between the cecum and the navel) or an interintestinal abscess.
As the damage progresses, diarrhea occurs. Watery discharge of a greenish or bright yellow color indicates steatorrhea and hologenic diarrhea, which occurs due to malabsorption of bile acids.
Intestinal bleeding can be hidden for a long time and occur against the background of the appearance of erosions. Heavy bleeding usually indicates the presence of deep slit-like ulcers.
In the absence of intestinal symptoms of the disease, general malaise, fever, changes in laboratory parameters (increased C-reactive protein, ESR, leukocytosis) for a long time serve as the reason for searching for the source of the inflammatory process. A high temperature in Crohn's disease may indicate the development of an abscess.
A progressive inflammatory process in the small intestine gradually leads to malabsorption: patients develop anemia and hypoproteinemia. Women experience amenorrhea, children experience slow growth and delayed sexual development.
About 25% of patients with Crohn's disease have extraintestinal manifestations (damage to the eyes, skin, joints, etc.). As the disease progresses, autoimmune lesions of other organs appear in most patients.
In some cases, autoimmune lesions of other organs (pyoderma, uveitis, arthritis, etc.) may occur before the appearance of intestinal symptoms. Endoscopic examination of the intestine helps to recognize Crohn's disease in these cases.
Crohn's disease - symptoms and treatment
The diagnosis is made based on the clinical picture, course of the disease and diagnostic methods: laboratory examination, endoscopy, histology and radiology.
Laboratory research
The initial laboratory examination, in addition to standard tests (general blood and urine tests), includes the determination of inflammatory markers. First of all, the level of C-reactive protein is assessed - an indicator of tissue damage during inflammation.
Fecal calprotectin and lactoferrin are tested to distinguish inflammation from functional complaints, as these proteins are markers of intestinal inflammation. Calprotectin can help differentiate inflammatory bowel disease from irritable bowel syndrome in most cases. However, these tests are not specific for Crohn's disease, so they are mainly used to monitor patients during and after treatment.
Albumin is a parameter characterizing the ratio of muscle and fat mass; its determination is especially important in the preoperative period, since low concentrations are associated with a higher risk of complications.
Endoscopy
To establish the diagnosis, ileocolonoscopy and multifocal biopsy are performed from the terminal ileum and each segment of the colon. During ileocolonoscopy, the doctor examines the rectum, sigmoid and colon, which form the large intestine, as well as the ileum.
Endoscopy is also used to exclude damage to the upper gastrointestinal tract and in the postoperative period [2].
Radiation research methods
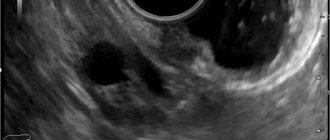
Ultrasound examination is indicated for acute conditions, as well as for identifying fistulas, stenoses, abscesses and for monitoring intestinal inflammation during treatment.
A plain radiograph is used in emergency situations, such as intestinal obstruction and perforation.
Magnetic resonance imaging (MRI) and CT enterography (computed tomography) for Crohn's disease accurately detect intestinal lesions and complications such as fistulas and abscesses. MRI and CT are performed during the initial examination if there is a high suspicion of Crohn's disease.
MRI is not exposed to radiation, so it is preferable to CT.
Computed tomography is used in cases where surgical intervention is planned, such as drainage of an abscess [9].
In rare situations when standard imaging methods are uninformative, capsule endoscopy is used to clarify.
Double-balloon enteroscopy is indicated only when a biopsy is required (eg, to exclude malignancy) or during therapeutic procedures, such as dilation of a stenosis.
MRI is the main method for perianal lesions. An alternative to MRI is endosonography, but it is used less frequently due to anal stenosis, which limits access, and pain, especially with severe perianal lesions.
Differential diagnosis
The main diagnoses with which it is necessary to distinguish Crohn's disease are: irritable bowel syndrome, ulcerative and infectious colitis.
For acute pain in the lower abdomen, the most important differential diagnoses are acute appendicitis and the infectious disease yersiniosis (pseudotuberculosis).
Granulomatous chronic intestinal inflammation can be caused by the systemic inflammatory disease sarcoidosis or tuberculosis. Malignant lymphomas and small bowel cancer sometimes lead to the development of small bowel stenosis and the formation of conglomerates of intestinal loops - these diagnoses should also be differentiated from Crohn's disease.
Treatment
Crohn's disease requires complex treatment, which includes drug therapy, surgical treatment if complications develop, and a special diet. Drug treatment is the mainstay of therapy and is aimed at reducing autoimmune inflammation and fighting infection. The following anti-inflammatory drugs are used: glucocorticosteroids, immunosuppressants, monoclonal antibodies to TNF-alpha, mesenchymal stem cells. To combat infection, broad-spectrum antibacterial drugs, antiviral and antifungal agents are used.
Surgical methods of treatment
Approximately 30% of patients with terminal ileitis have intestinal obstruction due to the formation of an ileal stricture. Fibrous strictures of the ileum up to 6 cm in length, located at a distance of up to 10-15 cm from the ileocecal valve, can be awakened endoscopically; an alternative option may be resection of the strictured section of the small intestine with the formation of an interintestinal anastomosis. In case of extended strictures (more than 20 cm) or multiple strictures, preference should be given to various options for surgical plastic surgery of the small intestine (expansion surgery without resection of a section of the small intestine). Resection of the intestine should be performed sparingly with a minimum distance of 2 cm from the fibrous wall.
The formation of anastomoses (one or two) during the operation does not increase the incidence of postoperative complications and relapse of the disease, and side-to-side hardware anastomosis reduces the risk of subsequent development of stricture.
It is possible to perform surgery using the laparoscopic method.
In 23-48% of cases, actively occurring terminal ileitis often leads to the development of complications in the form of infiltration or abscess of the abdominal cavity with the formation of intestinal fistulas (external or internal). Laparoscopic intervention for this type of complication can be difficult.
In this case, the patient is drained of the abscess, if necessary, the affected part of the intestine is removed and antibacterial drugs are prescribed.
Drainage of an abscess is carried out either surgically with removal of the affected area of the intestine, or, in the absence of a stricture, in specialized centers and in the presence of qualified specialists - by percutaneous drainage.
method of treating primary insufficiency of the bauhinium valve
Class A61K31/495 containing six-membered rings with only two nitrogen atoms as heteroatoms, e.g. piperazine
| 2, 5-disubstituted arylsulfonamide CCr3 antagonists - patent 2527165 (08/27/2014) | |
| substituted aminoindanes and their analogues, and their use in pharmaceuticals - patent 2522586 (07/20/2014) | |
| use of amine derivatives of fullerenes C60 and C70 and compositions based on them as antimicrobial agents - patent 2522012 (07/10/2014) | |
| low molecular weight inhibitors of n-terminal activation of the androgen receptor - patent 2519948 (06/20/2014) | |
| method for predicting the course of myocardial infarction based on assessing the severity of mitochondrial dysfunction - patent 2519700 (06/20/2014) | |
| agents that bind to amyloids - patent 2517174 (05/27/2014) | |
| a method for optimizing the intellectual activity of students - patent 2516117 (05.20.2014) | |
| new compounds of reverse action mimetics, method of their preparation and use - patent 2515983 (05/20/2014) | |
| phenylalkylpiperazines modulating tnf activity - patent 2512567 (04/10/2014) | |
| pharmaceutical composition for relief of the primary reaction to radiation and early transient disability - patent 2509557 (03/20/2014) | |
Class A61P1/00 Medicines for the treatment of disorders of the digestive tract or digestive system
| hepatoprotective agent from seaweed - patent 2528898 (09/20/2014) | |
| method for producing a drug for the prevention of digestive tract infections in poultry and the drug obtained by the method - patent 2528747 (09.20.2014) | |
| use of peptide actg (4-7)-pgp for hepatoprotective effects - patent 2528741 (09/20/2014) | |
| method of treating patients with dyspepsia syndrome in combination with excess body weight - patent 2528641 (09/20/2014) | |
| a new pyrazole-3-carboxamide derivative with antagonistic activity towards the 5-nt2b receptor - patent 2528406 (09/20/2014) | |
| pharmaceutical and/or food compositions based on short-chain fatty acids - patent 2528106 (09/10/2014) | |
| new thyroid hormone receptor beta agonist - patent 2527948 (09/10/2014) | |
| method of managing pregnancy in overweight women - patent 2527910 (09/10/2014) | |
| method for treating fatty hepatosis in cats - patent 2527700 (10.09.2014) | |
| toothpaste containing a buffer mixture - patent 2527691 (09/10/2014) | |