What is Creon?
Creon is a medicine that contains digestive enzymes produced by the pancreas of pigs and is designed to digest fats, proteins and carbohydrates. This remedy improves digestion processes, thereby reducing symptoms of pancreatic enzyme deficiency, as well as abdominal pain, flatulence, changes in stool and other uncomfortable conditions.
Creon is used as a replacement therapy for digestive enzymes when the body lacks its own. Creon is also used for insufficiency of pancreatic secretion, which is caused by a decrease in the activity of pancreatic enzymes.
The above conditions are caused by the following factors and pathologies:
- disruption of production and regulation of secretion;
- increased destruction of enzymes in the intestines;
- disruption of the delivery of pancreatic enzymes;
- cystic fibrosis;
- pancreatitis;
- postoperative period;
- consequences after removal of the stomach or part of it;
- pancreatic oncology;
- resection of the stomach (removal of part of it);
- blockage of the bile ducts or pancreas (as a result of neoplasms).
Pharmacological properties of the drug Creon
Creon contains pancreatin of porcine origin in the form of enteric-coated (stable in acidic environment) minimicrospheres in gelatin capsules. The capsules dissolve quickly in the stomach, releasing hundreds of mini-microspheres in a multi-dose manner, which ensures good mixing with the stomach contents, transport from the stomach along with its contents and, after release, good distribution of enzymes within the intestinal contents. When the minimicrospheres enter the small intestine, the shell quickly dissolves (at pH 5.5), releasing enzymes with lipolytic, amylolytic and proteolytic activity, which ensures the breakdown of fats, carbohydrates and proteins. The products of pancreatic digestion are then absorbed either immediately or after further hydrolysis by intestinal enzymes. In animal studies, there was no evidence of enzyme absorption in unchanged form, and therefore classical pharmacokinetic studies were not performed. Pancreatic enzyme supplements do not require absorption to be effective. On the contrary, their full therapeutic effect is manifested in the lumen of the gastrointestinal tract. Moreover, as substances of protein origin, they undergo proteolytic cleavage while passing through the gastrointestinal tract before being absorbed in the form of peptides and amino acids. Data from preclinical studies do not indicate acute, subchronic or chronic toxicity.
What do you need to know before you start taking Creon?
Do not take Creon if you have an allergy to animal proteins, exacerbation of pancreatitis, or other diseases of the pancreas. Tell your doctor if you have underlying medical conditions (gout, asthma, or allergies).
Tell your healthcare provider if you are pregnant or breastfeeding. During pregnancy, Creon should be taken with caution. When breastfeeding, the use of Creon is contraindicated.
For children, the doctor calculates the dose based on body weight.
Creon 10000 – a drug for the little ones
Creon 10000 is an excellent remedy for young children.
Creon 10000 is an excellent medicine for young children. Recently, more and more children are suffering from various disorders of the digestive system. Newborns cannot tell where it hurts, but parents can notice that the child is unwell. Colic, flatulence, various gastrointestinal diseases are problems that are often observed even in very young children.
A variety of enzyme medications are used to treat children. Creon is one of these drugs and, since it has proven itself to be an effective remedy, is often used in the treatment of gastrointestinal disorders. 10,000 is the dosage of a drug that can be used in the treatment of children in the first years of their life.
We should not forget that the dosage of the drug should be prescribed by the attending physician on an individual basis. The general recommendation is to use 1000 units/kg of the drug per meal. In the case of very young children who do not yet eat solid food, the medicine capsules can be opened and added to the baby’s drink.
It is not recommended to damage the small spheres of the drug that are inside the capsule, as this may reduce or even completely neutralize its medicinal effect. Under no circumstances should the drug be used without prior consultation with a qualified specialist. Creon 10000 has some contraindications, which can be determined by a doctor individually.
Creon 10000 is a medicine used in the treatment of various gastrointestinal diseases in children. It can only be prescribed by a doctor, who also prescribes an individual dose for a specific baby.
How to take Creon correctly
Use Creon exactly as indicated in the instructions, as well as based on the prescription of a specialist. Do not take Creon in doses not listed in the instructions. Do not exceed the permissible duration of use.
Creon should be taken with meals with a glass of water, without crushing or chewing, swallow whole.
Do not put the tablet in your mouth as this medication may irritate your mouth.
To be sure of the action of Creon, you can take blood tests, as you may not notice any changes in your well-being. Tell your doctor if your symptoms do not improve or get worse while using Creon.
Creon may not be the main treatment program. You should follow a diet created based on your indications.
Use Creon regularly, without skipping a dose, to achieve maximum effect.
Use of Creon in children with impaired motility of the upper gastrointestinal tract
Introduction
. In recent decades, the most common pathology in pediatric gastroenterological practice is gastrointestinal motility disorders. The causes of these disorders in children are the immaturity of neuromuscular structures and peculiarities of autonomic regulation. This is further aggravated by the unfavorable environmental conditions in which children find themselves, as well as the enormous psycho-emotional stress endured by children in educational institutions.
Normal gastrointestinal motility is ensured by the coordinated work of the muscular layer of the intestine and sphincters, during which food is crushed, mixed with digestive juices and moved in the distal direction. The propulsive activity of the intestine and the state of the sphincters are regulated by the autonomic nervous system, intramural nerve plexuses, as well as hormones of the gastrointestinal tract itself and peptides of endocrine cells. The muscles of the stomach and small intestine, as well as the muscles of the myocardium, contain pacemakers. However, unlike cardiac muscle, not every wave of depolarization leads to muscle contraction. Only when the action potential is superimposed on the plateau of the depolarization wave does muscle contraction of the intestinal muscles occur. The effect of neuropeptides and mediators on the tone of the intestinal muscles has not been fully studied. However, it is known that gastric motility is enhanced by hormones such as cholecystokinin and especially gastrin, and is suppressed by secretin, glucagon, VIP and somatostatin [1].
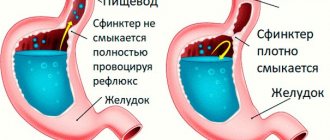
Under normal conditions, intestinal chyme moves unidirectionally in a distal direction. Disruption of the nervous regulation of the gastrointestinal tract, as well as disorders of humoral factors arising, for example, as a result of inflammatory changes in the organ, leads to disruption of the correct coordinated functioning of the muscular layer of the intestinal tube and sphincters. In this case, hyper- or hypotension of the intestinal tube, spasm or gaping of the sphincters develops. Motor abnormalities such as slow content movement, faster content movement, or retrograde content movement occur. Retrograde movement of chyme - reflux occurs when sphincter tone decreases and there is a negative pressure gradient between two adjacent sections of the gastrointestinal tract and/or retroperistalsis.
Currently, in clinical practice, a gastroenterologist is most often faced with the problem of gastroesophageal and duodenogastric reflux. Gastroesophageal reflux (GER) is observed in a number of birds and mammals as an adaptive mechanism of digestion. [5] In healthy people, a small number of GERs are observed: they are not important for digestion and are rather vestigial in nature. GER occurs mainly after eating, their duration does not exceed 5 minutes, and when performing pH-metry, the total decrease in pH in the esophagus to 4.0 units. and below should not exceed 4.5% of the total recording time [5]. Physiological reflux never leads to organic damage to the esophageal mucosa.
The causes of pathological GER are decreased tone of the lower esophageal sphincter, hiatal hernia, and impaired gastric motility. GER is often combined with duodenogastric reflux (DGR). Duodenogastric reflux occurs when the pylorus is gaping, impaired motility of the duodenum, lack of coordination in the work of the pylorus and duodenum, as well as duodenal hypertension. If bile from the duodenum enters the stomach in large quantities, it can be thrown further into the esophagus. These are the so-called DGRs. In this case, the development of deeper damage to the mucous membrane of the esophagus is possible due to the damaging effect of bile acids found in the refluxate [2].
A slowdown in the movement of intestinal contents in the distal direction may be associated with a decrease in propulsive activity and/or an increase in the tone of the corresponding sphincters, and an acceleration may be associated with an increase in propulsive activity and/or sphincteric hypotension. In such situations, it is important to correctly determine the cause of the disorders that have arisen and prescribe appropriate therapy.
The range of diseases accompanied by impaired motility of the gastrointestinal tract is wide. In childhood, according to our data, combined disorders of motility of various parts of the gastrointestinal tract are more common. For example, impaired gastric motility is combined with impaired motility of the biliary tract and large intestine, and gastroesophageal reflux disease in children is often combined with functional dyspepsia or irritable bowel syndrome.
Gastrointestinal motility disorders in children are mainly functional in nature and are associated with impaired autonomic regulation of the organ [2]. Slow and insufficient maturation of the nervous system is a consequence of an unfavorable pregnancy, as well as damage to the cervical spine due to improper management of childbirth or improper massage during the 1st year of life. Pathology of the cerebral cortex and hypothalamus as a result of birth trauma also leads to a disorder of autonomic regulation [2]. In some cases, functional motor disorders resolve on their own with the maturation of neural connections and humoral regulation. An example of such disorders may be functional disorders of the newborn period: infantile intestinal colic and regurgitation. In such cases, it is advisable to carry out only symptomatic therapy aimed at alleviating symptoms. However, the long-term existence of motor disorders can lead to the development of organic disease. For example, long-term GER leads to the development of reflux esophagitis, and long-term GER leads to reflux gastritis. According to our observations, in some cases, functional disorders of gastrointestinal motility in early childhood, such as infantile intestinal colic, are transformed in older age into functional abdominal pain and/or irritable bowel syndrome [5]. This, as a rule, is facilitated by poor nutrition, previous intestinal infections, psycho-emotional stress and concomitant organic diseases. In such a situation, it is legitimate to say that in these patients the digestive tract is a “Locus minoris”. The parents of these children need to be explained that adherence to diet, nutrition, as well as increased precautions against contracting intestinal infections plays a vital role in preventing the development of intestinal pathology.
Purpose of the study
. The purpose of this study was to search for optimal approaches to therapy, taking into account new research methods that make it possible to more accurately determine the type of motor disorders of the upper gastrointestinal tract.
Materials and methods
. In our clinic, 30 people were under observation with complaints of heartburn, belching, and abdominal pain. For all these patients, in addition to standard examination methods (general blood and urine tests, biochemical blood test, ultrasound of the abdominal organs, FEGDS with biopsy, pH-metry), additional studies were carried out such as electrogastrography and gastroduodenoscintigraphy. Electrogastrography is a non-invasive method based on recording the electrical potential from the gastrointestinal tract. It allows you to assess the electrical activity of the stomach and intestines, which correlates with the motor-evacuation function of these parts of the gastrointestinal tract.
Research results
.
When conducting gastroscopy and morphological studies of biopsy samples of the fundic and antral parts of the stomach, organic pathology was not detected in any case. When conducting 24-hour pH-metry, pathological GER was detected in 15 people (more than 50 per day), while the total duration of time with a pH in the esophagus of less than 4 was more than 1 hour. Based on research data, complaints and anamnesis, gastroesophageal reflux disease without esophagitis and functional dyspepsia were diagnosed. When performing gastroduodenoscintigraphy, a violation of the evacuation function of the stomach was revealed in all patients, and in 21 (70%) gastroesophageal and duodenogastric refluxes were detected. All these patients also underwent electrogastrography. In this case, two types
of violations were identified.
The first type was characterized by a violation of the evacuation of food from the stomach against the background of normal or reduced electrical activity of the duodenum
, the so-called
“lazy stomach”
.
In the second case,
there was
a slowdown in the evacuation of food from the stomach against the background of increased electrical activity of the duodenum
, which indicates its
increased tone
.
For the first type of disorders, we used prokinetics (domperidone) in therapy; for the second type of disorders, accompanied by duodenal hypertension, antispasmodics (Duspatalin) were used.
14 patients were additionally prescribed enzyme therapy (Creon)
. The rationale for prescribing enzyme therapy was the assumption that the action of enzymes will speed up the process of digesting food and will help reduce pressure in the duodenum, which, in turn, will lead to faster evacuation from the stomach. The use of the microspherical drug "Creon" is optimal in such patients. Minimicrospheres are quickly mixed with chyme. The absence of bile components in Creon determines its advantage over other enzymatic preparations, since DGR is often observed in patients with impaired motility of the stomach and duodenum. Bile components in enzyme preparations can enhance GDR and contribute to the damaging effect of bile acids on the mucous membrane of the stomach and esophagus.
"Creon" was prescribed in an average daily dose of 10,000 units Ph Eur/10 kg body weight. The drug was taken with meals. In patients receiving Creon, the symptoms of dyspepsia were relieved earlier - compared to the group who received only antispasmodics or prokinetics as therapy, on average by 3-4 days. This significantly increased the effectiveness of therapy and reduced the time of treatment in the hospital.
Discussion
. Thus, for patients with impaired motor-evacuation activity of the stomach, it is advisable to add enzyme preparations to the therapy. The microspherical enzyme preparation "Creon", improving digestion, due to a decrease in intraluminal pressure in the duodenum, promotes faster gastric emptying.
In conclusion, I would like to note once again that etiopathogenetic therapy for functional disorders of the gastrointestinal tract has not yet been fully developed, which would eliminate the cause of the pathological process and lead to a complete cure of the patient.
Currently used therapy is symptomatic. Literature:
1. Human physiology. In 3 volumes. T.3. Translated from English/Ed. R. Schmidt and G. Tevs. – M.: Mir, 1996.–198 pp., ill.
2. Functional diseases of the digestive system in children. A.V. Kapustin, A.I. Khavkin., Yu.A. Izachik. Institute of Pediatrics. Moscow, 1994
3. Clinical gastroenterology. P.Ya. Grigoriev, A.V. Yakovenko. – M., Medical Information Agency, 1998.–647 p.
4. Functional disorders of the upper digestive system in children. S.V. Bellmer, T.V. Gasilina. Russian pediatric journal. №5, 2001
5. Gastroenterology of childhood. Edited by S.V. Belmera and A.I. Khavkina - M.: Publishing House Medpraktika-M, 2003, 360 p.
Method of use and dosage of Creon
Use of Creon for cystic fibrosis.
Dosage method for Creon for children:
At the initial stage of treatment, the dosage regimen is calculated depending on body weight in children under 4 years of age - 1000 units of lipase per 1 kg with the main meal. Children from 4 years old - 500 units of lipase per 1 kg of weight during meals.
Dosing method for Creon in adults:
The maintenance dose is no more than 10,000 units of lipase per 1 kg of body weight per day or 4,000 units of lipase per 1 kg of fat consumed with food.
Other types of endocrine insufficiency.
Specific dosage calculation based on pancreatic disorders. In adults, the dose is calculated to be 25,000-80,000 units of lipase with meals or 0.5 of the dose with a snack.
To improve digestion with normal gastrointestinal function.
The dose is 10,000-20,000 units of lipase per dose.
Indications for use of the drug Creon
Insufficiency of exocrine pancreatic function in adults and children caused by the following conditions:
- cystic fibrosis,
- chronic pancreatitis,
- pancreatectomy,
- gastrectomy,
- pancreas cancer,
- operations involving gastrointestinal anastomosis (for example gastric resection according to Billroth II),
- obstruction of the pancreatic or common bile duct (for example by a tumor),
- Shwachman-Diamond syndrome and other diseases accompanied by exocrine pancreatic insufficiency.