Ascites is a pathological condition in which fluid accumulates in the abdominal cavity. The reasons for it are different. The most common cause of ascites is cirrhosis of the liver. It also occurs as a complication of oncological diseases, while the patient’s condition worsens and the effectiveness of treatment decreases.
- What types of cancer can cause ascites?
- Why does cancer cause fluid to accumulate in the abdomen?
- Manifestations of ascites in cancer
- What complications does ascites lead to?
- Diagnostic methods
- Treatment of ascites in oncology
- Prognosis for ascites in cancer patients
- Prices
Some numbers and facts:
- In the early stages of cancer, moderate ascites develops in approximately 15–50% of patients;
- Severe ascites develops in approximately 7–15% of cancer patients;
- With ascites, up to 5-10 liters of fluid can accumulate in the abdominal cavity, in severe cases - up to 20 liters.
Why does cancer cause fluid to accumulate in the abdomen?
In liver cancer, the causes of ascites are the same as in cirrhosis (in fact, liver cancer in most cases develops against the background of cirrhosis): impaired blood outflow, increased pressure and congestion in the veins, impaired albumin synthesis and a decrease in oncotic pressure of the blood.
In case of malignant tumors of other organs (stomach, intestines, uterus, ovaries), ascites occurs due to damage to peritoneal cancer cells. Because of this, fluid absorption is impaired. If tumor cells invade the lymph nodes, ascites may occur due to impaired lymph flow.
Epidemiology
According to statistics collected by foreign gastroenterologists, approximately 28% of patients face the problem of insufficient stomach acidity. It is important to note that it manifests itself in middle age - by the age of 40. Moreover, the older a person gets, the higher the risk of problems with acidity levels. By the age of 50, the problem is observed in 40-45% of patients, by 70 – in 75%.
Causes
Low acidity can be caused by several reasons, the main one being a reduction in the amount of hydrochloric acid produced; this function is performed by glands located in the mucous membrane of the fundus of the stomach.
A decrease in the secretion of hydrochloric acid can be due to the following factors:
- Ingestion of Helicobacter Pylori bacteria into the stomach (they create conditions conducive to the neutralization of stomach acid);
- Reduction of the gastric mucosa;
- Slow metabolism caused by problems with thyroid function;
- A change in the acid-base balance in the stomach manifests itself against the background of diseases accompanied by the loss of chlorine ions due to vomiting or diarrhea;
- Stomach cancer or radiation therapy that affects the functioning of the organ;
- Pancreatic islet cell tumors;
- Pituitary adenoma, leading to increased production of a hormone that regulates the endocrine system;
- Autoimmune gastritis is characterized by the death of mucosal cells, which affects all parts of the stomach;
- Zinc deficiency in the body;
- Low levels of thiamine and niacin.
Risk factors
Among the risk factors that increase the likelihood of decreased stomach acidity are:
- Poor nutrition or diets that limit food intake;
- Increased carbohydrate intake;
- Inflammatory processes in the intestines that have a negative effect on the production of hydrochloric acid;
- Unstable emotional state and depression on a regular basis;
- Gluten intolerance;
- Elderly age.
Also, neutralization of the effect of acids contained in gastric juice can be a consequence of taking soda and antacids for a long period of time. In addition, there are certain drugs and agents, the effects of which lead to a decrease in the production of hydrochloric acid.
Manifestations of ascites in cancer
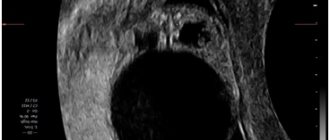
If a small amount of fluid accumulates in the abdominal cavity (100–400 ml), there are no symptoms. In such cases, ascites is often discovered accidentally during an ultrasound or CT scan of the abdominal organs.
Gradually, as ascites increases, the abdomen increases in volume. The patient feels heaviness in the abdomen, aching pain. Due to fluid retention, body weight increases. Compression of the internal organs occurs, and symptoms of abdominal ascites such as nausea and vomiting, belching, upset bowel movements and urination occur. The appearance of the navel changes: it bulges, as during pregnancy. The patient feels weak, constantly tired, and his appetite decreases.
What complications does ascites lead to?
With severe, long-term ascites, fluid accumulates in the pleural cavity, and hydrothorax develops. This leads to even greater respiratory distress and severe shortness of breath.
*By analogy with the abdominal cavity, in the chest there is a thin membrane of connective tissue - the pleura, the parietal layer of which lines the walls, the visceral layer covers the lungs.
With portal hypertension, microorganisms from the intestine can penetrate the ascitic fluid. Spontaneous bacterial peritonitis develops. The situation is aggravated by the fact that there are few antibodies in the ascitic fluid, so the immune response is weak.
A rare but very serious complication of ascites is hepatorenal syndrome. In this case, cirrhosis and liver failure lead to serious impairment of kidney function, up to severe renal failure. Patients with hepatorenal syndrome live on average from 2 weeks to 3 months. The causes of this condition are not fully known. It is believed that blood flow in the kidneys is impaired due to excessive use of diuretics, intravenous contrast during radiography and computed tomography, and certain medications.
Can hydrocephalus be cured?
Modern methods make it possible to normalize the outflow of cerebrospinal fluid from a congested brain or spinal cord by installing shunts - tubes that drain cerebrospinal fluid. Sometimes, with a mild form of the disease, this is enough to preserve the child’s intelligence. However, such a child will have to be home schooled, because... a minor head injury, which he easily receives at school, can be fatal. Such children also do not attend preschool institutions.
But in severe forms of the disease, manifested by a significant increase in head size, especially when combined with other developmental defects, the child’s physical and mental development inevitably suffers.
The growth of the head progresses after birth and it becomes very large with protruding external saphenous veins. Such children often have profound disabilities and cannot even care for themselves.
The most dangerous situation is when, already in utero, the child receives severe brain damage caused by increased intracerebral division. Children often suffer from visual impairment, hearing impairment, cerebral palsy, convulsive seizures, epilepsy, and attacks of uncontrollable headaches accompanied by vomiting. Most children, except those suffering from a mild form of hydrocephalus and receiving timely treatment, die before the age of 10 years.
Of course, the question of whether or not to leave a child with hydrocephalus depends on the degree of manifestation of the pathology, so the doctor, during an ultrasound of the fetus, will tell you what problems may arise and whether there is a chance for treatment and rehabilitation.
In the future, everything depends on the principles and financial capabilities of the family, because the treatment and recovery of such a child is expensive and not always promising. If the doctor insists on terminating the pregnancy, it is better to agree with him.
It is not uncommon for the birth of such a child to destroy a family. As a result, by the age of 6-10, the sick child still died, but at the same time other children suffered, deprived of the care and attention of parents who were fully occupied with caring for a child with a high degree of disability.
Diagnostic methods
External signs of ascites become clearly visible when the amount of fluid in the abdominal cavity reaches 0.5–1 liter. The abdomen is noticeably enlarged. When the patient stands, he looks drooping; when lying down, he is spread out, with his sides protruding. Doctors call this picture figuratively “the belly of a frog.”
If during an examination the doctor detects signs of ascites in the patient, he may prescribe the following diagnostic methods:
- Ultrasound, CT and MRI help to diagnose ascites and assess the amount of fluid in the abdominal cavity, the condition of internal organs, detect a malignant tumor, assess the number, size, localization of pathological foci, the degree of tumor invasion into various organs and tissues;
- A biochemical blood test helps assess liver and kidney function, determine electrolyte levels, and the degree of protein reduction;
- A blood clotting test helps identify disorders associated with liver dysfunction (the liver synthesizes some clotting factors);
- Diagnostic laparocentesis is a procedure during which a puncture of the abdominal cavity is performed under ultrasound guidance and a small (about a tablespoon) amount of ascitic fluid is obtained. It examines the levels of leukocytes and erythrocytes, total protein and albumin, glucose, and amylase. Conduct tests for the presence of microorganisms, cytological examination for the presence of tumor cells.
How is the procedure done?
The examination is painless and does not imply any violation of the integrity of the skin. There are different methods for doing it.
Transabdominal research methods
The transabdominal ultrasound method is an ultrasound examination that is performed using a surface sensor.
The examination is carried out through all layers of the abdominal wall.
- The patient in the ultrasound room must expose the anterior abdominal wall.
- After this, the patient takes a comfortable position on the couch.
- A special gel is applied to the stomach.
- During the procedure, the doctor may ask you to turn on your side or stomach in order to examine the organs from a better projection.
- The doctor can show the patient the progress of the examination on the monitor.
- If preparation for a transabdominal ultrasound was carried out normally, the procedure lasts about half an hour.
This diagnostic method is the most common, since it is completely painless, and during the examination the sensor is not inserted into the body.
Endoscopic ultrasound
Endosonography is a combination of ultrasound examination of internal organs and endoscopy, which allows you to bring an ultrasound sensor directly to the organ being examined.
This method is used when the necessary data cannot be obtained by transabdominal ultrasound.
- The person lies on his left side and bends his knees slightly.
- The endoscope is carefully inserted through the oral cavity or through the nasal cavity into the lumen of the pharynx and esophagus, which allows the attending physician to examine nearby lungs and lymph nodes using an ultrasound probe.
- By moving the endoscope further into the stomach, the doctor can evaluate the condition of its walls, as well as the nearby spleen and pancreas.
- When the sensor is inserted into the duodenum, the patency and condition of the bile ducts and the head of the pancreas are assessed, where the tumor process is very often localized.
The study is performed using medicated sleep or while taking sedative medications. In particular, medicated sleep is necessary when performing a biopsy of suspicious formations or when performing a study through the colon.
The procedure can take from 20 minutes to 2 hours, depending on the purpose of the examination, as well as the need for additional biopsy or surgery.
Treatment of ascites in oncology
Treatment of ascites in cancer patients is a complex task. The quality and life expectancy of the patient and the effectiveness of antitumor therapy depend on the correct approach to solving it. Ideally, you need a clinic that specializes in the treatment of ascites in cancer patients.
Conservative treatment
This therapy helps remove up to 1 liter of fluid per day. It significantly improves the condition in approximately 65% of patients. But it can only be used for moderate ascites. Many patients with advanced cancer do not tolerate fluid and salt restriction well. Therefore, conservative therapy is not considered as the main method of treating ascites in oncology.
Laparocentesis
Laparocentesis is a procedure during which a trocar is inserted into the abdominal cavity under ultrasound guidance - a special instrument in the form of a tube with sharp edges (reminiscent of a needle, only thicker) and fluid is removed. Laparocentesis is performed under local anesthesia under sterile conditions, with the patient sitting or lying down during the procedure. The trocar is inserted along the midline of the abdomen or along the line that connects the umbilicus to the ilium. During the procedure, up to 5-6 liters of fluid can be safely removed from the abdominal cavity.
After laparocentesis, the doctor may insert a peritoneal catheter into the abdominal cavity - a tube connected to a reservoir to drain ascitic fluid. With severe ascites, the catheter can be left in place for several days.
Possible complications during and after laparocentesis:
- A drop in blood pressure when a large amount of fluid is removed. To prevent this from happening, the ascitic fluid is removed slowly, and the patient’s pulse and blood pressure are constantly monitored;
- Protein deficiency due to the loss of a large amount of albumin along with ascitic fluid. To combat protein deficiency, albumin is administered intravenously;
- Pain. If necessary, painkillers are prescribed after laparocentesis.
- Fluid that remains after the procedure in some parts of the abdominal cavity. To drain all the fluid, your doctor may place more than one peritoneal catheter in different locations.
- Peritonitis as a result of penetration of microorganisms into the abdominal cavity. A rare complication. For its prevention and treatment, antibacterial drugs are prescribed, and surgical intervention may be required.
- Impaired fluid outflow through the peritoneal catheter. Most often it occurs due to the fact that the end of the catheter is “sucked” to the wall of the abdominal cavity or internal organs. Often, to cope with this problem, it is enough to change the position of the body. If this does not help, the catheter may need to be replaced.
- Fluid discharge after catheter removal. To collect it, a special reservoir is placed at the puncture site for 1–2 days.
- Fusion of the omentum (part of the peritoneum) or part of the intestine with the abdominal wall occurs with repeated punctures. If this causes significant bowel disruption, surgical removal of the adhesions may be required.
Intraperitoneal chemotherapy
Some patients are prescribed intraperitoneal chemotherapy - the chemotherapy drug is injected in high doses into the abdominal cavity, sometimes preheated to 41 degrees (this chemotherapy is called hyperthermic). This helps reduce ascites. Systemic chemotherapy is administered.
One of the new drugs for the treatment of ascites in cancer patients is the monoclonal antibody Catumaxomab. It is also administered intraperitoneally. Catumaxomab interacts with receptors of tumor and immune cells and induces an immune response. But the drug only acts on cancer cells that have certain molecular genetic characteristics.
Surgery
Omentohepatophrenopexy is indicated for some patients. During this operation, the omentum is sutured to the liver or diaphragm. Due to the occurrence of such contact, the absorption of ascitic fluid improves.
Peritoneovenous shunting is used as a palliative surgical intervention. A catheter is installed in the abdominal cavity, which connects it to the venous system. The catheter is equipped with a valve - it opens when the pressure in the abdominal cavity exceeds the central venous pressure. In this case, fluid is discharged into the veins.
Deperitonization of the walls of the abdominal cavity is an intervention during which the surgeon removes sections of the peritoneum, thereby creating additional pathways for the outflow of ascitic fluid.
Other types of surgical treatment are also used.
Feeling of discomfort in the stomach
Unpleasant sensations manifest themselves individually, but there are common symptoms:
- nagging pain or burning in the upper abdomen;
- heaviness;
- feeling of quick satiety;
- nausea or vomiting;
- heartburn;
- flatulence or increased gas production;
- feeling of a full stomach.
The presence of even one of the symptoms indicates that not everything is in order with the digestive organs.
Discomfort in the stomach is a frequent companion to the modern rhythm of life and poor eating habits. The main negative factors include:
- Stress.
Constant rush, nerves and stressful situations lead to disruptions in the functioning of the gastrointestinal tract; - Tobacco.
Cigarettes have a negative effect on the mucous membrane of internal organs involved in the digestion process; - Alcohol.
With regular consumption of alcoholic beverages, you may encounter not only individual symptoms of stomach discomfort, but also serious diseases; - Violation of nutrition rules:
snacking “on the run”, eating low-quality foods, overeating, abuse of fast food, predominance of fatty and fried foods in the diet, violation of heat treatment rules, lack of a diet; - Lactose intolerance.
It is common to many, but is especially common in infants and older people. The fact is that with age, the body secretes less and less enzymes that are responsible for processing lactose (this is a disaccharide contained in milk). Due to the inability to break down sugar in the stomach, fermentation processes begin and gas is released in large quantities. Which is the main cause of discomfort.
Frequent consumption of too hot and strong coffee or tea, or highly carbonated drinks can also lead to stomach problems.
A common manifestation of discomfort is a feeling of a full stomach.