Pancreatitis is an acute or chronic inflammation of the enzymatic pancreas and peripancreatic tissues, manifested by low back pain and increased activity of pancreatic enzymes. About two-thirds of cases of acute pancreatitis (AP) are caused by long-term excessive alcohol consumption or gallstones.
The etiology of AP, recurrent and chronic pancreatitis (CP) is very diverse. Various combinations of genetic, epigenetic, metabolic and environmental factors can trigger the inflammatory process and lead to its effects in several systems that regulate and maintain pancreatic function.
When treating the patient and taking preventive measures, it is important to determine the etiological factors in order to prevent relapse of the disease. This article takes a closer look at the rarer causes of acute and chronic pancreatitis.
Epidemiology
The content of the article
According to recent studies, every 34 out of 100 thousand people develop pancreatitis every year, and due to the increasing prevalence of the main etiological risk factors - obesity, alcoholism, smoking, stone formation, the disease is diagnosed in younger people. Also, such statistics are associated with improved diagnosis and identification of less common causes of pancreatitis.
An independent risk factor for AP is smoking. This habit worsens alcohol-related damage to the pancreas.
Risk factor for pancreatitis is smoking
Most patients have mild pancreatitis; in 20-30% of cases, severe pancreatitis occurs. The mortality rate from severe pancreatitis is about 15%.
Diagnostics
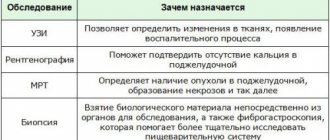
Due to the bright and pronounced symptoms, acute pancreatitis is easy to diagnose. Treatment is always prescribed individually, taking into account the form of the disease and the patient’s condition. To exclude complications, it is important to conduct laboratory and instrumental examinations in a timely manner. This will provide all the necessary data to assess the condition of the pancreas.
In acute pancreatitis, the following is always carried out:
- A general blood and urine test, the indicators of which will allow you to assess the general condition of the patient.
- Multislice computed tomography, which can be used to determine the severity of the disease.
- Ultrasound of the abdominal organs to assess the condition of organs located near the pancreas
In order to accurately select treatment methods, biochemical tests of urine and blood are prescribed. Also, if necessary, the list of instrumental studies can be expanded to detect neoplasms, abscesses, etc.
Etiology
The etiological factors of pancreatitis are very diverse - metabolic, mechanical, infectious, vascular. Often the disease occurs as a result of the interaction of several factors. The etiology of AP is determined only in 75% of patients.
Chronic pancreatitis is classified according to etiology and risk factors according to the TIGAR-O classification (Table 1).
Table 1. Etiological classification of chronic pancreatitis (TIGAR-O)
| Toxic-metabolic |
| Alcohol; Tobacco, smoking; Hypercalcemia (hyperparathyroidism); Hyperlipidemia; Chronic renal failure; Drugs and toxins. |
| Idiopathic |
| Early start; Late start; Tropical calcific pancreatitis, fibrocalcular pancreatic diabetes. |
| Genetic |
Autosomal dominant
|
| Autoimmune |
| Autoimmune pancreatitis type 1 (IgG4 positive); Autoimmune pancreatitis type 2 (negative IgG4). |
| Recurrent (reversible) and acute |
| Ponecrotic (acute); Reversible sharp:
Ischemic (postoperative, hypotensive); Infectious (viral); Chronic alcoholism; Poradiative; Diabetes. |
| Obstructive |
Benign pancreatic duct stricture:
Malignant stricture; Periampullary carcinoma; Pancreatic adenocarcinoma. |
Table 2. Rare causes of pancreatitis
| Nosology | Characteristics | Diagnostics |
| Metabolic pancreatitis | Hypertriglyceridemia and hypercalcemia | OP or HP |
| Drug-induced pancreatitis | Azathioprine, 6-mercaptopurine, sulfonamides, estrogens, tetracycline, valproic acid, antiretroviral drugs | OP or HP |
| Autoimmune pancreatitis | Focal or diffuse enlargement of the pancreas, hypotensive pancreatic shunt, expansion of the papillary part due to lymphoplasmocytes p.
| HP |
| Hereditary pancreatitis | Usually occurs at a young age, gene mutations are detected | Acute recurrent pancreatitis |
| Pancreatitis after the procedure | Endoscopic retrograde cholangiopancreatography was recently performed | Most often OP |
| Pancreatitis with sedimentation of bile (sediment) | Bile deposits and small stones (microlithiasis) | Most often OP |
| Pancreatitis Paraduodeninio groove ( groove ) | Fibrous formations between the head of the pancreas and the thickened wall of the duodenum, leading to duodenal stenosis, cystic changes in the pancreaticoduodenal groove or duodenal wall, pancreatic and bile duct stenosis | Exclusively HP |
| Duodenal diverticulum | Periampullary diverticulum, wind deformation | OP>HP |
| Traumatic pancreatitis | Direct trauma to the pancreas, intrapancreatic hematoma, rupture of the pancreas with fluid around it | OP or HP |
| Infectious pancreatitis | Various infectious factors: viruses, bacteria, fungi. | Most often in OP |
| Ischemic pancreatitis | Pancreatitis due to circulatory disorders, arterial hypotension, cardiogenic shock | OP or HP |
Death from acute inflammation: how to prevent tragedy?
Acute pancreatitis develops most often due to alcohol abuse and fatty foods. It is very difficult and often leads to life-threatening complications.
Mortality statistics from acute pancreatitis state that 20% of patients with this diagnosis may die, especially in the absence of proper timely therapy.
In order to avoid tragedy, it is necessary to make a timely correct diagnosis and choose the right treatment tactics: surgical intervention according to indications or conservative treatment in the intensive care unit.
Early diagnosis
If a person is diagnosed with chronic pancreatitis, he is familiar with the symptoms of exacerbation and the need for urgent hospitalization in a hospital. With the development of acute pancreatitis, the condition can be underestimated. The slightest delay in medical care can lead to irreparable consequences (disability or death of the patient). Therefore, if you develop any digestive problems, acute abdominal pain, especially against the background of fever, or a deterioration in your general condition, you must consult a specialist or call an ambulance.
To establish a diagnosis, a doctor (gastroenterologist, therapist or surgeon) will conduct a survey to clarify the medical history of the disease, identify risk factors for the disease, and bad habits. Then the specialist will examine the patient and examine him using physical methods: palpation, percussion, auscultation.
To identify an acute inflammatory process, it is necessary to conduct a laboratory examination (CBC, OAM, biochemical blood test, coprological study). Instrumental methods for diagnosing pancreatic pathology will require ultrasound, CT or MRI, and x-ray examination of the digestive organs.
Prevention of pancreatic inflammation
To prevent the development of acute pancreatitis (primary prevention), as well as to prevent exacerbations of chronic inflammation of the pancreas (secondary prevention), all people are recommended to follow certain rules:
- Proper nutrition based on the principles of mechanical, chemical and temperature sparing of the mucous membranes of the digestive tract. Fatty, fried, salty, spicy, and sour foods are excluded. The temperature of food and drinks is within body temperature. Dishes are served to the patient in liquid, puree, or mushy form to facilitate digestion.
- Categorical refusal of bad habits (alcohol abuse, smoking) is one of the most important rules for disease prevention.
- Maintaining a healthy lifestyle, playing sports (specially selected gymnastics), frequent walks in the fresh air.
- Compliance with the work and rest regime, exclusion of heavy physical activity and stressful situations. Sleep should be at least 8 hours a day.
- Timely diagnosis and treatment of other gastrointestinal diseases. Gallstone disease, chronic cholecystitis, any pathology of the biliary system, gastritis, duodenitis are especially important for the development of pancreatitis. Taking prescribed medications in tablets or parenterally to treat concomitant pathologies is extremely important for the prevention of pancreatitis.
Hypertriglyceridemic pancreatitis
Hypertriglyceridemic pancreatitis accounts for 1-14% of cases of AP and 56% of cases of pancreatitis in pregnant women. Hypertriglyceridemia is defined as elevated fasting triglycerides (TG) (>1.7 mmol/L). Serum TG levels above 11.3 mmol/l can lead to the development of AP in 5% of cases. In cases where the TG concentration exceeds 22.6 mmol/l, the incidence of AP is 10–20%. The risk of AP increases with a TG concentration of 5.6 mmol/l: the higher it is, the higher the risk of AP and the more severe the pancreatitis.
Pancreatitis caused by hypertriglyceridemia is associated with both primary (genetic - dyslipidemia types I, IV, V) and secondary (acquired) disorders of lipoprotein metabolism. The main causes of acquired hypertriglyceridemia are obesity, diabetes, hypothyroidism, pregnancy and medication use - treatment with estrogens or tamoxifen, beta-blockers, antiretroviral drugs, thiazide diuretics.
During pregnancy, TG levels usually rise to 3.3 mmol/L in the third trimester and do not cause pancreatitis. Inheritance is most common during pregnancy due to hereditary familial dyslipidemia.
Inflammation of the pancreas is not caused by TGs themselves, but by toxic free fatty acids formed as a result of hydrolysis of the pancreas by pancreatic lipases. The clinical picture of the disease is usually no different from ordinary pancreatitis. In some cases, severe hypertriglyceridemia, xanthoma, xantheliosis, hepatosteatosis, etc. may be observed.
It is important to promptly diagnose hypertriglyceridemic pancreatitis and correct triglyceride levels. Standard treatment of pancreatitis is also prescribed - infusion therapy, analgesics.
The main methods of reducing hypertriglyceridemia are apheresis, especially plasmapheresis, and insulin therapy. However, there is no data from randomized studies on the effectiveness of these methods. Treatment is selected based on the severity of pancreatitis and warning signs, including hypocalcemia, lactic acidosis, exacerbation of systemic inflammatory response, and progressive organ dysfunction.
Intravenous insulin should be used if the patient does not tolerate or cannot undergo apheresis. Insulin lowers TG levels, but the goal of this treatment in severe hypertriglyceridemic pancreatitis is to prevent stress-induced release of fatty acids from adipocytes. The usual dose of insulin infusion is 0.1-0.3 U/kg/h. This requires hourly blood glucose measurements. To prevent hypoglycemia, a glucose solution is prescribed.
Hourly blood glucose measurements
For therapeutic apheresis, triglyceride levels should be monitored after each procedure. Plasmapheresis is continued until the TG concentration drops to 5.6 mmol/l. For insulin alone, TG levels are monitored every 12 hours. The insulin infusion is stopped when the TG concentration reaches 5.6 mmol/L (usually after a few days).
Further long-term correction of hypertriglyceridemia with TG <2.2 mmol/L is important to prevent recurrence of pancreatitis. There are medical and non-medical measures for this. The latter include diet, weight loss for obesity, increased physical activity, limiting added sugar, and good glycemic control for diabetes. You should also avoid medications that increase TG levels. Medicines include antilipid drugs, usually fibrates (fenofibrate).
What are the prognosis for treatment?
The prognosis of chronic pancreatitis is often unfavorable. Pancreatic necrosis, or death of gland cells, is especially difficult to treat. A fatal outcome in the described case is likely.
To avoid tragedy, patients need to clearly understand that the causes of chronic pancreatitis depend on the quality of food. When diagnosed, you should not drink alcoholic beverages or eat fatty foods. The diet includes protein (mandatory) and a minimum amount of fat.
How long do people with pancreatitis live is a question that worries every sick person. Life expectancy is influenced by a number of reasons:
- Patient's age. The earlier a person gets sick, the higher the chance of recovery.
- Drinking pattern - how often ethanol is consumed.
- The degree of damage to the gland.
A young guy who recently turned 20 years old and does not drink alcohol can live with this diagnosis into old age. A man in his declining years who regularly drinks alcohol shortens his life by ten or more years.
Factors influencing life expectancy:
- Life expectancy depends on the form of the disease. Acute attacks are often fatal. In severe forms, death from pancreatitis occurs in thirty percent of patients.
- The severity of the disease affects the general condition of the body.
- Complications in the form of cyst formation, bleeding from a damaged organ, and problems with the gastrointestinal tract aggravate the situation, mainly in older patients. The mortality rate reaches 20%.
- Age category of patients.
- Regular, thoughtful treatment.
- Compliance with the doctor's requests for treatment.
- Consumption of products prescribed by a gastroenterologist.
- Refusal to drink strong and low-alcohol alcoholic beverages.
Calcific (hypercalcemic) pancreatitis
Calcific pancreatitis is very rare. The most common causes of hypercalcemia (about 90%) are hyperparathyroidism and malignancy. According to studies, hyperparathyroidism causes about 0.4% of cases of AP.
It is believed that calcium accumulated in the pancreatic duct activates trypsinogen in the pancreatic parenchyma. The low incidence of pancreatitis among patients with chronic hypercalcemia suggests that other factors (sudden increases in serum calcium levels) also influence OP.
Patients with hyperparathyroidism and associated hypercalcemia develop pancreatitis 10 to 20 times more often than the general population. The most common causes of hyperparathyroidism are:
- parathyroid adenoma (80%);
- hyperplasia of all 4 parathyroid glands (15–20%);
- thyroid cancer (2%).
Parathyroid adenoma
The most important principles of treatment are the correction of hypercalcemia and elimination of the underlying cause. In patients with asymptomatic mild hypercalcemia (calcium concentration 3.5 mmol/L), initial treatment is 200 to 300 ml/hour of isotonic sodium chloride solution based on a urine output of 100 to 150 ml per hour.
For immediate short-term treatment, patients who develop symptoms (lethargy, stupor) are given calcitonin, and for long-term treatment, an intravenous bisphosphonate is added. If bisphosphonates are contraindicated, zoledronic acid or denosumab can be used.
What is the pancreas and its functions
The organ is small in size, shaped like a willow leaf and exhibits two important functions:
- takes part in the digestion of food thanks to digestive juices;
- produces hormones that affect cells in the human body.
Insulin, which controls sugar levels, has become the main pancreatic hormone.
Pancreas
Toxic (drug-induced) pancreatitis
Drug-induced pancreatitis occurs in less than 5% of cases. The prognosis for this pancreatitis is generally good and the mortality rate is low. The pathogenetic mechanism of drug-induced pancreatitis includes:
- immunological reactions (6-mercaptopurine, aminosalicylates, sulfonamides);
- direct toxic effects (diuretics, sulfonamides);
- accumulation of toxic metabolites (valproic acid, didanosine, pentamidine, tetracycline), ischemia (diuretics, estrogens);
- increased viscosity of pancreatic juice (diuretics and steroids).
Demonstrating interactions between pancreatitis and drugs is usually difficult. Pancreatitis may develop within a few weeks of starting treatment. Rash and eosinophilia may occur. Meanwhile, patients taking valproic acid, pentamidine or didanosine do not develop pancreatitis until many months later due to chronic accumulation of the drug's metabolite.
When restarting treatment, patients should be closely monitored. If symptoms recur, the drug should be discontinued.
Symptoms
Acute pancreatitis has pronounced symptoms. Against the background of their manifestation, the patient’s condition always worsens sharply. There is always severe pain, which intensifies when lying on your back and after eating.
Constant girdle pain is localized in the epigastrium or left hypochondrium. Sometimes they radiate under the left shoulder blade. Additionally, nausea and other dyspeptic symptoms may occur. In severe cases, continuous vomiting of bile is observed, which does not bring relief. Body temperature also increases.
Autoimmune pancreatitis
Autoimmune pancreatitis (AIP) is a rare disease that causes fibrotic inflammation of the pancreas. The prevalence of the disease has not been established in detail. AIP is estimated to account for 5-6% of cases of chronic pancreatitis.
Autoimmune pancreatitis is an increasingly recognized disease. Typically, AIP begins with weight loss, jaundice, and diffuse enlargement of the pancreas in imaging studies simulating cancer.
According to international consensus criteria, autoimmune pancreatitis is divided into:
- AIP type 1, or lymphoplasmacytic sclerosing pancreatitis;
- AIP type 2, or idiopathic ductal-centric pancreatitis.
Autoimmune pancreatitis type 1 most often manifests as obstructive jaundice, in 50% of cases. Obstructive jaundice develops due to compression of the distal bile ducts (enlargement of the head of the pancreas) or stricture of the proximal bile ducts.
Obstructive jaundice
Despite intense inflammation, patients do not experience typical abdominal pain or it is mild. Autoimmune pancreatitis type 1 belongs to a spectrum of immunoglobulin (Ig) G4-related diseases that can affect almost all organs of the body (biliary strictures, interstitial nephritis, IgG4-associated glandular exocrinopathy, sialadenitis, retroperitol).
AIP should be suspected in patients with evidence of both pancreatic and hepatobiliary disorders. Elevated serum IgG4 levels are detected in most patients with type 1 AIP.
Typical radiological signs after computed tomography (CT) are:
- diffuse pancreatic parenchyma (sausage-shaped pancreas);
- frame-type rim or focal lesions;
- diffuse pancreatic atrophy.
Endoscopic retrograde cholangiopancreatography (ERCP) reveals diffuse or multifocal narrowing of the pancreatic duct without dilatation. To confirm the diagnosis, it is important to evaluate all tests, but histological examination is considered the standard of diagnosis.
Table 3. Comparison table for autoimmune pancreatitis types 1 and 2
| Type 1 AIP | Type 2 AIP | |
| Age at which the disease develops | About 60 years old | About 40 years old |
| Male | 75% | 50% |
| Damage to other organs/association with IgG4-related disease | 50% | No |
| Inflammation | Small | High (10-20%) |
| Increased serum IgG4 | Contained in approximately 66% | Set at about 25% |
| Histological data: | ||
| lymphoplasmacytic infiltration | Characterized by | Characterized by |
| storiform fibrosis | Characterized by | Characterized by |
| obliterative phlebitis | Characterized by | Rarely noticeable |
| damage to granulocytic epithelium | There is no | Characterized by |
| periductal inflammation | Characterized by | Characterized by |
| IgG4 cells | ≥10 cells/DPL (in area of significant increase) | |
| Response to steroid treatment | 100% | 100% |
| Risk of relapse | Up to 60% | |
Autoimmune pancreatitis is treated with corticosteroids at a dose of 40 mg/day. 4-6 weeks followed by a reduction of 5 mg per week. Inadequate response or relapse is more common in patients with concomitant IgG4-related sclerosing cholangitis. In this case, 2 mg/kg azathioprine is recommended.
Risk group
At risk, as Dmitry Chudayev says, are people with diseases of the biliary tract, cholelithiasis, and patients with acute surgical diseases of the abdominal organs. In addition, among the reasons for the development of pancreatitis, factors such as:
- poisoning;
- injuries;
- viral diseases;
- operations and endoscopic manipulations.
So in these cases, you should listen carefully to yourself and undergo timely examinations with a doctor to eliminate the risk of developing pathology.
“For prevention purposes, it is recommended to avoid alcohol, fatty, spicy and fried foods, especially in large quantities,” advises surgeon Chudayev.
Article on the topic
Spare the pancreas! How to protect yourself from pancreatitis