A cholecystectomy is an operation to remove the gallbladder. Currently, many techniques have been developed for this operation. Preference is given to minimally invasive (laparoscopic) interventions, as they reduce the risks of postoperative complications and minimize rehabilitation time. However, in some hospitals the routine operation is still laparotomy cholecystectomy, which is performed through incisions in the abdominal wall.
- Why is the operation performed?
- Indications and contraindications for cholecystectomy
- Types of surgery
- Operational risks
- Postoperative period
- Diet
Why is the operation performed?
The gallbladder is an important part of the digestive system. Bile collects in it, and when food enters the small intestine, the bladder contracts and throws out 40-60 ml of its contents. Bile promotes the activation of digestive enzymes, emulsifies and hydrolyzes fats, and removes excess cholesterol and bilirubin from the body.
If pathology occurs, the gallbladder can cause severe disorders, from pain to damage to the liver, pancreas, and even the development of severe septic complications. A timely operation according to indications allows one to avoid the development of severe complications and at the same time does not significantly worsen the patient’s quality of life in the future.
Recovery after gallbladder excision
All human organs work together, making the functioning of the body stable and efficient, and after excision of at least one of them, a person’s life does not become the same. If you had to have your gallbladder removed, the consequences may be the following - the presence of postcholecystectomy syndrome - a state of functional change in the biliary system after excision of the organ. In other words, after excision, the quality of life can be improved by getting rid of bad habits and establishing new useful ones: the body is rebuilt for a different job in new conditions. This can either pass without a trace or cause discomfort to the patient.
The only complication after surgery to remove the gallbladder is postcholecystectomy syndrome. It appeared in Western medical literature in the 30s of the 20th century. After excision of the organ, the contractility of bile is disrupted: it flows poorly into the duodenum. There is pain in the side, nausea, the body quickly becomes full after a small amount of food.
Here's how gallbladder removal affects the body .
Indications and contraindications for cholecystectomy
The most common indication for this operation is the development of complications of cholelithiasis (hereinafter referred to as cholelithiasis) and some acute pathologies of the gallbladder (GB):
- Acute cholecystitis. If left untreated, it can cause severe complications, including the development of peritonitis, abscesses and sepsis. If there are no stones, the patient can be managed conservatively. But with calculous acute cholecystitis, emergency surgery is indicated.
- Choledocholithiasis is the presence of stones in the bile ducts. In this case, obstruction (blockage) of the ducts and the development of a serious complication - obstructive jaundice - are possible. In addition, cholangitis and pancreatitis develop. During the operation, not only the gallbladder is removed, but also the bile ducts are sanitized. In some cases, drains are installed.
- Symptomatic cholelithiasis. The absolute indication for surgical intervention is hepatic colic due to cholelithiasis. It is also recommended to remove the bladder for other symptoms: bitterness in the mouth, as well as heaviness or aching pain in the right hypochondrium.
- Asymptomatic cholelithiasis. Previously, it was believed that in the presence of stones, cholecystectomy was indicated in any case, since doctors were afraid of the development of a malignant neoplasm against this background. But further observations showed that the likelihood of malignancy is low. Now removal is recommended only for the following indications: if the size of the stones exceeds 2.5-3 cm, and if the patient’s life expectancy is 20 years or more. In the latter case, the likelihood and severity of long-term complications are higher than the risks of surgery.
- Calcification of the gallbladder - deposits of calcium salts. It is complicated by the development of a malignant neoplasm in almost 25% of cases.
- Cholesterosis of the gallbladder is the deposition of cholesterol in the wall of the bladder. Cholecystectomy is performed for calculous cholesterosis and/or when its functionality is impaired.
- Gallbladder polyps. Surgery is indicated if the polyps are larger than 1 cm in size, or if they have a vascular pedicle. In other cases, dynamic observation is carried out.
Planned operations are not performed if the patient has acute infectious diseases or decompensation of chronic pathologies. If emergency intervention is necessary, the benefit/risk ratio is assessed individually.
How is cholecystectomy performed?
Bladder excision, or cholecystectomy, is the surgical removal of the gallbladder. In modern medicine, abdominal surgery is no longer performed, which requires a long recovery time.
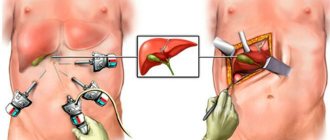
Today, cholecystectomy is often performed using laparoscopy , through small incisions in the abdomen into which a camera and instruments are inserted. Incisions of about 1 cm are enough to carefully remove the organ, relieving the patient of pain due to cholecystitis. The advantage of modern clinics is that they use an innovative laparoscopic endovideosurgical stand, which supplies carbon dioxide heated to human body temperature to the abdomen. This allows you to do all the actions as gently as possible, which means it reduces the time of tissue regeneration after surgery. All actions are carried out using high-quality optics, which increases visibility during the intervention. The operation is performed under general anesthesia and lasts about 40 minutes.
Types of surgery
There are two types of cholecystectomy practiced in Russia:
- Laparoscopic - all manipulations are performed through small punctures using endoscopic equipment. Currently, this technology is the gold standard for elective interventions in the absence of significant inflammation and adhesions.
- Laparotomy, or traditional open. It is carried out in case of adhesions and severe inflammation.
Let's consider each of the methods in more detail.
Laparoscopic cholecystectomy
The technique of this operation consists of making 3-4 punctures on the abdominal wall, through which hollow tubes (trocars) are inserted into the abdominal cavity, and through them instruments - a video camera, manipulators, clamps, electrodes, etc. Modern video cameras allow you to obtain high-quality detailed enlarged images, which is broadcast to the monitor. This allows for better visualization than with open abdominal surgery.
In order to have sufficient visibility and space for manipulation, the abdominal cavity is expanded using gas. Its insufflation (pumping) is carried out throughout the operation through a separate trocar. Next, the gallbladder and its structures are isolated. Its artery is ligated, its neck is cut off, and the bladder is removed through one of the trocars. After this, an inspection is carried out, the gas is sucked off and the tubes are removed. Drainage is installed in the wound, the punctures are sutured and sealed with a sterile plaster and bandage.
Advantages of laparoscopic surgery:
- Very low risk of abdominal wall trauma.
- Postoperative pain syndrome is practically absent.
- Very fast recovery and short hospital stay.
Traditional cholecystectomy
This operation (laparotomy cholecystectomy) is performed through an incision in the right hypochondrium or along the midline of the abdomen. It provides good access to the entire hepatobiliary system - extrahepatic ducts, pancreas, duodenum. This allows for all types of revision - from duct probing and intraoperative ultrasound to choledochoscopy. Most often, such operations are performed in cases of serious inflammatory processes, in particular peritonitis and abscesses.
There are situations when laparoscopic surgery is initially planned, but in the process of performing it, surgeons see serious complications and are forced to switch to open access. This situation is called conversion.
Causes
Currently, there are several most likely causes of the formation of gallstones. It is expected that this could be:
- stagnation of bile of a mechanical or functional nature; with mechanical - the outflow of bile is obstructed due to obstacles (adhesions, kinks, tumors, etc.), with functional - disturbances arise due to impaired motility of the gallbladder.
- disturbance of bilirubin or lipid metabolism, which affects the circulation and synthesis of bile; cholesterol, bile pigments, salts are precipitated, the quantitative ratio of bile components is also disrupted, and solid formations appear.
The presence of unfavorable factors may be decisive in the development of the disease. The largest number of patients are in developed countries, with older people predominating; perhaps the reason lies in lack of exercise, poor diet, and stress. Also, the risk of this disease is higher in women. In addition, the likelihood of stone formation increases:
- obesity: in people with a body mass index of more than 35, cholelithiasis is diagnosed 20 times more often;
- dietary features: predominance in the diet of foods containing large amounts of cholesterol, abuse of low-calorie foods, sudden weight loss (more than 1.5 kg per week);
- various diseases: metabolic disorders, Crohn's disease, diverticula, infections, etc.;
- burdened heredity: among relatives there are already patients with the same diagnosis;
- long-term use of drugs that affect metabolic processes.
Operational risks
Cholecystectomy, like any other operation, may be accompanied by the development of complications and unwanted reactions. They can be divided into several groups:
Complications from the wound:
- Hematomas and hemorrhages.
- Wound infection. Accompanied by redness of the skin, thickening and the release of pathological discharge. Requires urgent medical attention.
Complications from the abdominal cavity:
- Residual choledocholithiasis. As we know, gallstones can form not only in the gallbladder, but also in the ducts. At the preoperative stage, they try to detect them and solve this problem during cholecystectomy. But in some patients it is not possible to detect stones either preoperatively or intraoperatively. Remaining stones can cause complications, such as obstructive jaundice. Then repeated intervention is required.
- Bile leakage. In the early postoperative period, bile may be separated from the gallbladder bed. To divert it, a drainage is inserted into the wound at the end of the operation. Usually this situation lasts 2-3 days and stops on its own. The only thing required here is observation in a hospital.
- Damage to the bile ducts. As a result, bile leakage may develop. Then the drainage discharge remains for more than 2-3 days. In this case, repeated surgery and long-term rehabilitation are required.
Despite the fact that any surgical intervention may be accompanied by the development of complications, it is still worth noting that their risk is negligible when the operation is performed by an experienced surgeon in a well-equipped operating room.
In what situations is the gall bladder removed?
When an ultrasound examination reveals sand or small stones that do not cause attacks and can be crushed and dissolved, there is no need for surgical intervention. The indication for manipulation is damage to the organ itself. Most often, laparoscopic cholecystectomy is performed - a minimally invasive and low-traumatic operation using special instruments and modern technology. Pathologies for which it is performed:
- cholelithiasis leading to the formation of stones. During the period of inflammation, a pronounced pain syndrome occurs due to stones getting stuck, causing spasms of the bile ducts;
- acute cholecystitis is a complication of cholelithiasis that can lead to serious consequences in the form of sepsis (blood poisoning), damage and rupture of the walls of the gallbladder, followed by peritonitis;
- polyposis – benign growths of the mucous membrane, prone to malignancy (malignancy). Laparoscopy will be required if they increase in size, their number is more than two units, their diameter exceeds 10 mm, or the patient has clinical signs that worsen the quality of life;
- cholesterosis, associated with a slowdown in lipid metabolism in the body, which leads to the accumulation of cholesterol deposits on the walls of the organ and functional disorders. Surgery is necessary when diet and drug therapy do not produce positive results.
Postoperative period
Features of the recovery period after surgery are determined by the technique of its implementation. With laparoscopic intervention it is relatively easy. After just 6 hours you can sit down on the bed and gradually get up under the supervision of medical staff. The next day you can safely move around the department. As for food, they begin to eat light food on the second day after cholecystectomy. The drainage can be removed on the same day. On average, recovery takes about a month, but the time frame may increase depending on the general condition of the patient. Open surgeries sometimes require longer bed rest and pain relief.
Preparing for surgery
The methods of preparing for surgery are similar and do not depend on where laparoscopic cholecystectomy is performed in Moscow.
Before the procedure, the patient undergoes a full examination at the medical center. Laboratory and instrumental diagnostic measures are prescribed - blood and urine tests, ultrasound, and, if necessary, MRI. Their goal is to determine the patient’s health status and identify concomitant pathologies that require correction before surgery. If pathologies that impede the operation are identified, treatment will be prescribed to compensate for the disease.
In the absence of contraindications, cholecystectomy is prescribed. Preparation for the procedure:
- Follow a special diet the day before surgery. You can only eat light foods that do not overload the digestive tract.
- Dinner the day before is allowed no later than 19:00.
On the day of surgery, you should not eat or drink. If the patient regularly takes any medications, their use should be coordinated with the surgeon and anesthesiologist. In most cases, therapy is not interrupted.
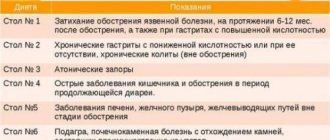
Diet
An important point in the recovery period is diet. During this period, it is recommended to give up alcohol, heavy foods (fats, marinades, smoked foods), and light carbohydrates. Small meals 4-6 times a day are recommended.
In the federal network of expert oncology clinics “Evroonko”, cholecystectomy is performed laparoscopically if there are no contraindications. We use expert-class equipment, staffed by highly qualified specialists.
Book a consultation 24 hours a day
+7+7+78
Prognosis and recommended lifestyle
Every person undergoing surgery is concerned about the question of how his future existence will turn out. Will it be the same as before, or will it become less complete due to restrictions? It all depends on gender and age, the patient’s health status, the rate of tissue healing, and the presence of chronic diseases. Not only proper nutrition is of great importance, but also reasonable physical activity. Spending a long time in a chair or lying on the sofa leads to obesity and causes stagnation of bile. Gentle exercises, walks in the fresh air, measured work at home and in the garden help to increase its circulation. Short swimming in the pool several times a week improves metabolism and relaxes the spine. If you or your loved ones need professional support in rehabilitation after surgery, our specialists will help with this. Sign up for a free initial consultation to discuss further steps with your doctor that will make it possible to avoid post-operative complications and re-formation of stones, as well as reduce rehabilitation time.
Possible complications
Among the common ones are the development of the inflammatory process and obstruction (block) of the biliary tract, which can lead to obstructive jaundice and acute pancreatitis. Also, in the absence of timely treatment, the appearance of fistulas, bladder rupture, the development of peritonitis and other complications dangerous to humans is possible.
To identify cholelithiasis, determine the degree of inflammation in the wall of the gallbladder, as well as select the correct individual tactics of surgical treatment, you must send me a complete description of an ultrasound of the abdominal organs, preferably a gastroscopy, to my personal email address, you must indicate your age and main complaints. In rare cases, if stones in the ducts are suspected, it is necessary to perform an endoscopic ultrasound examination of the ducts and pancreas. Then I will be able to give a more accurate answer to your situation.