Treatment of wounds of the perineum and anal canal still remains one of the pressing health problems [1]. The search for effective means for the treatment of postoperative wounds continues to concern operating surgeons and attending physicians, since due to constant microbial contamination of intestinal contents, small-scale operations are accompanied by prolonged healing of postoperative wounds and, as a consequence, an increase in rehabilitation time [1-4].
Currently, among many different drugs, there are modern, quite effective drugs for topical use, which have virtually no side effects [5, 6]. Such drugs, which also have a unique mechanism of action, include the drug Posterisan, developed in the form of an ointment for rectal use [7]. Dosage: 1 g contains microbial bodies and metabolic products of 330 million killed Escherichia coli bacteria. The shelf life of the medicinal product is 3 years.
Posterisan belongs to the group of immunobiological drugs and has a regenerating, antipruritic, anti-inflammatory effect, as well as (and this is most important) an immunostimulating effect. Posterisan forms specific and stimulates nonspecific immunity. Stimulates the T-system of immunity, increases the phagocytic activity of leukocytes and cells of the reticuloendothelial system, a number of humoral factors of nonspecific immunity. Increases the formation of antibodies at the site of exposure and local tissue resistance to the effects of pathogenic microflora due to the content of concentrated lipopolysaccharides of cell membranes and metabolites of E. coli of various strains, including those resistant to antibiotics and other antibacterial agents. Reduces exudation, normalizes the permeability and tone of blood vessels, stimulates the regeneration of damaged tissues.
At the State Research Center of Coloproctology named after. A.N. Ryzhikh conducted a study to evaluate the effect of the drug posterizan on the healing of postoperative wounds of the anal canal and perineum.
To achieve this goal, it was necessary to solve the following tasks: 1) assess the rate of healing of the postoperative wound; 2) calculate the frequency of postoperative complications; 3) analyze data from a cytological examination of fingerprint smears taken from the wound surface; 4) monitor how quickly patients’ ability to self-care is restored in the postoperative period; 5) study the quality of life of patients before and after surgery.
Composition and release form
| Ointment | 1 g |
| microbial cells of E. coli killed by phenol | 500 million |
| hydrocortisone (in 166.7 mg aqueous suspension) | 2.5 mg |
| excipients: lanolin; Vaseline (yellow) or paraffin (yellow, soft); phenol |
in aluminum tubes (with applicator) 25 g, complete with applicator; 1 tube in a box.
| Rectal suppositories | 1 sup. |
| microbial cells of E. coli killed by phenol | 1000 million |
| hydrocortisone (in 387.1 mg aqueous suspension) | 5 mg |
| excipients: solid fat; macrogolglycerol; hydroxystearate; acetylcysteine; phenol (preservative); ethylenediaminetetraacetate disodium salt |
5 pcs in blister; There are 2 blisters in a box.
Pharmacodynamics
A combined drug containing two active components - a suspension of a bacterial culture containing inactivated bacteria and their metabolic products, and hydrocortisone. Stimulates the T-system of immunity, increases the phagocytic activity of leukocytes and cells of the reticuloendothelial system, increases the role of a number of humoral factors of nonspecific immunity (induces the formation of cytokines), enhances the formation of antibodies at the site of exposure. Concentrated lipopolysaccharides of cell membranes and metabolites of E. coli of various strains, incl. resistant to antibiotics and other antibacterial agents, lead to an increase in local tissue resistance to the effects of pathogenic microflora. Hydrocortisone (contained in a small dose) complements the effect of a bacterial culture suspension due to its anti-inflammatory, antiallergic and antipruritic effect, which is manifested in reducing exudation, normalizing the permeability and tone of blood vessels, reducing swelling, hyperemia, itching, and stimulating the regeneration of damaged tissues.
Posterisan
Posterisan is an immunostimulating drug for the local treatment of diseases of the anorectal area. The basis of posterizan is made up of inactivated Escherichia coli bacteria, their metabolic products and metabolites. This entire bacterial mass acts as an antigen - a substance perceived by the body as foreign and, for this reason, inspiring the latter to mobilize all its immune resources. Available in the form of ointment for rectal and external use and rectal suppositories. When posterisan is applied topically to the skin and mucous membranes, it penetrates the inflamed tissue and acts as a kind of “vaccination” that activates the body’s own defenses at the site of inflammation. As a result of contact with the drug, T-lymphocytes are activated, which begin to intensively produce cytokines, which in turn have a stimulating effect on macrophages and granulocytes. The latter, with a remarkable appetite, begin to absorb cell fragments, whose unwanted presence became the cause of the inflammatory reaction. Thanks to posterisan, the production of secretory immunoglobulins is stimulated, which begin to bind and neutralize antigens. Cytokines perform another important function in this case: they activate the process of collagen synthesis, which takes an active part in the regeneration of tissues damaged by inflammation. In addition to this, it should be noted that posterizan reduces vascular exudation, normalizes the tone and permeability of the walls of blood vessels, and also increases the local resistance of tissues to the effects of pathogenic bacteria.
Posterizan ointment is applied in a thin, even layer to the affected area of the skin or mucous membranes several times a day: morning and evening, as well as after each bowel movement. If you need to administer the ointment deeply, you can use the screw-on plastic applicator included in the package. To do this, it should be put on a tube with ointment, and then inserted into the rectum.
After use, the applicator is washed and dried. Posterizan in the form of rectal suppositories is used with the same frequency as ointment - in the morning and evening, as well as after each visit to the toilet “in a big way”. In each case, one suppository is used. After introduction into the rectum, it gradually melts under the influence of body temperature, which ensures continuous and uniform release of the active substance directly at the site of inflammation. It is no secret that the skin of the anorectal area is particularly sensitive, and therefore the suppository is administered carefully and without effort or sudden movements. This may seem insignificant, but it is recommended to cut your fingernails to avoid damage to the skin. Suppositories should be administered after bowel movements. Immediately after this exciting moment, it is necessary to spend some time in a horizontal position so that the suppository mass can dissolve and release all its “ammunition”. Easing your fate by involving various lubricants or creams in the process is highly not recommended: in this way, the absorption characteristics of the active substance can be changed for the worse. The only thing that can be done to improve the sliding of the suppository is to hold it in your hand or warm it in warm water. It is not at all necessary to insert the suppository “all the way”: the criterion for optimal depth of penetration into the rectum is the ability to palpate it with a fingertip. In this matter, it is important to observe the “golden mean”, because if the injection is not deep enough, the suppository will not reach the hemorrhoids. The creators of posterizan recommend using pads during the course of medication: this way you can avoid soiling your underwear and ensure dry skin in the anorectal area. Ointment and suppositories of posterizan are perfectly combined with each other, which opens up additional therapeutic possibilities. The average duration of treatment is 2-3 weeks.
Directions for use and doses
Externally, rectally. Apply a thin layer to the affected area in the morning and evening, as well as after each bowel movement. For deeper introduction of the ointment into the anal canal, you can use a screw-on applicator. Rectal suppositories are used in the acute period of the disease, 2–3 pcs. per day. After eliminating the subjective symptoms of the disease, the affected area continues to be lubricated once a day or 1 supp. 1 time per day for several days. If the drug is used to treat chronic dermatitis, then after the disappearance of skin manifestations, it is recommended to extend therapy for another 1–2 weeks. The combined use of ointments and suppositories is possible. After completing the course of treatment, to consolidate the therapeutic effect, it is advisable to use a drug (ointment or suppositories) that does not contain hydrocortisone for another 2-3 weeks.
results
Since a standard analgesic regimen with the prescription of non-steroidal anti-inflammatory drugs was used in the postoperative period, the quality of life and pain intensity did not have statistically significant deviations in the main and control groups.
However, the data obtained from clinical and cytological assessment of the course of the wound process differed significantly in these two groups of patients.
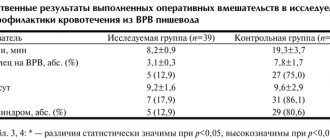
In patients after surgical treatment of anal fissure using controlled pneumodivulsion of the anal sphincter, a significant number of cases showed hyperthermia greater than 37.5 °C, which persisted for almost 2 days. The use of the study drug posterisan influenced the course of the postoperative period. In the control group, hyperthermia was observed in 83% of patients; its duration for 2 days was observed in almost half of all patients (48% of cases). When posterizan was used, hyperthermia in the postoperative period was observed in only 56% of patients; in most of them, the temperature stabilized by the end of the 1st day, and in only 8% of patients it persisted for 2 days ( p
<0.05) (Table 3).
Table 3. Clinical assessment of the course of the wound process in patients of the main and control groups, abs.
(%) All patients underwent cytological examination on days 2, 15 and 28 after the surgical stage of treatment. In the group using the study drug, the results of cytological examination were significantly better than in the control group. Thus, on the 15th day in the main group there was not a single patient with active inflammation, while in the placebo group, cytological signs of active inflammation remained in 59% of patients. On the 28th day in the main group, 63% of patients observed healing of the wound surface with the formation of a connective tissue scar, however, in the control group, only 2 (4.2%) patients achieved complete epithelization of the wound ( p
<0.05) (Table 4).
Table 4. Cytological assessment of the course of the wound process in patients of the main and control groups, abs.
(%) It is necessary to note the role of the study drug in the healing processes of the wound surface and the rate of contraction of the postoperative wound. On the day of surgery, there was no statistically significant difference between the area of the wound surface in both study groups (2.09 cm2 in the control group and 2.05 cm2 in the main group). When using posterizan on the 15th day, the wound surface area was 1.13±0.28 cm2, and in the placebo group - 1.72±0.47 cm2 (the average wound area in the control group remained 34% larger than in the main group) . The same trend continued on the 28th day. The indicators are respectively equal to 0.50±0.22 cm2 in the main group and 0.84±0.34 cm2 in the control group and differed from each other by 41% ( p
<0.05) (Fig. 3).
Fig.3. Dynamics of the healing area of the surgical wound.
Drug safety
It should be emphasized once again that during the study, not a single adverse event that arose during the use of the drug was registered.
Complications in the late postoperative period
In patients of the main group, all wounds healed within normal periods - up to 45 days. In patients of the control group, in 5 (10.4%) cases, the presence of a long-term non-healing wound of the anal canal was diagnosed, i.e., the healing process was more than 45 days after surgery (from 46 to 85 days).
During a cytological examination when contacting for a long-term non-healing wound in these 5 (10.4%) patients of the main group, a picture of “perverted” repair was observed with the presence of multinucleated cells such as foreign bodies in smears from wounds, as well as a chronic inflammatory process with a large number of unchanged leukocytes. The number of leukocytes in the wounds ranged from 30 to 80 per field of view.
In these patients, various microorganisms were identified in the discharge of postoperative wounds during microbiological examination. Such clinically significant microorganisms as Proteus
mirabilis
(Proteus) were detected in 2 cases,
Acinetobacterl woffi
(Acinetobacter) - in 1,
Staphylococcus aureus
(Staphylococcus aureus) - in 4,
Streptococcus haemolyticus
(hemolytic streptococcus) - in 3 observations. When quantified in patients with non-healing wounds, these microorganisms exceeded 105 CFU.
In patients in the control group with long-term non-healing wounds, various microorganisms were identified, including sexually transmitted ones: in 2 patients - trichomonas in combination with chlamydia, in 2 - trichomonas in combination with cytomegaloviruses. In one patient, an association of candida and gardnerella was detected.
All patients with long-term non-healing wounds who were diagnosed with sexually transmitted infections were prescribed appropriate therapy depending on the pathogen isolated.
As a result of the treatment, recovery was noted in all patients with long-term non-healing wounds.