Clinical picture
Clinical manifestations of hemorrhoids are different in acute and chronic course of the disease.
The main symptom of acute hemorrhoids is most often pain in the anus, caused by thrombosis of hemorrhoidal vessels. In the presence of pronounced edema and inflammatory infiltration of surrounding tissues, a false impression of strangulation of hemorrhoids may be created. Most often, thrombosis of hemorrhoids begins with the internal ones, and then moves to the external hemorrhoidal plexuses, thus causing combined hemorrhoids. With this type of development of acute hemorrhoids, the main symptom is severe pain in the anus. If isolated thrombosis of external hemorrhoids develops (which is quite rare), upon examination of the perianal area, dense round-shaped formations of a purplish-blue color can be detected, which can persist for 2-3 months.
Typical symptoms of chronic hemorrhoids are periodic bleeding (usually during bowel movements) and prolapse of hemorrhoids outside the anal canal. Possible, but optional, signs of chronic hemorrhoids are pain, discomfort in the anal canal, and itching of the perianal skin.
Bleeding of varying severity is observed in more than half of the patients, which emphasizes the dominant role of this symptom in the diagnosis of chronic hemorrhoids. Typically, patients note the release of scarlet blood without clots, which can either be released abundantly from the anus, splashing the walls of the toilet, or leave a trace only on toilet paper. Sometimes streaks of scarlet blood can be detected in the stool. Most often, anal bleeding is periodic, that is, observed during or immediately after defecation. Less commonly, there is constant bleeding from the anus. Regular bleeding can lead to a decrease in peripheral blood hemoglobin levels and the development of anemia.
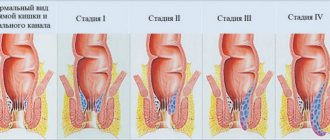
Prolapse of hemorrhoids becomes a characteristic sign of the disease in the later stages of chronic hemorrhoids, when dystrophy and atrophy of the ligamentous-muscular apparatus holding the hemorrhoidal plexus occurs. In the initial stages of hemorrhoid development, this symptom is the leading one only in a small proportion of patients. Prolapsed hemorrhoids are defined as soft-elastic dark cherry-colored formations, covered with mucous membrane, protruding into the lumen of the anal canal.
Pain in the anus in patients with chronic hemorrhoids is not a pathognomonic sign, as it is observed in a number of other proctological diseases. Most often, the pain syndrome is caused by the development of complications of hemorrhoids - the formation of acute and chronic anal fissure. Discomfort and anal itching can join other symptoms of hemorrhoids in later stages of the disease, most often in patients with pronounced functional changes in the colon and obturator apparatus.
Hemorrhoids: causes, symptoms, diagnosis and treatment approaches
The term “hemorrhoids” comes from the Greek words “haema” - blood and “rhoos” - flows and was first found in the writings of Hippocrates when describing bleeding from the anus [1]. The disease is mentioned in ancient medical works of various cultures, Babylonian, Hindu, Greek, Egyptian.
Being a widespread disease, occurring in 36% of the population of economically developed countries, hemorrhoids rank first in the structure of proctological diseases [2]. A significant number of patients are young and of working age, which indicates the significant social and economic significance of the problem under consideration.
For many years, there has been a theory of varicose veins, which states that hemorrhoids develop due to varicose veins in the anal canal. Today it has been proven that the formation of hemorrhoids includes a wide range of pathological changes, including venous dilatation, vascular thrombosis, degenerative changes in collagen fibers and fibroelastic tissues, deformation and rupture of the anal subepithelial muscle [3, 4]. An additional aggravating factor is the addition of inflammatory changes in the vascular wall and surrounding connective tissue. Recent data show the participation of a number of enzymes, primarily matrix metalloproteinases (MMPs) and zinc-dependent proteinase in the degradation of connective tissue and the destruction of extracellular matrix proteins (elastin, fibronectin, collagen). The role of MMP-9 in the destruction of elastic fibers has been established [4]. Activation of MMP-2 and MMP-9, thrombin, plasmin or other proteinases is accompanied by disruption of capillary blood flow and activation of transforming growth factor β (TGF-β) [5]. Hypervascularization and increased microvascular density are an important pathogenetic factor in hemorrhoids. [6]. Microvascular density increases in hemorrhoidal tissues. An increase in the level of endoglin (one of the TGF-β binding sites) is a marker of vascular proliferation [7]. It has been shown that the diameter of the superior rectal artery in patients with hemorrhoids has a significantly larger diameter and a higher peak blood flow velocity compared to healthy individuals. These changes persist even after surgical treatment of hemorrhoids [8, 9].
There is a connection with defecation disorders, in particular with stool frequency [10–12]. Data on the role of dietary factors, including low protein diet, consumption of spicy foods, and alcohol, remain controversial [13].
At the present stage, the following are considered as the main mechanisms for the development of hemorrhoids (L. L. Kapullera (1974), G. I. Vorobyova et al. (2002)):
- Vascular dysfunction caused by increased arterial blood inflow and decreased outflow through the cavernous veins.
- Dystrophic processes in the common longitudinal muscle of the submucosal layer and the ligament of Parks, which hold the cavernous plexus in the anal canal.
- Destruction of the fibromuscular framework of the internal hemorrhoids, holding them in the anal canal above the anorectal line, combined with increased arterial blood flow, an increase in the size of the hemorrhoids, displacement in the distal direction and, ultimately, prolapse from the anal canal.
Loss of elasticity leads to mobility of hemorrhoids, which, under the influence of pressure in the rectum, begin to move towards the anal canal (if problems arise with emptying the rectum and constipation). In advanced stages, the suspensory ligament and Parkes' ligament rupture and the internal hemorrhoids begin to prolapse.
Classification of hemorrhoids
In practice, the following four categories of hemorrhoids are most often used:
1) acute/chronic; 2) external/internal; 3) complicated/uncomplicated; 4) stage of hemorrhoids according to the degree of prolapse and reducibility of the nodes.
In the International Classification of Diseases ICD-10 (1995, WHO, Geneva), the following forms of hemorrhoids are distinguished in the section of venous diseases:
- I 84 hemorrhoids;
- I 84.0 internal thrombosed hemorrhoids;
- I 84.1 internal hemorrhoids with other complications (bleeding);
- I 84.2 internal hemorrhoids without complications;
- I 84.3 external thrombosed hemorrhoids;
- I 84.5 external hemorrhoids without complications;
- I 84.6 residual hemorrhoidal marks;
- I 84.7 thrombosed hemorrhoids, unspecified;
- I 84.8 hemorrhoids with other complications, unspecified;
- I 84.9 hemorrhoids without complications, unspecified.
Clinical manifestations of hemorrhoids
The most common presentation of hemorrhoids is rectal bleeding associated with bowel movements, described by patients as "having a drop of blood in the toilet." Blood is typically bright red in color [13–15]. A typical symptom complex of the chronic course of the disease consists of repeated bleeding, usually associated with defecation, prolapse of hemorrhoids from the anus during and after defecation, and pain in the anus. Bleeding from the anus is observed in 76% of patients. Prolapse of hemorrhoids (as the first symptom) is observed in 39% (G. I. Vorobyov, 2006). Hemorrhoidal bleeding usually occurs during bowel movements. In this case, scarlet blood is released from the anal canal in the form of frequently dripping drops after defecation, separately from the intestinal contents. Sometimes blood appears in streaks in the stool. Relatively rarely (in 10% of cases) bleeding is permanent. In even rarer cases, blood may stagnate in the rectum, and clots and dark red blood may be present. The volume of blood loss can vary significantly. Blood may be barely noticeable on toilet paper, or it may splatter on the toilet. Before claiming that this is hemorrhoidal bleeding, it is necessary to perform an irrigation and colonoscopy, which will exclude all other causes of bleeding, especially colon tumors.
A positive stool occult blood test or the presence of anemia are usually not associated with hemorrhoids and require the exclusion of a number of bowel diseases, including colorectal cancer.
Pain is not a characteristic sign of chronic hemorrhoids. However, if pain occurs, it is necessary to determine its type, find out whether it is acute or chronic and how its intensity manifests itself during rectal emptying. Dull, constant pain is characteristic of a long course of the disease with frequent exacerbations. Pain after defecation with hemorrhoids is more typical for acute thrombosis of internal hemorrhoids and anal fissure. Thus, if the patient’s main complaint is pain, other causes should be sought [16].
Discomfort and anal itching, especially severe in patients with irritable bowel syndrome or other functional diseases of the gastrointestinal tract, are more characteristic signs of the later stages of the disease. Anal itching with hemorrhoids is usually associated with prolapse of nodes and mucus on the skin, resulting in maceration of the skin of the perianal area. At the same time, contact dermatitis may develop in this area as a result of the use of anal suppositories or ointments containing irritating components.
Perianal swelling of the skin is, as a rule, a manifestation of acute hemorrhoids and is quite rare in chronic cases. Swelling is sometimes accompanied by a feeling of discomfort, which patients often mistake for a feeling of heaviness in the perineum and anus and a desire to have a bowel movement. In the chronic phase, perianal edema is associated with frequent prolapse of hemorrhoids and is accompanied by other symptoms, in particular mucus discharge and bleeding.
Pathological discharge from the rectum in the form of mucus cannot be called pathognomonic for hemorrhoids, since they can occur in other pathological conditions of the colon. Almost all patients with pathological discharge from the anal canal have concomitant diseases of the rectum and colon.
The diagnosis of hemorrhoids is based on a clinical examination, which includes physical examination, digital examination, and anoscopy. Considering that every third patient with hemorrhoids has concomitant diseases of the anal canal, rectum and colon, it is mandatory to perform sigmoidoscopy and colonoscopy, which will identify other intestinal diseases accompanied by bleeding. Thus, 1% of patients referred for consultation to a proctologist were diagnosed with rectal or colon cancer. All patients are advised to consult a therapist with general clinical research methods [16].
Classification of hemorrhoid treatment methods [17]
I. Conservative (diet with a high content of dietary fiber, phlebotonic drugs, suppositories, ointments).
II. Minimally invasive:
- infrared coagulation;
- sclerosing treatment;
- latex ligation of hemorrhoids;
- suture ligation of hemorrhoidal arteries under Doppler ultrasound control.
III. Surgical methods:
- hemorrhoidopexy (Long's operation);
- hemorrhoidectomy according to Milligan-Morgan, Parks, Ferguson.
When choosing a treatment method for hemorrhoids, the practitioner must remember that the hemorrhoidal plexus is a normal anatomical structure and should not be removed in the absence of clinical symptoms of the disease. Considering the significant role of the internal hemorrhoidal plexuses in sealing the anal canal, it is necessary to try to use more gentle methods of treating hemorrhoidal disease. Studies by foreign and domestic coloproctologists indicate that radical hemorrhoidectomy is indicated for no more than 30% of patients with hemorrhoidal disease [18].
Algorithm for choosing a treatment method
Stage I: conservative treatment (normalization of intestinal function, phlebotonic therapy) in combination with minimally invasive treatment methods (sclerosing treatment, infrared coagulation, bipolar coagulation).
Stage II: conservative therapy and minimally invasive treatment methods (sclerosing treatment, infrared coagulation, bipolar coagulation, ligation of internal hemorrhoids with latex ligatures).
Stage III: sclerosing treatment, bipolar coagulation, ligation of internal hemorrhoids with latex ligatures, a combination of treatment methods.
Stage IV: Longo operation, Milligan-Morgan hemorrhoidectomy, Parkes hemorrhoidectomy, Ferguson hemorrhoidectomy.
Lifestyle changes are recommended for patients with any stage of hemorrhoids as part of treatment and as a preventive measure [19]. These changes include increasing dietary fiber and fluid intake, decreasing fat intake, regular exercise, and improving anal hygiene. Because the effect of passing hard stool on the anal lining can cause additional trauma to the hemorrhoids, increasing fiber intake in the diet may help relieve strain during bowel movements. According to clinical studies, the inclusion of dietary fiber in the diet reduces the risk of bleeding by 50%, but does not reduce the manifestations of prolapse and symptoms such as pain and itching.
Oral flavonoids. Venotonic agents increase vascular tone, reduce capillary permeability, and have an anti-inflammatory effect. A recent meta-analysis of 14 randomized clinical trials involving 1514 patients evaluating the effectiveness of flavonoids in the treatment of hemorrhoids showed that flavonoids reduced the risk of bleeding by 67%, persistent pain by 65%, itching by 35%, and reduced the recurrence rate by 47% [20].
Local treatment. The main goal for most topical creams and suppositories is to control symptoms. Most drugs are over-the-counter products. Medicines may contain various components, such as local anesthetics, corticosteroids, antibiotics. Tjandra et al. [20] showed good results when treated with an ointment containing nitroglycerin to relieve symptoms. Perrotti reported good efficacy of topical nifedipine ointment in the treatment of acute thrombosed external hemorrhoids [20]. It is worth noting that the effect of topical nitrates and calcium channel blockers on the relief of hemorrhoidal symptoms may be due to their effect on the relaxation of the internal anal sphincter.
Thus, hemorrhoids are one of the common diseases with a complex and not fully understood pathogenesis and a high prevalence of risk factors among the population. Numerous pathogenetically based methods of treating hemorrhoids (conservative, minimally invasive, surgical) should be used depending on the stage of hemorrhoidal disease. Timely diagnosis and choice of rational tactics for patient management will reduce the economic costs of treatment and improve the quality of life.
Literature
- Leff E. Hemorrhoids // Postgrad Med. 1987; 82:95–101.
- Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study // Gastroenterology. 1990; 98: 380–386.
- Thomson WH The nature of haemorrhoids // Br J Surg. 1975; 62:542–552.
- Han W., Wang ZJ, Zhao B., Yang XQ, Wang D., Wang JP, Tang XY, Zhao F., Hung YT Pathological change of elastic fibers with difference of microvessel density and expression of angiogenesis-related proteins in internal hemorrhoid tissues // Zhonghua Weichang Waike Zazhi. 2005; 8:56–59.
- Yoon SO, Park SJ, Yun CH, Chung AS Roles of matrix metalloproteinases in tumor metastasis and angiogenesis // J Biochem Mol Biol. 2003; 36: 128–137.
- Han W., Wang ZJ, Zhao B., Yang XQ, Wang D., Wang JP, Tang XY, Zhao F., Hung YT Pathological change of elastic fibers with difference of microvessel density and expression of angiogenesis-related proteins in internal hemorrhoid tissues // Zhonghua Weichang Waike Zazhi. 2005; 8:56–59.
- Chung YC, Hou YC, Pan AC Endoglin (CD105) expression in the development of haemorrhoids // Eur J Clin Invest. 2004; 34: 107–112.
- Aigner F., Gruber H., Conrad F., Eder J., Wedel T., Zelger B., Engelhardt V., Lametschwandtner A., Wienert V., Böhler U. et al. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease // Int J Colorectal Dis. 2009; 24: 105–113.
- Aigner F., Bodner G., Gruber H., Conrad F., Fritsch H., Margreiter R., Bonatti H. The vascular nature of hemorrhoids // J Gastrointest Surg. 2006; 10: 1044–1050.
- Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study // Gastroenterology. 1990; 98: 380–386.
- Johanson JF, Sonnenberg A. Constipation is not a risk factor for hemorrhoids: a case-control study of potential etiological agents // Am J Gastroenterol. 1994; 89: 1981–1986.
- Loder PB, Kamm MA, Nicholls RJ, Phillips RK Haemorrhoids: pathology, pathophysiology and aetiology // Br J Surg. 1994; 81:946–954.
- Pigot F., Siproudhis L., Allaert FA Risk factors associated with hemorrhoidal symptoms in specialized consultation // Gastroenterol Clin Biol. 2005; 29: 1270–1274.
- Aigner F., Gruber H., Conrad F., Eder J., Wedel T., Zelger B., Engelhardt V., Lametschwandtner A., Wienert V., Böhler U. et al. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease // Int J Colorectal Dis. 2009; 24: 105–113.
- Kaidar-Person O., Person B., Wexner SD Hemorrhoidal disease: A comprehensive review // J Am Coll Surg. 2007; 204: 102–117.
- Livzan M.A. Pain syndrome in gastroenterology - treatment algorithm // Medical advice. 2010, no. 3–4. P. 68.
- American Gastroenterological Association medical position statement: Diagnosis and treatment of hemorrhoids // Gastroenterology. 2004; 126:1461–1462.
- Acheson AG, Scholefield JH Management of haemorrhoids // BMJ. 2008; 336:380–383.
- Livzan M. A. Modern principles of treatment of constipation // Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2009. T. 19, No. 2. P. 70–74.
- Alonso-Coello P., Zhou Q., Martinez-Zapata MJ, Mills E., Heels-Ansdell D., Johanson JF, Guyatt G. Meta-analysis of flavonoids for the treatment of haemorrhoids // Br J Surg. 2006; 93:909–920.
M. A. Livzan, Doctor of Medical Sciences, Professor V. L. Poluektov, Doctor of Medical Sciences, Professor E. A. Lyalukova1, Candidate of Medical Sciences
State Budgetary Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation , Omsk
1 Contact information
Diagnosis of hemorrhoids
The patient's diagnostic examination plan should include:
- taking anamnesis;
- examination of the perianal area - you should pay attention to the condition of the skin, the presence of skin hyperemia, maceration, determine the degree of prolapse of hemorrhoids, the possibility of their self-reduction and the severity of bleeding;
- digital examination of the rectum - the presence of compacted hemorrhoids, polyps, anal papillae is determined, the functional state of the anal sphincter is assessed;
- clinical blood test - anemia and its severity are detected, as well as the manifestation of systemic inflammatory reactions;
- anoscopy - visually determines the condition of the internal hemorrhoids, the mucous membrane of the distal part of the rectum, the dentate line and the epithelium covering the anal canal;
- sigmoidoscopy - performed when colonoscopy is not possible and is intended to assess the condition of the mucous membrane of the rectum and distal part of the sigmoid colon;
- colonoscopy - performed to exclude other diseases of the colon that manifest similar symptoms.
Differential diagnosis
Polyps, villous tumors, cancer
Differential diagnosis should be made with sessile, non-moving broad-based polyps, polypoid formations (adenomas) and rectal cancer. Diagnosis of internal hemorrhoids not complicated by thrombosis, edema or prolapse is usually not difficult. Suspicion of rectal or anal cancer must be resolved through a mandatory biopsy and microscopic examination of the material obtained.
Hypertrophied anal papilla
If a dense formation is detected, the stem of which originates from the area of the dentate line, one should think about a hypertrophied anal papilla. An accurate diagnosis is made based on the results of anoscopy.
Rectal prolapse
Rectal prolapse can be partial (incomplete), affecting only the mucous layer of the intestinal wall, or complete, with prolapse of the entire thickness of the rectal wall. Incomplete prolapse may affect only part or the entire circumference of the rectum. Difficulties may arise in the differential diagnosis of prolapsed internal hemorrhoids and complete or incomplete rectal prolapse. It should be noted that internal hemorrhoids are formations that are not uniform in thickness and are separated by grooves, while with prolapse of the mucous membrane a cylindrical protrusion with clear boundaries is determined.
Can there be hemorrhoids without blood?
Often it is the appearance of blood in the stool that indicates the presence of a disease. In some cases, many other complaints are present, but there is no bleeding. Patients experience the following complaints:
- severe pain when going to the toilet;
- discomfort, foreign body sensation, itching.
There are cases when there is no obvious bleeding, but interspersed with bloody streaks are observed in the stool. If there is no blood, but pain and discomfort regularly bother you, the disease continues to develop. Prolapse of hemorrhoids without bleeding may also occur.
Other causes of similar symptoms
Many patients are interested in whether the presence of pain in the rectal area can signal other diseases. Pain, discomfort and swelling in the perianal area may indicate not only hemorrhoids, but also other pathologies:
- abrasions, ulcers, anal fissures;
- intestinal fistulas;
- parasites in the intestines;
- diseases of the endocrine glands;
- liver diseases.
Discomfort in the anus occurs due to non-compliance with personal hygiene rules and diaper rash.
Without timely treatment, hemorrhoidal disease continues to progress. Its course is getting worse. Consequences such as thrombosis and anal fissures develop. With these diseases, itching and swelling in the anus are always a concern. There is a risk of purulent inflammation of the intestines and infection of the anus.
What to do if there are signs of hemorrhoids?
Do you experience complaints typical of hemorrhoidal disease, but do not see any blood? You need to undergo diagnosis and treatment from a proctologist. The doctor will recommend a treatment course that will help get rid of the disease. If you consult a doctor early, hemorrhoids are treated much faster; conservative methods are effective. By contacting a proctologist in a timely manner, it will be possible to cure hemorrhoidal disease before it is complicated by bleeding.
There is no need to experiment and self-medicate. This will not only be a waste of money on expensive medications, but may also cause your health to worsen. Treatment of hemorrhoids is individual, therefore, for it to be effective, it must be prescribed by a doctor. On Clinic in Almaty employs qualified specialists. In the proctology department, for the convenience of patients, male and female proctologists diagnose and treat rectal diseases. Patients feel relief after the first visit to the doctor. Hemorrhoids after childbirth and during pregnancy are treated taking into account contraindications.
In the clinic, proctological diseases are treated with drug therapy and modern non-surgical methods.
Treatment Options for Internal Hemorrhoids
There are many ways to combat the disease. What will be optimal in a particular case can only be said by a doctor after a comprehensive examination of the patient. In the initial stages, conservative treatment also helps - painkillers, rectal suppositories, gels, ointments, creams, etc.
When the nodes are finally formed, minimally invasive methods of solving the problem are much more effective:
- Sclerotherapy. A sclerosing agent is injected into the affected node, gluing its walls.
- Laser vaporization, in which the nodes are “evaporated” under the thermal influence of the laser.
- Ligation. Using a vacuum ligator, a latex ring is placed on the hemorrhoidal node, which compresses the affected vessel, simultaneously depriving it of recharge.
- Disarterization. The problematic artery (and in some cases also a node) is sutured with a special thread.
- Milligan-Morgan operation. The hemorrhoid is removed and cut off using a laser, after which the affected area is sutured using a special thread.
In the final stages of internal hemorrhoids, surgical intervention is no longer necessary. In this case, doctors use hemorrhoidectomy and other options for excision of hemorrhoids.
Regardless of which treatment option is chosen, the patient is advised to follow a diet that helps normalize the functioning of the digestive tract.
To avoid all these unpleasant manipulations, it is necessary to regularly see a proctologist. Medical specialists are experts in their field. Make an appointment, and they will not only detect your illness in a timely manner, but will also select the optimal treatment option.
Causes of hemorrhoids without blood
The main causes of the disease are a sedentary lifestyle, intense physical activity, and poor nutrition. Stagnation of blood in the pelvis, excessive strain on the veins and frequent constipation predispose to the development of the disease.
Lack of blood at the initial stage of hemorrhoidal disease is a common occurrence. This happens because the hemorrhoids are inflamed, the veins are swollen due to stagnation of blood, but are not seriously damaged. In this case, bleeding does not occur. The pathological process becomes chronic. In the chronic form of hemorrhoids, exacerbations often occur. Signs of the disease intensify with alcohol abuse, during pregnancy and the postpartum period. Remissions in a chronic disease are accompanied only by discomfort.
With exacerbation of hemorrhoids, the likelihood of damage to hemorrhoids and adjacent vessels increases. Sooner or later the bleeding will make itself known. It should be noted that external hemorrhoids often occur without blood than internal hemorrhoids.
Reasons for the development of internal hemorrhoids
The root cause that causes the appearance of hemorrhoids is always the same - disturbances in blood flow in the vessels of the rectum. As a result of the lack of balance between inflow and outflow, blood accumulates in one place or another, stretching the walls of blood vessels and forming nodes. Of much greater interest are the reasons contributing to this very disturbance of blood flow. It could be:
- Excess weight.
- Problems with bowel movements (regular constipation or diarrhea).
- Increased pressure in the abdominal cavity.
- Poor nutrition, which consists of foods and drinks that irritate the mucous membranes of the rectum and colon.
- Blockage of the pelvic veins, the appearance of adhesions, tumors, etc. in this area.
- Dystrophy of the muscles and ligaments responsible for fixing the vessels of the hemorrhoidal plexus.
- Sedentary lifestyle.
- Various vascular pathologies, including atherosclerosis, varicose veins, etc.
- Prolonged hacking cough, often provoked by smoking.
- Severe straining during bowel movements.
- Difficult physical work, such as regularly lifting heavy loads.
If the above options occur to you from time to time, the risk of developing internal hemorrhoids is unlikely. However, if any of this has already become part of your lifestyle, it’s time to check with a proctologist.