Among all diseases of the gastrointestinal tract (GIT), the incidence of chronic pancreatitis ranges from 5.1 to 9%, and in the last few decades, the incidence of pancreatitis in our country has doubled1.
Chronic pancreatitis is an insidious disease, largely due to its recurrent nature. Patients are often concerned about periods of exacerbation, accompanied by severe pain, nausea, and vomiting.
Where does chronic pancreatitis come from? What causes the disease and is it possible to fight it? Let's try to figure it out.
Symptoms of chronic pancreatitis
Symptoms of chronic pancreatitis may vary depending on the stage (remission or exacerbation), course and physical condition of the patient. The main signs of the disease are as follows:
- acute pain without clear localization. Pain can be felt in the right hypochondrium, upper or middle abdomen and spread to the back. In many patients, pain occurs immediately after eating, especially if the diet contained fatty, smoked or spicy foods;
- frequent loose stools are one of the main signs of indigestion. Digestive problems in chronic pancreatitis are caused by a lack of enzymes;
- heaviness in the abdomen, nausea, which also indicate a lack of digestive enzymes;
- increasing feeling of hunger, muscle tremors, weakness, cold sweat;
- intoxication, manifested in fever, chronic fatigue, and a feeling of general malaise.
Symptoms
Clinical manifestations of the disease are associated not only with damage to the organ itself, but also with a violation of its secretory and endocrine functions. In acute pancreatitis, the symptoms are pronounced:
- Intense pain in the epigastric region, left hypochondrium, local or encircling, often radiating under the left shoulder blade. Unpleasant sensations intensify when lying down and after an error in diet.
- Increased salivation, belching, nausea, frequent vomiting, which does not bring relief.
- Increased body temperature. Fever and chills may occur.
- Changes in skin and mucous color. Moisture and pallor of the skin and moderate yellowing of the sclera are often observed. In rare cases, the skin also takes on a yellowish tint. There may be bluish spots on the body and hemorrhages in the navel area.
- Dyspeptic symptoms – bloating, heartburn.
- Irritability, tearfulness, and in severe cases pancreatogenic psychosis develops.
Chronic pancreatitis is characterized by periods of exacerbation and remission and has a staged course.
In the preclinical stage, there are no symptoms of the disease; changes in the pancreas become an accidental finding during an ultrasound of the abdominal organs. During the period of initial manifestations, multiple episodes of exacerbation of pancreatitis are observed with manifestations characteristic of the acute form of the disease. Gradually, their frequency becomes lower, but symptoms persist during the interictal period: abdominal pain, occasional vomiting, nausea, diarrhea, flatulence. At the stage of persistent symptoms, there is pain in the upper half of the abdomen, often of a girdling nature. The patient loses weight, in particular due to refusal to eat due to fear of increased pain. Manifestations of secretory and endocrine insufficiency, such as indigestion and hyperglycemia, intensify.
Subsequently, pancreatic atrophy occurs. The pain may become less intense or absent, and the frequency of attacks of pancreatitis is reduced. The feces become mushy, foul-smelling, and greasy. Exhaustion is observed, and pancreatogenic diabetes mellitus develops. In the last stage, systemic complications arise, and malignant degeneration of the tissue of the affected organ is possible.
Causes of chronic pancreatitis
One of the most common causes of chronic pancreatitis is poor diet and unhealthy lifestyle. Constant overeating, abuse of fatty foods and alcohol cause blockage of the excretory ducts of the pancreas.
Narrowed excretory ducts provoke the accumulation and premature activation of digestive enzymes. As a result, the pancreas actually begins to digest itself, and inflammation forms1.
In addition, the following factors can lead to chronic pancreatitis3:
- ulcer of the duodenum, stomach and enteritis. Chronic inflammation of the mucous membrane of the gastrointestinal tract makes it difficult to secrete pancreatic juice, which often causes chronic pancreatitis;
- cholelithiasis. After leaving the gallbladder, the stone causes blockage of the common duct and inflammation of the pancreas develops;
- genetic predisposition;
- toxic effects of drugs.
Epidemiology
The content of the article
According to recent studies, every 34 out of 100 thousand people develop pancreatitis every year, and due to the increasing prevalence of the main etiological risk factors - obesity, alcoholism, smoking, stone formation, the disease is diagnosed in younger people. Also, such statistics are associated with improved diagnosis and identification of less common causes of pancreatitis.
An independent risk factor for AP is smoking. This habit worsens alcohol-related damage to the pancreas.
Risk factor for pancreatitis is smoking
Most patients have mild pancreatitis; in 20-30% of cases, severe pancreatitis occurs. The mortality rate from severe pancreatitis is about 15%.
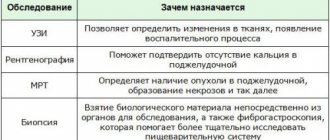
Diagnosis of chronic pancreatitis
Identifying chronic pancreatitis can be difficult due to the nonspecific clinical picture. Nausea, abdominal pain, digestive problems - these symptoms are characteristic of many diseases, for example, stomach ulcers or chronic cholecystitis. Therefore, identifying the disease may require a whole range of studies. Diagnosis of chronic pancreatitis may include2,3:
- external examination of the patient. Chronic pancreatitis may be indicated by bluish areas of the skin on the front and side walls of the abdomen. In some patients, bright red patches of skin on the chest and back become noticeable. Palpation may reveal pain in the left hypochondrium and the upper third of the abdomen;
- a general and detailed blood test, which shows the presence of an inflammatory process, based on an increase in the concentration of leukocytes;
- laboratory blood test to identify markers of nutritional status;
- fecal elastase test;
- ultrasonography. In some cases, ultrasound examination (ultrasound) can be performed through the walls of the stomach and duodenum, which significantly increases the accuracy of the examination. This method is called endoUS and combines the possibility of endoscopic and ultrasound diagnostics of the gastrointestinal tract (GIT);
- computed tomography: used to determine complications of pancreatitis associated with thickening of the pancreas tissue.
What is pancreatitis
Pancreatitis is inflammation of the pancreas. This organ secretes enzymes into the duodenum (just behind the stomach) that help food digest, such as amylase (to break down carbohydrates) and lipase (to break down fats). With severe inflammation of the pancreas - acute pancreatitis - its cells are destroyed and enzymes enter the blood. Therefore, for any severe abdominal pain, doctors determine the level of amylase in the blood.
Acute pancreatitis is a painful and very dangerous disease. Its symptoms are almost impossible to endure “on your feet”: it is a severe, persistent pain in the pit of the stomach and under the left rib, which often radiates to the back (so-called girdling pain occurs). A person with acute pancreatitis often even takes a special position on the bed - lying on his left side, so as not to increase the pain by moving the ribs when breathing. Most people with acute pancreatitis experience severe nausea and vomiting; any food intake increases the pain: after all, the pancreas begins to secrete enzymes when eating, and this increases blood flow, and therefore pain. Many people's body temperature rises.
Diagnosis of acute pancreatitis is the job not so much of gastroenterologists as of surgeons, since the intensity of pain can be the same as with appendicitis and other “surgical” pathologies.
Exacerbation of chronic pancreatitis
Chronic pancreatitis may hardly manifest itself until the period of exacerbation. Relapse of the disease is usually associated with two main reasons3:
- alcohol consumption. Even a small amount of alcohol consumed can provoke the transition of the disease into the acute phase;
- violation of the diet, overeating, a large number of fatty, fried, spicy dishes on the menu.
Other factors can also provoke exacerbation of chronic pancreatitis in adults, for example, chronic stress, physical fatigue, poisoning or the toxic effects of certain medications3.
Exacerbation of the disease is manifested by the following symptoms3:
- attack of acute or dull pain in the hypochondrium. Painful sensations spread to the subscapular region or the entire back;
- progressive diarrhea. In this case, the feces have a characteristic greasy shine. Undigested food remains are often observed in the stool;
- the occurrence of specific bitterness in the oral cavity, nausea and loss of appetite;
- whitish coating on the surface of the tongue;
- weight loss.
Exacerbation of chronic pancreatitis in adults can last for one to two weeks. You cannot fight the disease on your own during this period: the best solution is hospitalization and constant monitoring by specialists.
Treatment of chronic pancreatitis
The answer to the question “how to cure chronic pancreatitis” remains open even for modern doctors. The treatment regimen is determined by the doctor for each individual case. The main thing is that therapy should be comprehensive, affecting the main cause of the disease.
Treatment of chronic pancreatitis includes2,3,4:
- immediate cessation of bad habits. Smoking and abuse of strong alcoholic beverages aggravate the inflammatory process and contribute to the subsequent development of the disease;
- strict adherence to the diet. The daily diet should contain high-calorie foods, without spicy foods, salt and pure sugar. You should eat food often, in small portions. In case of exacerbation of chronic pancreatitis, therapeutic fasting is prescribed, which will help stop pancreatic secretion and relieve pain. After 1-3 “hungry” days, the patient is transferred to a special diet;
- basic therapy. In this case, we are talking about taking the following type of drugs: antispasmodics and analgesics, antisecretory and detoxification drugs. Treatment is carried out under the supervision of a doctor with strict adherence to the instructions;
- taking enzyme preparations, the task of which is to compensate for the impaired functioning of the pancreas. The fact is that the pancreas does not recover (it is not the liver), and therefore will no longer be able to work at full capacity during chronic pancreatitis. That is why the first line of therapy is enzyme preparations, which should be taken for life. An example of an enzyme drug prescribed for chronic pancreatitis is Creon®;
- complex therapy. May include taking antispasmodics or analgesics, antisecretory and detoxification medications. Therapy is carried out under the supervision of a physician with strict adherence to the instructions;
- taking anti-inflammatory and painkillers that improve the patient’s well-being;
- herbal medicine, which can be prescribed during remission only as prescribed by a doctor.
What to do if an exacerbation of pancreatitis occurs suddenly, and the ambulance has not yet arrived? Before the doctors arrive, you need to lie down, try to relax your abdominal muscles as much as possible and apply a heating pad with cold water to the sore spot. You should not take painkillers or any other medications - this will interfere with correct diagnosis. And, of course, any food and drinks, even plain water, are strictly prohibited, because any food or liquid can cause increased pain3.
Nutrition for pancreatitis
Nutrition for pancreatitis is selected in order to avoid nutritional deficiencies, prevent the onset of diabetes and other metabolic syndromes (high levels of low-density cholesterol, diabetes, hypertension), and reduce the frequency of attacks of pancreatitis. It is recommended to consume a sufficient amount of protein and carbohydrates, a minimum amount of fat (up to 60 g per day). It is better to bake, boil or steam food for pancreatitis.
The diet for acute pancreatitis should include foods that are easily digestible and do not cause irritation: fresh fruits and vegetables, plant-based milk, low-fat dairy products, rice, tofu, whole grain bread and cereals. A diet for chronic pancreatitis involves eating low-fat foods, fruits, vegetables (with pancreatitis you can eat tomatoes, cucumbers, carrots, cabbage), and whole grain cereals. For pancreatitis, you can use both fresh and frozen vegetables.
The drug Creon® 25000 for chronic pancreatitis
Find out more
Decreased pancreatic function inevitably leads to a lack of digestive enzymes in the body, so-called enzyme deficiency. As a result, the quality of digestion suffers, and the body does not receive the necessary energy and nutrients for full functioning. Creon® is designed specifically to compensate for the lack of its own enzymes through their delivery from the outside and belongs to the group of enzyme preparations. The drug contains enzymes identical to those produced by the pancreas. The key feature is that the active ingredient Creon® is small particles - minimicrospheres, which are collected in a capsule. The fact is that science has been studying enzyme preparations for more than 100 years in order to increase their effectiveness. To date, scientific advances indicate that preparations with particles whose size does not exceed 2 mm4.5 can most accurately recreate the natural process of digestion. Moreover, it has been scientifically proven that the smaller the particles of the drug, the more effective it can be4,6.
Creon® is the only drug whose capsule contains hundreds of small particles - minimicrospheres7. Their size does not exceed 2 mm, which is recorded as recommended in world and Russian scientific works4,5,6.
Pancreatitis in children
In young children, pancreatitis is usually a consequence of congenital malformations of the digestive system or enzyme deficiency. It can also be a complication of mumps (mumps). In older children, the development of the disease may be associated with poor nutrition (including abuse of sweets and carbonated drinks) or caused by intestinal parasites.
Children are often unable to clearly formulate their complaints, what and how they hurt. Therefore, at the first signs of the disease (the child’s complaints of abdominal pain, nausea, vomiting, unstable stool with impurities of undigested food), you should immediately consult a doctor. Infants with pancreatitis cry hysterically and quickly lose weight. Their tummy is swollen.
It is necessary to diagnose the disease promptly and begin treatment to prevent loss of the pancreas.
More information about pancreatitis in children
What else is important to know about enzyme preparations?
The minimum starting dosage is Creon® 25,000 units, which is stated in Russian recommendations for the treatment of chronic pancreatitis and exocrine pancreatic insufficiency2,5. The number indicates the amount of the enzyme lipase, which helps digest fats. If necessary, the doctor can increase the dosage; in European practice, the required dose per single dose can reach up to 80,000 units8. By comparison, the pancreas of a healthy person produces up to 720,000 of these units during each meal9.
Therapy should be taken seriously, since high-quality “nutrition” of the body is the key to its functioning. How long can a person live without energy from food? With chronic pancreatitis, the body must be supplied with enzymes at every meal, even with a snack. Thus, in accordance with the instructions for the drug Creon®, a full dose is required for a meal (for example, 25,000 units), and half for a snack. Creon® capsules are convenient to use: you can open them and add minimicrospheres to food, thereby selecting the desired dose10. More information about the admission rules can be found here.
Diagnosis of the disease
Diagnosis is carried out only in a clinical setting - the patient initially consults a therapist. During the examination, the doctor clarifies the complaints and prescribes a number of procedures:
- blood test (general and biochemical);
- Analysis of urine;
- stool analysis with determination of fat content;
- radiology diagnostics;
- linked immunosorbent assay;
- collection of pancreatic secretions through a probe (inserted directly through the esophagus);
- secretin-pancreozymin test;
- Lund's method eliminates the insertion of a probe, but is not as effective and is therefore used much less frequently.