The low FODMAP diet is designed for people suffering from symptoms of common intestinal diseases. As stated, if you follow a special diet and diet, constipation goes away, bloating, abdominal pain, and diarrhea do not bother you. Initially, the diet was offered to those suffering from irritable bowel syndrome. But, according to observations, those who are diagnosed with inflammatory bowel diseases can also feel the result.
What is IBS?
How often do you wake up feeling bloated and at the end of the day find that your clothes are tight around your stomach? This is actually quite normal, but what if your belly is bloated every day and these episodes happen so often that they negatively impact your daily life?
Quite often, the cause of these sensations is irritable bowel syndrome, a condition that is twice as common in women as in men. If you're someone who already experiences IBS, you know that it can be stressful, uncomfortable, and at times embarrassing.
This syndrome is the most common cause of bloating, with up to 90% of IBS patients reporting bloating. It occurs when your normally regular bowel movements turn into cramps. In addition to bloating, symptoms also include:
- abdominal pain,
- discomfort,
- severe flatulence,
- diarrhea,
- constipation.
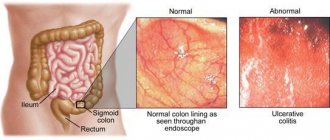
IBS is a functional disorder, meaning it causes changes in your bowel function, but it is not associated with ulcers, inflammation or any abnormal blood tests. This means that a test like a colonoscopy and an x-ray will most likely show no abnormalities.
Because the symptoms of irritable bowel syndrome are common to a number of other bowel disorders, the condition is usually diagnosed through a process of exclusion, meaning that diagnosing the problem can take a long time.
What happens when you eat them?
Most FODMAPs pass through most of your intestines unchanged. They are completely resistant to digestion and fall under the category of dietary fiber.
But some carbohydrates only function as FODMAPs in some people. These include lactose and fructose.
General sensitivity to these carbohydrates also varies from person to person. In fact, scientists believe they contribute to digestive problems like IBS.
When FODMAPs reach the colon, they are fermented and used by gut bacteria as an energy source.
The same thing happens when dietary fiber feeds your friendly gut bacteria, leading to various health benefits.
However, friendly bacteria tend to produce methane, while bacteria that feed on FODMAPs produce hydrogen, another type of gas that can lead to gas, bloating, stomach cramps, pain, and constipation ().
Many of these symptoms are caused by intestinal enlargement, which can also make your belly appear larger ().
FODMAPs are also osmotically active, meaning they can pull water into your intestines and promote diarrhea.
Summary:
FODMAPs are poorly absorbed in some people's bodies, causing them to reach the colon. They draw water into the intestines and are fermented by intestinal bacteria, producing hydrogen.
Causes of the syndrome
The exact cause of IBS is still unknown, but there are many possible triggers. High levels of stress or infection by a parasite or virus are two common causes.
Genetics and an abnormal balance of gut bacteria are also thought to contribute.
Food also plays a role. People with IBS often find that certain foods trigger their symptoms, and it's important to know which foods are safe to eat and which are not.
A group of foods called FODMAPs are the most common dietary trigger—and scientific research has proven that a diet low in FODMAPs can significantly improve the symptoms of irritable bowel syndrome for many people.
What is FODMAP
FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, polyols, which are short-chain carbohydrates (sugars) that are poorly absorbed in the small intestine.
F ermentable - fermentable, O ligosaccharides - oligosaccharides, D isaccharides - disaccharides, Monosaccharides - monosaccharides A nd - and P olyols - polyols.
Some people experience digestive upset after consuming them.
Important ! The FODMAP diet doesn't involve fasting or any other crazy indulgences, but it can still be dangerous for some, according to nutrition experts.
It's worth noting right away that FODMAP foods are a natural part of many healthy diets. Because they are poorly digested, they end up in the colon and act as “food” for your gut bacteria, which then release a lot of gas.
People with IBS have more sensitive nerve endings in their digestive system, so this gas may cause discomfort. The effects of FODMAPs are cumulative—what you eat throughout the day or week matters.
Simply put, a FODMAP diet is a diet that reduces the intake of certain carbohydrates that are difficult to digest. These carbohydrates provide food for intestinal bacteria.
Additionally, many high FODMAP foods also contain lots of prebiotics, which provide food for the beneficial bacteria found in your gut. Research shows that long-term avoidance of FODMAP foods can affect your bacteria balance and gut health.
Instead of overhauling your diet, think of the low FODMAP diet as a short-term event that will help you identify your specific IBS triggers.
Typically, the low FODMAP diet lasts for 2 to 6 weeks , as long as your gut symptoms calm down. Gradually, the FODMAP groups are then reintroduced one by one and symptoms are monitored until you know which foods to include and which to limit or eliminate.
What to do if diet doesn't help
A low FODMAP diet does not always help with irritable bowel syndrome. It fails 30% of the time, but before you give up, check the following:
- If the pain does not go away, make sure that you do not eat foods with prohibited ingredients. When buying ready-made or semi-finished food, people do not notice harmful ingredients. And the recipes include garlic, onions, artificial sweeteners sorbitol or xylitol: a small amount is enough to aggravate the disease.
- Make sure you use the FoodMaestro app, developed by the folks at King's College London, or Monash University's FODMAP diet option. Check if you have translated the name of your menu component correctly.
It is not recommended to follow the diet without consulting a gastroenterologist. Unlike nutrition systems aimed at losing excess weight, a therapeutic menu requires a more serious approach. It is not enough to simply take a list of permitted and prohibited dishes: the diet is compiled individually in each specific case. Without medical supervision, you risk depriving yourself of important nutrients, and their lack will affect your health.
What to do if the gastroenterologist has not heard of the diet? The developments are relatively new, and not every physician follows the information. But more and more gastroenterologists are learning about a diet low in short-chain carbohydrates. Consult several specialists and you will find a competent one.
The Low-FODMAP diet can dramatically improve the condition of people with gastrointestinal diseases, as confirmed by Dr. Megan Rossi. But the diet is effective in 70-76% of cases, and requires the supervision of a qualified physician. The Low-FODMAP nutrition system includes 3 stages, and their total length takes up to 6 months.
Megan Rossi reminds you that unless you have a medical condition, the diet may do more harm than good. It helps to reduce body weight because it involves giving up flour. But the power system is aimed at solving a specific problem. Healthy people may have complaints about the functioning of the gastrointestinal tract, since they will not receive prebiotics - food components that are fermented by the microflora of the large intestine and stimulate its growth. But with an appropriate diagnosis, the diet improves the overall quality of life.
Is the FODMAP diet backed by science?
Yes.
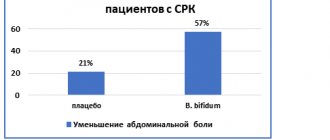
The low FODMAP diet was developed by doctors and nutritionists at Monash University in Australia. Clinical trials on people with irritable bowel syndrome (IBS) have shown that it helps IBS sufferers reduce symptoms in 75% of patients.
This diet limits or eliminates foods that contain FODMAPs and is now accepted worldwide as the first line of dietary therapy for irritable bowel syndrome. However, being too restrictive can make it difficult to meet your nutritional needs.
Diagnostic features
3 things to do if you suspect IBS:
- Don't self-diagnose . Many conditions, such as diverticulitis or celiac disease, can cause similar symptoms, so it is important to see your GP and possibly a gastroenterologist for a thorough assessment. Most importantly, do not ignore your symptoms and do not hope that they will disappear on their own.
- Contact a nutritionist . Avoiding foods without consulting a professional can also make diagnosis more difficult. If you suspect food is the culprit, take the time to see an accredited dietitian, as you may be eating more than you need and missing out on valuable nutrients.
- Consider your stress level . Stress can make IBS symptoms worse, so try to reduce stress with things like yoga, a warm bath at the end of the day, or reading your favorite book. Try to also get enough sleep and exercise.
How does the low FODMAP diet work?
Low FODMAP is a three-step elimination diet:
- First, you stop eating certain foods (high FODMAP foods).
- Then you slowly reintroduce them to see which ones are causing concern.
- Once you identify the foods that cause your symptoms, you can avoid or limit them without worrying about everything else.
We recommend sticking to the elimination portion of the diet for 2-6 weeks . This will reduce symptoms and help reduce abnormally high levels of gut bacteria.
Then every 3 days you can add high FODMAP foods to your diet, one at a time, to see if it causes any symptoms. If a particular high FODMAP food causes symptoms, then avoid it long-term.
Is it easy to follow a diet?
Following a diet is not difficult if you create a balanced menu. Problems arise in determining which foods are allowed, especially if you buy convenience foods or store-bought products. After all, it is impossible to make a list of all the foods available in supermarkets and calculate the FODMAP levels.
There are applications on the Internet that allow you to scan a barcode, but they are not adapted for residents of the Russian Federation. Products on shelves in Russian, Australian and American stores differ, so the database is incomplete. There are many sources on the Internet that do not always provide accurate information. To determine the safety of ingredients, consult your physician.
FODMAP products
Common FODMAP foods that include fructans :
1. Vegetables:
- artichoke;
- asparagus;
- beetroot;
- broccoli;
- garlic;
- leek;
- onion;
- cabbage;
- Shallot
2. Cereals
- bran (wheat, rye or barley);
- wheat noodles.
3. Fruit
- apple;
- dried fruits;
- grapefruit;
- persimmon;
- grenades;
- watermelons.
4. Nuts:
- cashew nuts;
- pistachios.
5. Legumes:
- baked beans;
- chickpeas;
- lentils.
Common FODMAP foods that include lactose :
- condensed milk;
- cow's milk;
- custard;
- goat milk;
- ice cream;
- sheep's milk;
- yogurt;
- cheese;
- cottage cheese.
Common FODMAP foods that contain a lot of fructose :
- apple;
- fruit juices;
- figs;
- mango;
- pear;
- watermelon;
- corn syrup;
- concentrated fruit products;
- honey.
Common FODMAP foods that include polyols:
- avocado;
- cauliflower;
- mushrooms;
- sweet corn;
- apple;
- apricot;
- blackberry;
- cherries;
- rambutan;
- nectarine;
- peach;
- pear;
- plum;
- prunes;
- watermelon;
- sweeteners: isomalt (E953), maltitol (E965), mannitol (E421), sorbitol (E420), xylitol (E967).
Foods Suitable for a Low FODMAP Diet
1. Fruits:
- banana;
- blueberry;
- grape;
- melon;
- kiwi;
- lemon;
- lime;
- mandarin;
- passion fruit;
- papaya;
- orange;
- raspberries;
- strawberry;
- tangelo.
2. Vegetables:
- salad;
- celery;
- broccoli;
- Brussels sprouts;
- Bell pepper;
- cabbage (regular);
- carrot;
- chilli;
- corn;
- cucumber;
- eggplant;
- green bean;
- parsnip;
- potato;
- pumpkin;
- spinach;
- green onions (exclusively green part);
- tomato;
- zucchini.
3. Dairy products:
- milk;
- lactose-free milk;
- rice milk;
- feta cheese;
- hard cheese;
- brie;
- Camembert;
- feta;
- ice cream substitutes;
- gelati;
- sherbet;
- oil substitutes.
4. Cereal products:
- flakes;
- gluten-free bread and pasta;
- rice;
- corn;
- oats (less than ½ cup);
- polenta;
- quinoa.
5. Sweeteners:
- sugar;
- glucose;
- artificial sweeteners that do not end in "-ol"
- stevia;
- golden syrup;
- maple syrup;
- rice malt syrup.
Try these simple alternative foods to relieve bloating:
- Replace regular bread with gluten-free bread.
- Swap oats for quinoa.
- Replace the couscous with rice.
- Replace milk with lactose-free milk.
- Replace mango with pineapple.
- Replace dried lentils with canned lentils.
- Replace the onions with green onions.
Note ! Onions are one of the main foods that cause IBS symptoms. Even in very small quantities, this vegetable can cause discomfort.
It is worth noting that fructans can transfer from onions to other ingredients during cooking. Garlic also contains fructans, but most people can generally tolerate small amounts of garlic.
A good way to enjoy the flavor of garlic and onions without the fructans is to use their oil.
What diet will help with irritable bowel syndrome?
There are many diseases (eg, inflammatory bowel disease, celiac disease, lactose or fructose intolerance, microscopic colitis, intestinal cancer) that have symptoms similar to irritable bowel syndrome, so before treating this disease and trying to follow a specific diet , it is necessary to accurately diagnose it.
You can make an appointment at the Expert Center for examination and diagnosis of irritable bowel syndrome by phone. 426-33-88.
At the moment, there is no universal diet that would suit all patients with irritable bowel syndrome. However, many IBS patients attribute the exacerbation of their symptoms to eating certain foods, and following a diet that eliminates these foods helps them alleviate the disease.
Because diets are not universal, often what works for one person may not work for another. The dietary changes that are right for you will depend on your individual symptoms and reactions to certain foods.
A food journal can help you identify foods that reduce or worsen your symptoms. We recommend keeping track of the foods you eat, the symptoms you experience, and how long after eating these symptoms occur.
According to recent scientific research, foods and drinks that worsen the condition of people with irritable bowel syndrome include:
- foods high in fat;
- some dairy products;
- alcoholic drinks;
- caffeine;
- drinks high in artificial sweeteners;
- beans, cabbage and other foods that cause increased gas formation.
The International Foundation for Functional Gastrointestinal Disorders also identifies insoluble fiber, chocolate and nuts as foods that may cause problems in some people with IBS.
Eating fiber for IBS
Increasing your fiber intake may improve symptoms of constipation-predominant irritable bowel syndrome in some cases, but be aware that insoluble fiber may increase bloating, flatulence, and cramping, especially if the increase is not gradual. Soluble fiber is well tolerated, so for irritable bowel syndrome with constipation, a dietary supplement is used - psyllium, obtained from plantain seeds.
Foods containing fiber include fruits, vegetables, cereals, and whole grains. For adults, 22 to 34 grams of fiber is recommended each day. When adding fiber to your diet, it is recommended to increase the amount little by little, by 2 - 3 grams per day. Adding too much fiber at one time can cause gas and bloating and make you feel even more abdominal discomfort.
Low FODMAP Diet
The low FODMAP diet is currently a well-known treatment for patients with irritable bowel syndrome (IBS), but the diet is controversial, difficult to follow, and not all IBS patients respond positively to this treatment. Recent scientific research has shown that this diet significantly reduced IBS symptoms in about half of the people who tried it. The success of the diet depends on individual tolerance to foods and the composition of the intestinal microbiota. To find out if a low FODMAP diet is right for you, you should consult a gastroenterologist.
You can make an appointment with a gastroenterologist specializing in the treatment of intestinal diseases at the Expert GC by tel. 426-33-88.
FODMAP substances are oligosaccharides, disaccharides, monosaccharides and polyols (FODMAPs - Fermentable, Oligo, Di, Mono and Polyol), which some people do not have enough digestive enzymes to break down. These are types of carbohydrates that are poorly absorbed in the small intestine and, if not broken down, cause fermentation in the large intestine. They reach the colon undigested and are broken down by intestinal bacteria. During the fermentation process, gas is released and this can cause discomfort and unpleasant symptoms for those who suffer from irritable bowel syndrome, such as gas, diarrhea or bloating.
There are four groups of FODMAP substances:
- Oligosaccharides (fructans and galactans) including wheat, rye, onions, broccoli, garlic, chickpeas, lentils, soy products and beans.
- Disaccharides (lactose) including cow's milk, ice cream, yogurt and cottage cheese.
- Monosaccharides (fructose) including apples, mangoes, pears, watermelon and honey.
- Polyols including sorbitol, mannitol, and xylitol, including nectarines, peaches, plums, cauliflower, and mushrooms.
Researchers suggest that FODMAP substances entering the small intestine increase the amount of water it contains, which may contribute to loose stools and diarrhea in IBS. Then these substances, unbroken, enter the large intestine, where billions of bacteria ferment them, which leads to the formation of gases and bloating. Therefore, reducing the intake of FODMAP substances may improve symptoms of bloating and diarrhea in some patients with irritable bowel syndrome.
Because fructans (oligosaccharides) are found in many foods that also contain gluten, such as pasta and white bread, it has long been thought that patients with irritable bowel syndrome should follow a gluten-free diet. A new study published in the American Journal of Gastroenterology shows that in a group of people with IBS who thought they were reacting to gluten, fructan caused more gastrointestinal distress than gluten. Laboratory studies have shown that wheat and other gluten-containing grains (such as rye, barley, wheat) also contain significant amounts of fructans. It turns out that fructans and gluten commonly coexist in food, and gluten-free grain products tend to be low in FODMAPs.
Some people have symptoms caused by one or two FODMAPs, while others have problems with all five. Foods with FODMAP substances should only be limited if they contribute to IBS symptoms.
How to replace high FODMAP foods?
Vegetables
High FODMAP Foods
Asparagus, artichokes, onions (any), leeks in bulbs, garlic, onion and garlic salt, beets, celery, savoy cabbage, broccoli, Brussels sprouts, white cabbage, dill.
Low FODMAP Alternatives
Bell peppers, carrots, green onions, fresh herbs, cucumbers, lettuce, tomatoes, zucchini, Chinese cabbage, celery, corn, eggplant, lettuce, pumpkin, bamboo shoots.
Legumes and mushrooms
High FODMAP
Green peas, baked beans, chickpeas, lentils, red beans, peas, green beans, any mushrooms.
Low FODMAP
Bean sprouts, green beans, green beans,
Fruits
High FODMAP
Apples, pears, mangoes, watermelons, nectarines, peaches, plums, persimmons, apricots, avocados, cherries, nectarines, prunes, canned fruits in their own juice, large portions of fruits, dried fruits, fruit juice, concentrated fruit plum sauces.
Low FODMAP
Bananas, oranges, tangerines, grapes, melon, grapefruit, kiwi, lemon, lime, orange, passion fruit, papaya.
Milk and dairy products
High FODMAP
Regular and low-fat cow's and goat's milk, yogurt, soft cheese, cream, custard, ice cream based on whole milk and cream.
Cheeses: soft, creamy with high fat content, mozzarella, Adyghe, Suluguni
Low FODMAP
Lactose-free or soy milk, lactose-free yogurt, hard cheese. Ice cream substitutes: frozen juices, sorbet.
Bread, cereal, biscuits, cookies and snacks
High FODMAP
Rye and wheat bread, wheat flakes with dried fruits, wheat pasta, rye and wheat cereals, cookies, crackers, wheat and rye biscuits/
Low FODMAP
Gluten-free bread and spelled sourdough bread, nuts, gluten-free pasta, quinoa.
Gluten-free biscuits, rice cakes/pies, cornbread.
Sweets
High FODMAP
Honey and honey products, sweeteners: isomaltitol, maltitol, mannitol, sorbitol, xylitol and other sweeteners ending in “-ol”.
Low FODMAP
Glucose, sugar (sucrose), other artificial sweeteners not ending with “-ol”
Nuts and seeds
High FODMAP
Cashews, pistachios
Low FODMAP
Almonds (<10 nuts), pumpkin seeds
It is not necessary to completely eliminate all foods high in FODMAP carbohydrates. Consulting a nutritionist can help you eliminate high FODMAP foods from your diet and then reintroduce them little by little to find your tolerance level.
You can make an appointment with a nutritionist specializing in therapeutic nutrition at the Expert State Center by phone. 426-33-88.
What is the end result?
It is important to understand ! The foods that cause symptoms vary from person to person.
To relieve IBS symptoms, it is important to avoid high FODMAP foods that irritate the gut, including:
- Dairy-based milk, yogurt and ice cream
- Wheat-based products such as cereals, breads and crackers
- Beans and lentils
- Some vegetables such as artichokes, asparagus, onions and garlic
- Some fruits such as apples, cherries, pears and peaches
Instead, base your nutrition on low FODMAP foods such as:
- Eggs and meat
- Certain cheeses such as brie, camembert, cheddar and feta
- Almond milk
- Grains such as rice, quinoa and oats
- Vegetables such as eggplants, potatoes, tomatoes, cucumbers and zucchini
- Fruits such as grapes, oranges, strawberries, blueberries and pineapple
Ask your doctor or dietitian for a complete list of healthy FODMAP foods.
A FODMAP diet for life?
No, the goal of the low FODMAP diet is to help your gut heal and reintroduce certain foods into your diet over a period of time.
Ideally, a low FODMAP diet should be followed for 2-6 weeks .
After an initial low FODMAP diet, people can return to their normal eating habits and only need to avoid very specific high FODMAP foods.
Duration of compliance
The duration of adherence to this diet may vary for each patient depending on the course of his disease . On average, it takes from 3-4 to 8-14 weeks to stabilize the condition, but the specific time period will depend on the patient’s medical history, the severity of intestinal damage, concomitant diseases and conditions.
In order for the effect to occur faster, it is important to follow all the doctor’s recommendations, take the prescribed therapy and eat often, but little by little. Ideally, you should eat 5-6 times a day in small portions. The break between meals should be about 3.5-4 hours. This will contribute to a complete digestion process and a speedy recovery (entering the remission phase).