What can you do on a diet after gallbladder removal for adults?
After cholecystectomy, it is necessary to remember that it is especially important for the body to receive complete and balanced nutrition in order to adapt to the absence of the gallbladder. In the first days after surgery, the restrictions are quite strict, but further recovery will not cause you any serious difficulties2.
Your diet should be balanced in a ratio of 1:1:2. This means that approximately ¼ of your diet should come from high-quality vegetable fats and complete proteins, and half should be given to complex carbohydrates. The diet after cholecystectomy is based on diet No. 5, intended for people with diseases of the liver and biliary tract.
List of permitted products:
| Vegetables | carrots, cauliflower, broccoli, pumpkin, beets, boiled potatoes, leafy greens, cucumbers |
| Fruits | bananas, pears, sweet apples, apricots and peaches |
| Nuts and dried fruits | almonds, walnuts, cashews, raisins and dried apricots |
| Meat | dietary veal, rabbit, turkey and chicken meat |
| Low-fat fish | pollock, hake, pike perch |
| Soups | soups cooked with a second broth, vegetable soups; |
| Porridge | crumbly and semi-viscous from buckwheat, rice and oatmeal; |
| Seafood | up to 3 times a week |
| Bread | whole grain and with bran - just not fresh, crackers, biscuits, bread, crackers |
| Dairy products | cottage cheese, fermented baked milk, kefir, yogurt, low-fat and unsalted cheeses |
| Oil | creamy - up to 30 grams and all types of vegetable - up to 15 grams per day |
| Beverages | still water, tea, weak coffee, herbal infusions, jelly, fruit juice and compote |
Material and methods
The study is based on an analysis of the results of surgical treatment of 431 patients with stomach cancer who were treated at the Oncology Clinic named after. V.M. Efetov and at the Crimean State Medical University named after. S.I. Georgievsky from 2006 to 2013. Among the patients there were 246 (57.1%) men and 185 (42.9%) women aged from 25 to 82 years (mean age 60.2±7.9 years). In accordance with the results of a morphological study of surgical material, 410 (95.1%) patients were diagnosed with gastric cancer, 16 (3.7%) with gastric lymphoma and 5 (1.2%) with gastrointestinal stromal tumor. More often - in 252 (58.5%) patients - the tumor was localized in the body of the stomach, in 118 (27.4%) patients - in the proximal stomach, less often - in 61 (14.1%) patients - in the antrum of the stomach. In 308 (71.5%) patients the tumor had endophytic or mixed growth and in 123 (28.5%) patients it had exophytic growth, and therefore for this category of patients gastrectomy was the main type of surgical intervention.
Based on the requirements of the seventh edition of the international classification of malignant neoplasms TNM (2009), stage I gastric cancer was diagnosed in 73 (16.9%) patients, stage II - in 98 (22.7%), stage III - in 213 ( 49.4%), stage IV - in 47 (10.9%) patients. In this regard, 308 (71.5%) patients were operated on for locally advanced gastric cancer (pT3-pT4), in 200 (46.4%) cases multivisceral resection was performed with additional removal or resection of organs adjacent to the stomach: in 126 (29.3%) observations - two, 51 (11.8%) - three, 17 (3.9%) - four and 6 (1.4%) observations - five. In 384 (89.1%) patients, the nature of the operations performed corresponded to the volume R0 (radical operations), in 47 (10.9%) patients - to the volume R1−2 (palliative).
At the reconstructive stage after gastrectomy, a fundamentally new technique was developed for creating a food reservoir in the initial section of the jejunum, which participates in the formation of the esophageal-intestinal anastomosis both in the loop version of the reconstruction of the digestive tract (Ukrainian Patent No. 50085 dated 05.25.10) and in reconstruction on the isolated and transected intestine according to Ru (Patent of Ukraine No. 75880 dated 12/10/12). After this, all patients scheduled for gastrectomy were divided into two comparable representative groups. Separation into groups was carried out in a blind manner using envelopes that included recommendations on the method of reconstruction of the digestive tract. In accordance with this, the main group, which included gastrectomy with the creation of a food reservoir, included 146 patients, and the control group (gastrectomy using the traditional method of reconstruction of the digestive tract) included 285 patients. Considering that the formation of the groups was carried out using the method of blind distribution, the comparability of the groups was established before treatment, and the data obtained were considered as initial. The examination program was the same for patients in both groups and included clinical, laboratory and instrumental methods. At 12, 24 and 36 months after surgery, patients were readmitted to the hospital for examination. We determined the parameters characterizing the morphological changes in the esophageal mucosa in various variants of reconstruction of the digestive tract after gastrectomy.
During dynamic observation, fibroesophageal intestinoscopy made it possible to visually assess the condition of the mucous membrane of the esophagus and small intestine involved in the formation of the anastomosis, diagnose focal and diffuse superficial erosive changes, determine the nature of the closure of the anastomosis, possible cicatricial inflammatory stenosis, and monitor the degree of inflammatory changes in the formed food reservoir. To assess the degree of inflammatory changes, the Savary-Miller classification of reflux esophagitis (1987) was used.
The main criterion for diagnosing reflux esophagitis was the data from a morphological study of areas of the esophageal mucosa taken during an endoscopic examination. The biopsy was performed in close proximity to the area of the formed esophageal anastomosis and above it. The resulting material was placed in a 2.5% glutaraldehyde buffer solution and fixed in formaldehyde for 24 hours. After embedding the treated material with paraffin, sections 4 μm thick were prepared and stained with hematoxylin and eosin. All preparations were examined under a light microscope; the pathologist did not have information about the clinical and endoscopic picture of the disease.
Comparison of groups of patients for each of the studied factors was carried out on the basis of a qualitative analysis of contingency tables using χ2 and Fisher tests in the statistical calculation program Excel 2007.
What not to do on a diet after gallbladder removal for adults
Foods high in cholesterol remain prohibited after surgery, as they cause thickening and stagnation of bile. Simple carbohydrates also cause bile stagnation, so their consumption is kept to a minimum. It is necessary to exclude from the menu foods that irritate the gastrointestinal tract. First of all, these are vegetables and fruits with a high content of essential oils and oxalic acid: spinach, sorrel, citrus fruits. Marinated and smoked products, as well as all types of pickles, are prohibited.
List of prohibited products:
| Flour | products made from premium flour, baked goods, industrial confectionery |
| Broths | rich broths from meat and fish, soups based on them |
| Meat | fatty meat and poultry (goose, duck, lamb, pork, lard and canned meat) |
| Fish | fatty varieties (catfish, mackerel, sturgeon, canned fish) |
| Semi-finished products | industrial sausages, sausages, smoked meats and liver |
| Vegetables | bitter and sour types (sorrel, spinach, green onions, garlic, radishes, daikon) |
| Fruits and berries | sour (cherry, plum, pineapple, all types of citrus fruits, persimmon) |
| Eggs | fried and egg yolks |
| Cereals | semolina, legumes |
| Milk products | fatty and sweet dairy products (yogurt, cottage cheese, raw milk, sour cream, whipped cream and ice cream) |
| Mushrooms | in any form |
| Beverages | carbonated mineral and sweet water, strong tea and coffee, cocoa, concentrated juices, alcohol |
Menu for a week for a diet after removal of the gallbladder for adults with recipes
The daily menu after gallbladder removal depends primarily on how long ago the operation was performed.
The strictest diet awaits patients immediately after the surgery. In the first hours after the operation, eating is prohibited. The day after cholecystectomy, you are allowed to drink rosehip decoction without sugar and still water. You need to drink in small sips and no more than 1-1.5 liters per day. Then liquid porridges and pureed soups made with water or vegetable broth are introduced into the diet.
The first week after surgery is the strictest; specific recommendations can only be prescribed by the attending physician. Further, the diet becomes more varied.
Expert's choice
The best drugs for the treatment of cholecystitis according to KP
Postcholecystectomy syndrome: diagnosis and treatment
Gallstone disease (GSD) is extremely common in civilized countries, including Russia. The incidence is especially high among women aged 35–40 years and older. GSD is characterized by the formation of gallstones in the biliary system, mainly in the gallbladder, and complications arising from the progression of the pathological process.
The main treatment for this disease is cholecystectomy. In 25% of patients who underwent cholecystectomy, abdominal pain and dyspeptic disorders that require treatment appear or persist after some time. Adequate therapy of patients depends on a correct understanding of the pathogenesis of clinical symptoms developing after cholecystectomy. The peculiarities of their formation are associated, on the one hand, with disturbances in cholesterol metabolism inherent in gallstone disease, and on the other, with the fact that the pathological process occurs in new anatomical and physiological conditions, i.e. in the absence of the gallbladder.
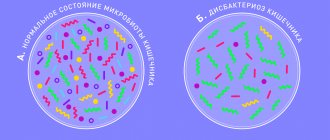
It is known that removal of the gallbladder for calculous cholecystitis does not relieve patients from metabolic disorders, including hepatocellular dyscholia, which persists after surgery. In most patients after cholecystectomy, lithogenic bile with a low cholate-cholesterol coefficient is determined. Loss of the physiological role of the gallbladder, namely the concentration of bile during the interdigestive period and its release into the duodenum during meals, is accompanied by a violation of the passage of bile into the intestines and indigestion. Changes in the chemical composition of bile and its chaotic entry into the duodenum disrupt the digestion and absorption of fat and other substances of lipid nature, reduce the bactericidal properties of duodenal contents, which leads to microbial contamination of the duodenum, weakened growth and functioning of normal intestinal microflora, disruption of the hepatic-intestinal circulation and decreased total pool of bile acids. Under the influence of microflora, bile acids undergo premature deconjugation, which is accompanied by damage to the mucous membrane of the duodenum, small and large intestines with the development of duodenitis, reflux gastritis, enteritis and colitis. Duodenitis is accompanied by duodenal dyskinesia and, first of all, duodenal hypertension with the development of duodenogastric reflux and reflux of contents into the common bile duct and pancreatic duct.
As a result, dyskinesia of the sphincter of the hepatopancreatic ampulla, bile and pancreatic ducts (sphincter of Oddi) is formed, and deconjugated bile acids cause the development of diarrhea. Thus, in patients with a removed gallbladder, the existing clinical manifestations may be associated with changes in the chemical composition of bile, impaired passage into the duodenum, dyskinesia of the sphincter of Oddi, as well as with excessive bacterial growth in the intestine, maldigestion and malabsorption syndromes, duodenitis and other pathological disorders in the digestive system. In addition, in a number of patients, organic obstructions to the outflow of bile associated with cholecystectomy may persist or develop again. Pathological conditions that are observed in patients after cholecystectomy can be divided into 3 groups.
- Functional disorders of the sphincter of Oddi - increased tone of the sphincter of the common bile duct or pancreatic duct or the common sphincter as a result of loss of a functioning gallbladder.
- Biliary hypertension with the presence of organic obstructions to the flow of bile, in the presence of which recurrent or residual choledocholithiasis is detected in 5–20% of patients, stenosis of the major duodenal papilla in 11–14%, strictures of the bile ducts and bile-ducting anastomoses in 6.5–20%, 0.1–1.9% have an excess stump of the cystic duct.
- Concomitant diseases that developed before or after surgery. The main ones are chronic pancreatitis, duodenal dyskinesia, irritable bowel syndrome, duodenitis, peptic ulcer, gastroesophageal reflux disease, hiatal hernia.
Currently, the term “postcholecystectomy syndrome” is used to designate only dysfunction of the sphincter of Oddi, caused by a violation of its contractile function and preventing the normal outflow of bile and pancreatic secretions into the duodenum in the absence of organic obstacles. It is proposed, instead of the previously accepted definitions “postcholecystectomy syndrome”, “biliary dyskinesia”, etc., to use the term “sphincter of Oddi dysfunction”.
Clinical manifestations of sphincter of Oddi dysfunction depend, first of all, on the involvement of one or another of its structures in the process. With isolated dysfunction of the common bile duct sphincter, biliary pain develops; with the predominant involvement of the pancreatic duct sphincter, pancreatic pain develops; and with pathology of the common sphincter, combined biliary-pancreatic pain develops. Dysfunction of the sphincter of Oddi is characterized by recurrent attacks of severe or moderate pain lasting 20 minutes or more, repeated for 3 months or more. With the biliary type, the pain is localized in the epigastrium or right hypochondrium with irradiation to the back and right scapula, with the pancreatic type - in the left hypochondrium with irradiation to the back, decreasing when bending forward, with the combined type - it has a girdling character. Pain can be combined with the following symptoms: a) onset after eating; b) appearance at night; c) nausea and/or vomiting.
However, assessment of clinical symptoms alone is not sufficient to exclude organic pathology of the biliary system. For this purpose, a number of screening and clarifying methods are used (table).
Non-invasive methods to suggest sphincter of Oddi dysfunction include blood levels of bilirubin, alkaline phosphatase, aminotransferases, amylase and lipase. Laboratory tests must be carried out during or no later than 6 hours after the end of a painful attack, as well as over time. A transient increase of 2 or more times in the level of liver or pancreatic enzymes during a period of at least 2 consecutive attacks of pain is important in confirming sphincter of Oddi dysfunction.
The provocative morphine-prostigmine test is of similar importance, when parenteral administration of drugs provokes the development of a painful attack, most often of a mixed biliary-pancreatic type in combination with an increase in the blood level of aminotransferases, alkaline phosphatase, and pancreatic enzymes. However, the diagnostic value of this test is limited by its low sensitivity and specificity.
During ultrasound, great importance is attached to the expansion of the common bile duct and main pancreatic duct, which indicates a violation of the flow of bile and pancreatic secretion at the level of the sphincter of Oddi. At the same time, in 3-4% of patients who have undergone cholecystectomy and have no symptoms, dilation of the common bile duct is noted. Of particular importance is ultrasound examination of the diameter of the common bile duct using fatty breakfasts, which stimulate the production of endogenous cholecystokinin and increase choleresis. After a test breakfast, the diameter of the common bile duct is measured every 15 minutes for 1 hour. An increase in its diameter by 2 mm or more compared to the initial one suggests the presence of incomplete obstruction of the common bile duct, both as a result of dysfunction of the sphincter of Oddi, and due to organic pathology of the biliary system.
To assess the condition of the pancreatic ducts, a test with the introduction of secretin at a dose of 1 mg/kg is used. Normally, after stimulation of pancreatic secretion by secretin, ultrasound shows an expansion of the pancreatic duct within 30 minutes, followed by its decrease to the initial level. If the duct remains dilated for more than 30 minutes, this indicates a violation of its patency.
With biliscintigraphy, the presence of dysfunction of the sphincter of Oddi is indicated by an increase in the transit time of the radiopharmaceutical from the porta hepatis to the duodenum, and it is proportional to the level of basal pressure of the sphincter of Oddi. At the same time, with dilated common bile duct, this study is of little information for assessing the function of the sphincter of Oddi.
Invasive methods for assessing the function of the sphincter of Oddi include an indirect method - endoscopic retrograde cholangiopancreatography (ERCP). Indirect signs of increased tone of the sphincter of Oddi are the diameter of the common bile duct more than 12 mm, the delay of contrast in the common bile duct for more than 45 minutes. Dysfunction of the sphincter of the main pancreatic duct is indicated by the expansion of the latter to more than 5 mm and a slowdown in the evacuation of contrast from its lumen. However, similar changes can be observed in the presence of organic pathology.
The most accurate method to confirm dysfunction of the sphincter of Oddi is manometry. In this case, it is possible to cannulate the common bile duct and Wirsung duct separately with manometry of their sphincters, which makes it possible to identify predominantly the biliary or pancreatic type of disorder, as well as to establish the etiology of recurrent pancreatitis in patients who have undergone cholecystectomy and papillotomy. Signs of sphincter of Oddi dysfunction during manometric examination are:
- increased basal pressure in the lumen of the sphincters;
- increased amplitude and frequency of phasic contractions (tachyodia);
- increased frequency of retrograde contractions;
- paradoxical response to the administration of cholecystokinin analogues.
Manometry of the sphincter of Oddi is not indicated for all patients. The choice of this study is based on an assessment of the severity of clinical manifestations and the effectiveness of conservative therapy.
Thus, we can assume that we are talking about dysfunction of the sphincter of Oddi in the following situations:
- the presence of pain in the epigastric region in patients who have undergone cholecystectomy, in cases where other causes that can explain their origin are not identified (concomitant diseases, structural changes in the biliary and pancreatic ducts);
- the presence of idiopathic recurrent pancreatitis;
- for recurrent biliary colic in patients with the presence of an unchanged gallbladder and common bile duct and with a normal composition of gallbladder bile.
Approximate formulations of diagnoses for patients who have undergone cholecystectomy:
Diagnosis: cholelithiasis, cholecystectomy in 1994 (for cases in which there are no clinical symptoms).
Diagnosis: dysfunction of the sphincter of Oddi of the biliary type. Gallstone disease, cholecystectomy in 1999
Diagnosis: chronic recurrent (obstructive) pancreatitis with exocrine and endocrine insufficiency in the acute phase.
Concomitant disease: cholelithiasis, cholecystectomy in 1994.
Diagnosis: irritable bowel syndrome with a predominance of constipation in the acute phase.
Concomitant diagnosis: cholelithiasis, cholecystectomy in 1994.
Management of patients who have undergone cholecystectomy. The goal of treatment: to restore the normal flow of bile and pancreatic secretions from the biliary and pancreatic ducts into the duodenum. Treatment objectives: normalize the chemical composition of bile; restore the patency of the sphincter of Oddi; restore the normal composition of intestinal microflora; normalize digestive processes and small intestinal motility to prevent duodenal hypertension.
To prevent the formation of bile sludge or stones in the extrahepatic biliary system, it is recommended:
- limiting (but not completely eliminating) the intake of foods containing cholesterol (fats of animal origin) and fatty acids (fats that have been heat-treated over 100°C - fried foods);
- regular 4-6 meals a day;
- slow weight loss. When using low-calorie diets (2110 kJ/day and below), during fasting, during shunt operations, additional administration of ursodeoxycholic acid at a dose of 10 mg/kg/day is necessary;
- adding dietary fiber contained in products of plant origin or food additives (bran, etc.) to the diet. At the same time, it is better to use vegetables, fruits, and herbs after heat treatment (boiled, baked). Bran can be used in the form of ready-made breakfasts (porridge, bread) and proprietary preparations;
- providing daily bowel movements.
Drug treatment for sphincter of Oddi dysfunction is aimed at relieving spasm of the smooth muscles of the latter. For this purpose, a number of drugs that have an antispasmodic effect are used. Nitrates: nitroglycerin is used for quick pain relief, nitrosorbitol is used for course treatment. The mechanism of action of nitrates is reduced to the formation of free radicals of nitric oxide (NO) in smooth muscles, which activate guamylate cyclase and increase the content of cGMP, which leads to their relaxation. However, pronounced cardiovascular effects, side effects and the development of tolerance make them unsuitable for long-term treatment of sphincter of Oddi dysfunction.
Anticholinergics block muscarinic receptors on the postsynaptic membranes of target organs. As a result, calcium channels are blocked, the entry of calcium ions into the cytoplasm of smooth muscle cells is stopped and, as a result, muscle spasm is relieved. Both non-selective (belladonna preparations, metacin, platiphylline, buscopan, etc.) and selective M-cholinergic blockers (gastrocepin, etc.) are used as antispasmodics. However, when taking drugs in this group, a fairly wide range of side effects can be observed: dry mouth, urinary retention, visual disturbances, increased intraocular pressure, tachycardia, constipation, drowsiness. The combination of rather low effectiveness with a wide range of side effects limits the use of drugs in this group for sphincter of Oddi dysfunction.
Blockers of slow calcium channels - phenylalkylamines (verapamil, gallopamil), 1,4-dihydroperidines (nifedipine, amlodipine) and benzothiazepines (diltiazem, etc.) close calcium (“slow”) channels of cell membranes, prevent the entry of calcium ions into the cytoplasm of smooth muscle cells and cause her relaxation. The drugs have numerous cardiovascular effects, primarily vasodilating, and therefore have not found widespread use in the treatment of sphincter of Oddi dysfunction. There are only a few publications on the use of nifedipine for sphincter of Oddi dysfunction, and the feasibility of their use requires further study.
Myotropic antispasmodics, the mechanism of action of which is the inhibition of phosphodiesterase, or the activation of adenylate cyclase, or the blockade of adenosine receptors, which leads to a decrease in the tone and motor activity of smooth muscles. Representatives of this group of drugs are drotaverine (no-shpa, no-shpa forte), bencyclane (halidor), dicycloverine (trigan-D), alverine (meteospasmil), etc.
The main disadvantages of drugs from all of the above groups are:
- significant differences in the effectiveness of treatment for sphincter of Oddi dysfunction in each specific case;
- lack of a selective effect on the sphincter of Oddi;
- the presence of undesirable effects caused by effects on the smooth muscles of blood vessels, the urinary system and all parts of the digestive tract.
In contrast, hymecromone (odeston) has a selective antispasmodic effect on the sphincter of Oddi and the sphincter of the gallbladder. In addition, the drug does not increase pressure in the biliary tract, does not affect the secretory function of the digestive glands and intestinal absorption processes.
In restoring the normal outflow of bile in the absence of a gallbladder, along with the patency of the sphincter of Oddi, the level of pressure in the duodenum is of great importance. If it exceeds the secretory pressure of bile and pancreatic juice, they will be deposited in the biliary and pancreatic ducts with corresponding consequences.
In this regard, resolution of duodenal hypertension is considered an indispensable condition for the management of patients with sphincter of Oddi dysfunction. When choosing treatment tactics, it should be taken into account that the main pathogenetic mechanism for the development of duodenal hypertension is the excess content of liquid and gas in the lumen of the duodenum as a result of fermentation and putrefactive processes caused by microbial contamination.
To decontaminate the duodenum, 1-2 seven-day courses of antibacterial therapy are carried out with a change of drug during the next course of treatment. The drugs of choice are: doxycycline 0.1 g 2 times a day, tetracycline 0.25 g 4 times a day, biseptol 960 mg 2 times a day, furazolidone 0.1 g 3 times a day, ersefuril 0.2 g 4 times a day day, ciprofloxacin 250 mg 2 times a day, metronidazole 0.25 g 4 times a day, Intetrix 1 capsule 4 times a day, less often - chloramphenicol 0.25 g 4 times a day.
The selection of drugs is usually carried out empirically. For severe symptoms of dyspepsia, 2 drugs are prescribed at once, one of which should act primarily on anaerobic microflora (for example, metronidazole). Along with taking intestinal antiseptics, in some cases prebiotics are prescribed: in the presence of diarrhea - Hilak Forte 60 drops 3 times a day for 1 week, then 30 drops 3 times a day for 2 weeks; in cases of predominance of constipation - lactulose 1-2 tablespoons 1 time per day until stool normalizes.
After completion of antibacterial therapy, probiotics (preparations containing normal strains of intestinal flora) are indicated. One of the well-known representatives of the group of probiotics is bifiform, which contains in one enteric-coated capsule, enterococci 107, bifidumbacteria 107 and a nutrient medium that promotes their growth in the small and large intestines. The drug is prescribed 1 capsule 2 times a day for 2 weeks. In combination with antibacterial agents, it is necessary to prescribe aluminum-containing buffer antacids (alugastrin, alumag, maalox, phosphalugel, smecta, etc.). Any of the drugs is taken 1 dose 1 hour after breakfast, lunch and dinner and before bedtime (cannot be combined with Hilak Forte). The duration of treatment is 5–7 days. The feasibility of using these drugs is due to their following abilities:
- bind organic acids, which leads to a decrease in the osmolarity of intestinal contents and cessation of fluid flow into the intestinal lumen;
- increase the intraduodenal pH level, which creates conditions for normal digestive processes;
- bind deconjugated bile acids, which reduces secretory diarrhea and their damaging effect on the mucous membrane;
- reduce the absorption of antibacterial drugs, which increases their concentration in the intestinal lumen and enhances the antibacterial effect, and also reduces the side effects of drugs.
The presence in most patients of relative enzyme deficiency as a result of the destruction of digestive enzymes by duodenal and small intestinal microflora, a decrease in intraduodenal pH levels, as well as disruption of the process of mixing them with food chyme is the rationale for the prescription of enzyme preparations. If you are prone to diarrhea, pancreatin preparations are prescribed: mezim forte, creon, licrease, pancitrate and others, 1 dose 2-3 times a day at the beginning of meals; if you are prone to constipation - combined products containing pancreatin, bile acids, hemicellulose: festal, enzistal, digestal, 1 tablet 2-3 times a day at the end of meals. The duration of treatment is individual and, as a rule, does not exceed 10 days.
We present indicative schemes for the management of patients with sphincter of Oddi dysfunction.
Diagnosis: dysfunction of the sphincter of Oddi of the biliary type. Gallstone disease, cholecystectomy in 1996
- Low-fat diet (40 g/day vegetable fats), excluding fried, spicy, sour foods.
- Gimecromon (odeston) 200 mg 3 times a day 30 minutes before meals for 7–14 days.
- Exclusion of drugs that have a choleretic and hydrocholeretic effect (bile acids, including in enzyme preparations, infusions and decoctions of choleretic herbs, synthetic choleretic drugs, gastric juice, etc.).
Diagnosis: dysfunction of the sphincter of Oddi of the biliary type. Gallstone disease, cholecystectomy in 1989. Concomitant diseases: chronic catarrhal, mainly distal duodenitis. Small intestinal bacterial overgrowth syndrome.
- Low-fat diet (40 g/day vegetable fats), excluding fried, spicy, sour foods.
- Gimecromon (odeston) 200–400 mg 3 times a day for 30 minutes. before meals - 1-2 weeks.
- Biseptol 480 2 tablets 2 times a day for 5–7 days, from days 6–8 doxycycline 0.1 g 2 times a day or ciprofloxacin 250 mg 2 times a day for 5 days, followed by bifiform 1 capsule 2 times a day for 2 weeks.
- Pancreatin 250–500 mg, or mezim forte, or creon, or lycrease, or pancitrate, 1 tablet or 1 capsule 3 times a day with meals - up to 2 weeks, then “on demand”.
- Alumag (Maalox protab, phosphalugel, etc.) 1-2 doses 3 times a day 1 hour after meals for 1 week.
Thus, timely and correct assessment of the clinical symptoms developing in patients after cholecystectomy makes it possible to select adequate therapy and, as a result, significantly improve the quality of life of patients with diseases of the hepatobiliary system.
For questions regarding literature, please contact the editor.
P. Ya. Grigoriev, Doctor of Medical Sciences, Professor, E. P. Yakovenko, Doctor of Medical Sciences, Professor N. A. Agafonova, Candidate of Medical Sciences, A. S. Pryanishnikova, I. P. Soluyanova, Candidate of Medical Sciences Sciences, Z. V. Bekuzarova, A. V. Yakovenko, Candidate of Medical Sciences, Russian State Medical University, Moscow
Sample menu for 7 days for the first month after surgery
Day 1
Breakfast : cottage cheese casserole with raisins, green tea Snack : 50 gr. crackers + a glass of compote (no sugar) Lunch : pumpkin puree soup with crackers, turkey fillet baked in foil Snack : curdled milk with apple Dinner : salad with seafood, fresh cucumber and herbs, seasoned with pumpkin oil, toasted bran bread
Recipe for pumpkin puree soup with croutons:
- Pumpkin – 1 kg;
- Potatoes – 2-3 pcs.;
- Onions – 1 pc.;
- Carrots – 2-3 pcs.;
- Vegetable broth – 1 l.;
- Salt - to taste;
- Chopped greens - for serving;
- Olive oil - for serving;
- Crackers - for serving.
Cooking:
- Peel the pumpkin from seeds and peel. Cut into small cubes.
- Peel potatoes, onions and carrots and cut into cubes.
- Heat the vegetable broth in a thick-bottomed saucepan and add the prepared vegetables.
- Cook vegetables over medium heat until broth comes to a boil. Next, reduce the heat to low, cover with a lid and cook the vegetables until cooked.
- When the vegetables can be easily pierced with a fork, turn off the heat and let the soup cool.
- Turn the cooled broth with vegetables into a homogeneous puree using a blender or food processor.
- Serve the finished soup in portioned bowls, garnished with chopped herbs, a handful of homemade croutons and a few drops of olive oil.
Day 2
Breakfast : boiled buckwheat porridge with butter, biscuits with low-fat cheese Snack : baked pear with cottage cheese Lunch : rice with vegetables, chicken breast baked in foil Snack : fruit pastille, tea Dinner : veal meatballs, cauliflower puree
Day 3
Breakfast : protein omelet with vegetables, baked in the oven, biscuit with butter tea Snack : banana Lunch : steamed pike perch fillet, baked vegetable salad Snack : mashed cottage cheese with fresh cucumber and herbs Dinner : steamed fish cutlets, stewed cabbage, biscuit
Roasted vegetable salad recipe:
- Zucchini – 2 pcs.;
- Tomato – 3 pcs.;
- Bell pepper – 1 pc.;
- Onions – 2 pcs.;
- Salt - to taste;
- Olive oil – for dressing.
Cooking:
- Preheat the oven to 200 degrees.
- Wash the vegetables thoroughly and dry.
- Place peeled onions in one baking dish. Cooking time is approximately 45 minutes.
- Place peppers, tomatoes, and zucchini in the second pan. Cooking time is approximately 25 minutes.
- Remove the prepared vegetables from the oven and let them cool.
- Chop the cooled vegetables and season with chopped herbs, salt and olive oil.
Important
What does a brown coating on the tongue mean? Is it dangerous?
Day 4
Breakfast : oatmeal in water with dried apricots and crushed almonds, cracker, boiled egg Snack : fruit chips from apple, pear or banana Lunch : fish soup, salad of Chinese cabbage, cucumber and carrots, dressed with sesame oil, biscuits Snack : bread with vegetables juice Dinner : beet salad with prunes and nuts, stuffed peppers
Day 5
Breakfast : cheesecakes baked in the oven with fruit puree, rosehip broth Snack : kefir, a handful of hazelnuts Lunch : rice with seafood, salad with leafy greens and baked beets, dressed with olive oil Snack : homemade compote with crackers Dinner : carrot cutlets, chicken pate breasts, biscuits
Carrot cutlet recipe:
- Carrots – 500 gr.;
- Egg – 1 pc.;
- Green buckwheat flour – 3 tbsp;
- Dried herbs - to taste;
- Salt - to taste.
Cooking:
- Wash and peel the carrots. Slice and boil until done.
- Grind the boiled carrots in a convenient way (grater, blender).
- Add the egg and green buckwheat flour to the chopped carrots, mix thoroughly.
- Add salt and dried herbs.
- The carrot “mince” can be placed in silicone molds or formed into cutlets with wet hands and placed on parchment.
- Bake in an oven preheated to 200 degrees for about 15-20 minutes.
Day 6
Breakfast : rice porridge with baked pumpkin, cracker with poached egg Snack : galette with cheese Lunch : vegetable stew, pollock baked in foil with herbs and butter Snack : homemade jelly with cracker Dinner : meat casserole, boiled cauliflower and broccoli with olive oil
Day 7
Breakfast : rice pudding with fruit sauce, cracker with turkey pate Snack : kefir with dried fruits Lunch : beef cabbage soup in secondary broth, croutons, summer salad with mustard oil Snack : banana, a handful of almonds Dinner : pike fillet baked with vegetables with tomato sauce, toasted bread, low-fat cheese
Recipe for rice pudding with fruit sauce:
- Rice – 250 gr.;
- Oat milk – 100ml;
- Egg – 2 pcs.;
- Peach – 2 pcs.;
- Apples – 2 pcs.;
- Sugar – 3 tbsp.
Cooking:
- Boil the rice according to the instructions on the package.
- Pour milk into a thick-bottomed pan and add the cooked rice to it. Boil the rice in milk for a few minutes.
- Remove the pan with rice from the heat and let cool.
- Add the yolks to the cooled rice and stir. Beat the whites to strong peaks and also add to the rice.
- Place the rice mixture in a baking dish. Cook for about 30 minutes in an oven preheated to 180 degrees.
- Wash and peel the fruits for the sauce. Cut into cubes and simmer in a saucepan with sugar for a few minutes. Let cool and rub them through a sieve.
- Serve the rice pudding in portions and top with the fruit sauce.
Good to know
How to provide first aid during an attack of cholecystitis
Popular questions and answers
We discussed how to eat properly after removal of the gallbladder with an endocrinologist and nutritionist Ekaterina Kazachkova .
Is the diet after gallbladder removal for life?
— A strict diet must be maintained for the first 3-4 months after surgical treatment. Depending on the pace of recovery (and they are very individual), over time the daily menu can gradually expand. However, you need to remember that you need to introduce new products gradually, in small quantities and be sure to monitor the body’s reaction, and only after consultation with your doctor.
What can a lack of diet lead to in the first month after surgery?
— If you do not follow the recommended diet, the risk of postoperative complications increases, such as postoperative diarrhea, dysfunction of the sphincter of Oddi, which leads to pain and digestive disorders.
Is it possible to form stones after gallbladder removal?
- Yes, this happens, but it is extremely rare when stones can form in the bile ducts.
To prevent this situation, it is recommended to adhere to a diet on an ongoing basis. Sources :
- Laparoscopic cholecystectomy. Koshenov M.R. Bulletin of Surgery of Kazakhstan, 2012. https://cyberleninka.ru/article/n/laparoskopicheskaya-holetsistektomiya-1/viewer
- Dysfunction of the sphincter of Oddi in the postcholecystectomy period. Bueverov A.O. Medical Council, 2022. https://cyberleninka.ru/article/n/disfunktsiya-sfinktera-oddi-v-postholetsistektomicheskom-periode/viewer
- Modern view on the problem of postcholecystectomy syndrome. Neresov A.V., Kaibulaeva D.A., Vasnev O.S., Tashenova L.K., Sakhipov M.M., Berestimov G.T. and others. Pharmacoeconomics. Modern pharmacoeconomics and pharmacoepidemiology. https://cyberleninka.ru/article/n/sovremennyy-vzglyad-na-problemu-postholetsistektomicheskogo-sindroma-po-materialam-ekspertnogo-soveta-sostoyavshegosya-4-maya-2019/viewer
Introduction
Numerous morphological studies have established that the cardia lacks an anatomical muscular sphincter similar to the muscular sphincter of the pylorus. The regulation of the passage of food from the esophagus to the stomach and the prevention of gastroesophageal reflux is performed by the so-called functional sphincter of the cardia, which includes the angle (20-40˚) of the transition of the esophagus to the stomach - the angle of His, the gas bubble in the fundus of the stomach; peraeesophageal ligament; mucous rosette, or Gubarev valve. In the functional sphincter, the gas bubble plays a decisive role [9].
During gastrectomy, elements of the functional sphincter of the cardia are removed, which leads to the free flow of duodenal contents into the small intestine and then through a vertically formed esophagojejunostomy into the esophagus with the development of reflux esophagitis. Enteroesophageal reflux of small intestinal contents after gastrectomy is the cause of the development and progression of inflammation in the esophageal mucosa [10]. If in patients with an unoperated stomach the main substrate for the development of inflammatory, and subsequently structural changes in the esophageal mucosa is hydrochloric acid contained in gastric juice, then after gastrectomy reflux of the contents of the small intestine occurs, the entry of alkaline contents of the duodenum, bile acids and pancreatic enzymes. The damaging effect of bile acids depends on the pH of the environment. At pH from 3.0 to 6.0, the damaging effect of bile acids is maximum; at pH 2.0, bile acids precipitate. In this regard, the acidity of gastric juice is considered as a kind of natural barrier to the effect of bile on the esophageal mucosa, which is eliminated during gastrectomy [3].
Current methods of conservative treatment of reflux esophagitis that occurs after removal of the stomach are ineffective [6]. The only effective way to prevent the development of enteroesophageal reflux and reflux esophagitis after gastrectomy is to prevent regurgitation of the contents of the small and duodenal intestines into the esophagus [7, 8].
To prevent enteroesophageal reflux, numerous methods have been developed for the formation of areflux esophagojejunostomoses using muscle cuffs from the wall of the small intestine, from the wall of the esophagus, intraintestinal valves like a non-pouring inkwell, etc. [1, 2, 5]. However, as an analysis of the pathogenesis of enteroesophageal reflux shows, the low effectiveness of standard and areflux esophagojejunostomoses is due to one thing - the proposed methods do not provide for the restoration of the defining structural elements of the removed functional sphincter of the cardia, in particular the gas bubble, which provides compression of the abdominal esophagus and is capable of restoring the valve mechanism, which only acts in the craniocaudal direction.
The main symptoms of enteroesophageal reflux are heartburn, mainly at night when the patient is in a horizontal position for a long time, regurgitation of bile, belching, pain in the chest when lifting heavy objects and when bending the body forward. Most researchers agree that the clinical manifestations of enteroesophageal reflux in the form of symptoms of regurgitation in the first months after gastrectomy do not have morphological signs of esophagitis [4, 8].
Enteroesophageal reflux, detected using X-ray and radioisotope research methods, the frequency of which after gastrectomy reaches 30%, does not indicate the inevitable development of structural changes in the esophageal mucosa, which are diagnosed in no more than half of patients with enteroesophageal reflux [10]. As a rule, the result of histological examination of biopsy samples of the esophageal mucosa is a discrepancy between the endoscopic picture and morphological changes.
The standard in the diagnosis of reflux esophagitis is esophagoscopy with targeted biopsy of the mucous membrane of the distal esophagus in close proximity to the esophageal-intestinal anastomosis, followed by morphological examination.
Diagnosis based on clinical, radiological and endoscopic studies with targeted biopsy of the mucous membrane of the distal esophagus allows not only to visualize the reflux of small intestinal contents through the esophageal-intestinal anastomosis into the esophagus, but also to verify the morphological changes characteristic of esophagitis.
The purpose of this study is to analyze the long-term results of gastrectomy using a new variant of reconstruction of the digestive tract to prevent the development of reflux esophagitis.