The disease is a common pathology and requires immediate surgical intervention. Surgery to remove the appendix is considered safe and does not affect subsequent health. Surgeons warn that ignoring primary symptoms and prolonged refusal to hospitalize causes the development of complications, including peritonitis. In the latter case, the risk of death increases.
Causes of appendicitis
The exact reasons for the development of the inflammatory process are still unclear. But there are several common options:
- Disturbance in the balance of microflora - bacteria that are safe in a normal environment become toxic and cause inflammation.
- Vasospasm causes deterioration in tissue nutrition. Some areas die and become a source of infection.
- Stagnation in the intestines - feces, foreign bodies, neoplasms or parasites can close the lumen of the appendix. At the site of closure, mucus accumulates, where the microbiome begins to multiply. Narrowing and compression of the appendix disrupts blood circulation and lymph flow, which leads to rapid progression of inflammation and necrosis of appendix tissue.
A predisposing factor will be frequent constipation, which forms fecal stones.
Symptoms of appendicitis
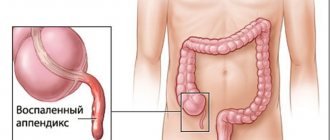
The appendix is located in the lower abdomen. The first symptom is unbearable pain that appears in the navel area and spreads to the lower right side of the abdomen. The pain worsens over a short period of time when moving, taking a deep breath, coughing or sneezing.
Other typical symptoms:
- nausea, even vomiting
- decreased or complete lack of appetite
- constipation or, conversely, diarrhea
- flatulence, painful bloating
- fever, chills, symptoms of intoxication
- urge to defecate
Signs of inflammation of the appendix may differ in men and women. For example, women experience nausea, vomiting and fever. At the beginning of the development of the disease, the pain is pressing, pulling, and not even necessarily on the right side, which can be mistakenly recognized as gynecological problems.
Then the pain may become cramping, such symptoms most often occur in the evening or at night.
In men with acute inflammation, severe pain in the abdominal area and spontaneous tightening of the right testicle occur. When the scrotum is pulled back, discomfort and pain occur in the anal area and a strong urge to have a bowel movement.
In older people, the symptoms of appendicitis may appear less clearly: minor pain, mild nausea. At the same time, appendicitis in older people is often characterized by a severe course and the development of complications.
In children under 5 years of age, the symptoms of appendicitis are not as pronounced as in adults. The pain often has no clear localization. Appendicitis in a small child can be recognized by increased body temperature, diarrhea and the presence of plaque on the tongue.
Signs of perforation of the appendix
As already mentioned, appendicitis can burst even a couple of hours after the onset of the pathological process, although most often this occurs within 24-48 hours. Bursting appendicitis causes the following symptoms:
Sick leave after appendicitis
- pain in the abdomen and back;
- the pain intensifies when laughing, coughing, or lying on the left side;
- nausea;
- vomiting;
- chills;
- diarrhea;
- trembling in the limbs;
- headache;
- tachycardia (130-140 beats per minute);
- temperature rise to 40 C.
If the pain disappears, then this is a sign of death of the nerve endings and gangrene of the appendix. If you suspect appendicitis, you should immediately seek medical help, since treatment consists of surgical removal of the inflamed appendix.
Until the ambulance team arrives, you should not drink, eat, take painkillers, or apply heat to your stomach.
Types of pathology
Acute appendicitis develops rapidly and manifests itself with pronounced symptoms. With inaction, the pain intensifies and inflammation can lead to serious complications.
By its nature, acute appendicitis can be complicated or uncomplicated. Uncomplicated pathology, in turn, has 2 forms: catarrhal (only the mucous membrane is inflamed), destructive (deeper layers are affected).
Chronic is a fairly rare form. In most cases, it develops as a result of acute appendicitis in the absence of treatment. Has the same symptoms, but they manifest themselves very sluggishly. There are periods of exacerbation and remission, like any chronic disease.
Chronic appendicitis is also divided into subtypes:
- Residual - a consequence of acute appendicitis that ended in self-healing. It manifests itself as a dull aching pain in the right iliac region.
- Recurrent – has a paroxysmal nature: exacerbations occur from time to time, followed by remission.
- Primary chronic – develops independently, without preceding acute appendicitis.
Literature
1. McBurney C. Experiences with early operative interference in cases of disease of the vermiform appendix. NY Med J 1889;50:1676-1684.
2. Coldrey E. Five years of conservative treatment of acute appendicitis. J Int Coll Surg 1959;32:255-261.
3. Anonymous. R. Combined traditional Chinese and western medicine in acute appendicitis. Chin Med J 1977;3:266-269.
4. Surana R, Quinn F, Puri P. Is it necessary to perform appendectomy in the middle of the night in children. BMJ 1993;306:1168.
5. Ambjommson E. Management of appendiceal abscess. Curr Surg. 1984;41:4-9.
6. Bagi P, Oueholm S. Non-operative management of the ultrasonically evaluated appendiceal mass. Surgery. 1987;101:602-605.
7. Engkvist O. Appendectomy a froid: a superfluous routine operation? Acta Chir Scand 1971;137:797-800.
8. McPherson AG, Kinmoth JB. Acute appendicitis and the appendix mass. Br J Surg. 1945;32:365-70. doi:.10.1002/bjs.18003212705.
9. Thomas DR. Conservative management of the appendix mass. Surgery 1973;73:677-80.
10.EACS. Acute appendicitis—Operative versus conservative management: EACS guidelines for endoscopic surgery. Heidelberg: Springer, 2006, pp. 387-389.
11. Mosegaard A, Nielsen OS. Interval appendectomy: A retrospective study. Acta Chir Scand 1979;145:109-11.
12. Adams ML. The medical management of acute appendicitis in a non-surgical environment: a retrospective case review. Mil Med. 1990;155:345-347.
13. Gurin NN, Slobodchuk IUS, Gavrilov IUF. The efficacy of the conservative treatment of patients with acute appendicitis on board ships at sea. Vestn Khir 1992;148:144-150.
14. Eriksson S, Granstrom L. Randomized controlled trial of appendectomy versus antibiotic therapy for acute appendicitus. Br J Surg. 1995;82:166-169. doi:10.1002/bjs.1800820207.
15. Malik AA, Wani NA. Continuing diagnostic challenge of acute appendicitis-evaluation through modified Alvarado score. Aust NZ J Surg 1998;68:504-505.
16. Eriksson S, Granstrom L, Bark S. Laboratory tests in patients with suspected acute appendicitis. Acta Chir Scand 1989;155:11 -20.
17. Granstrom L, Erikson S, Tisell A. Ultrasonography as a tool in the diagnosis of acute appendicitis: A prospective study. Surg Res Commun 1992;11:309-314.
18. Puylaert JBCM. Acute appendicitis US evaluation using graded compression. Radiology 1986;158:355-360.
19. Huskisson EC. Measurement of pain. Lancet 1974;2(7889):1127-1131.
20. Horton MD, Counter SF, Florence MG, Hart MJ. A prospective trail of computed tomography and ultra sonography for diagnosing appendicitis in the atypical patients. Am J Surg 2001;182(3):305-306.
21. Oeutsch AA, Shani N, Reiss R. Are some appendicectomies unnecessary? An analysis of 319 white appendices. JR Coll Surg Edinb 1983;28:35-40.
22. Pieper R, Kager L, Nasman P. Acute appendicitis: a clinical study of 1018 cases of emergency appendectomy. Acta Chir Scand 1982;148:51 -62.
23. Kalan M, Talbot D, Cunliffe WJ, Rich AJ. Evaluation of the modified Alvarado score in the diagnosis of acute appendicitis. A prospective study. Ann R Coll Surg Engl. 1994;76:418-419.
24. Arnbjornsson E. Small intestinal obstruction after appendectomy: an avoidable complication? Curr Surg 1984;41:354-357.
25. Raf LE. Causes of abdominal adhesions in cases of intestinal obstruction. Acta Chir Scand 1969;135:73-76.
26. Grosfeld JL, Weinberger M, Clatworthy HW Jr. Vascularized appendical transplants in biliary and urinary tract replacement. J PediatrSurg 1971;6:630-638. doi:10.1016/0022-3468(71)90389-7.
27. WeinJberg RW. Appendix ureteroplasty. Br J Urol 1976;48:234.
28. Eriksson S, Granstrom L, Tisell A. Ultrasonography in suspected acute appendicitis. Is it difficult to learn. Br J Surg 1993;80(suppl):4.
29. Singh JK et al. Imaging of acute abdomen and pelvis: Acute appendicitis and beyond. Radiographies 2007;27:1419-1431.
30. Athey PA, Hacken JB, Estrada R. Sonographic appearance of mucocele of the appendix. J Clin Ultrasound. 1984;12:333-337.
31. Simpson J, Scholefield J. Acute appendicitis. The Foundation Years 2006;2(2):72-75.
2. Roggo A, Wood WC, Ottinger LW. Carcinoid tumors of the appendix. Ann Surg 1993;217:385-90.
Diagnosis of appendicitis
The first step in examining a patient is an examination and history taking. The doctor asks you to tell us when the symptoms began and how long the discomfort lasts. This is important to understand in order to distinguish the disease from something else.
It is important to consider other factors that could cause the development of appendicitis:
- Surgical operations in the abdominal area in the recent past.
- Taking medications or supplements.
- Bad habits, abuse of alcohol, drugs, etc.
Feeling the abdomen will help determine the location and intensity of pain, its characteristics. A pelvic and rectal examination may be necessary. The final diagnosis is made only after laboratory tests. Blood and urine tests can help detect signs of inflammation or other health problems.
Visual examination methods may also be required - ultrasound of the abdominal organs, CT or MRI. They will allow:
- determine the condition of the appendix and assess its integrity
- detect signs of inflammation
- evaluate blockage inside the appendix
- identify an abscess or other complications
Methods
Pain was recorded using visual analogues every 6 hours in hospital - from 0 points to 100, pain was relieved with intramuscular diclofenac, and after discharge - with paracetamol.
Ultrasound was performed on days 12 and 30. Moreover, in 38 patients treated conservatively with antibiotics, the process was visualized in 15 on the 12th day. A month later, in 15 patients, the appendix was visualized in 9. Of these 9, 4 had a relapse of appendicitis a year later. All conservatively treated patients with recurrent OA underwent surgery.
How to treat appendicitis?
The pathology requires immediate treatment, since the appendage may burst and its contents will spill into the abdominal cavity and peritonitis will begin. Therefore, the only solution is to remove the appendix surgically.
Appendectomy is a surgical operation to remove the appendix. It can be carried out in two ways:
- classic – abdominal surgery
- laparoscopic, when there are no large incisions
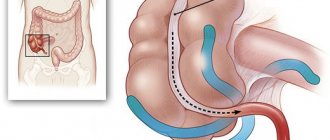
Abdominal surgery is performed if the appendix ruptures and if its contents spill into the abdominal cavity, as well as if the rupture causes an abscess.
Laparoscopy is considered the most modern method of removing the appendix for various reasons: less invasiveness, quick recovery, and fewer complications.
The operation is carried out as follows:
- the surgeon makes small incisions through which access to the appendix appears
- a camera with illumination is introduced
- other instruments are used to remove the process
- areas are treated to disinfect infectious material
- the operated area is examined and sutures are placed