Pancreatic cancer is a malignant neoplasm that develops from glandular tissue or ducts. Pancreatic cancer affects the organ and very quickly invades nearby tissues. The symptoms of pancreatic cancer are often invisible until the final stages occur. The first signs of pancreatic disease begin to appear when the formation increases in volume and begins to spread in the body, metastasizing to the lymph nodes, liver, bones, lungs and other organs and systems.
The Scientific and Practical Surgery Center has ultra-modern equipment to combat cancer. Diagnosis and treatment are carried out by highly qualified specialists who have modern methods of treatment, who have undergone practical and theoretical training in advanced cancer treatment technologies in recognized global cancer centers.
What is pancreatic cancer?
Pancreatic cancer is a life-threatening tumor of the organ that produces substances necessary for digesting food and absorbing sugar.
The disease accounts for approximately 3% of all cancer diagnoses, and slightly less than 10% of all deaths from them.
Such formations are difficult to detect due to the location of the gland and the absence of symptoms in the early stages, as a result of which treatment is often started only in advanced stages, when dangerous cells have already spread throughout the body.
Clinical manifestations of the disease
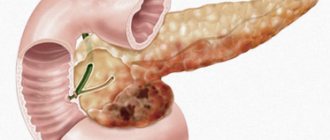
The clinical manifestations of the disease and their combination are determined by the area of damage to the pancreas (head, body, tail).
Pancreatic head cancer
Cancer of the head of the pancreas (carcinoma) is manifested by the development of persistent yellowness of the mucous membranes and skin with a dark green tint (obstructive jaundice), itching of the skin, paroxysmal pain in the right upper abdomen; when the tumor grows into the Vater’s nipple, “silver stool” (a mixture of bile) may be observed and blood in stool).
Pancreatic body cancer
Pancreatic body cancer is characterized by severe girdling pain in the upper abdomen, the intensity of which is determined by germination into the solar plexus (solar syndrome). The pain is relieved by being forced to lie on the stomach or by bending the torso forward.
Pancreatic tail cancer
Cancer of the tail of the pancreas manifests itself as vague, dull pain in the upper left half of the abdomen and left hypochondrium. The patient may show signs of carbohydrate metabolism disorders (increased or decreased blood glucose - diabetes mellitus or glycemic syndrome). More often than with other localizations of pancreatic cancer, a tumor may be palpable.
When the tumor grows or the nerve trunks and plexuses are compressed, the pain becomes constant, severe, and unbearable. Complications of pancreatic cancer are manifested by thrombosis (blockage of blood vessels with blood clots), most often thrombosis of the splenic vein, enlargement of the spleen (splenomegaly). As the disease progresses, metastasis occurs, primarily to the liver (the liver becomes lumpy, rocky in density) and other organs.
How does pancreatic cancer develop?
The pancreas is a vital organ located behind the stomach, next to the gallbladder. It consists of three parts - head, body and tail, and produces enzymes - substances necessary for the digestion of fats, carbohydrates and proteins. In addition, it produces hormones responsible for the distribution of sugar. Hormones are substances that are created by our glands, enter various organs through the bloodstream and tell them how to act - work or rest, secrete something or absorb. : Insulin helps cells convert glucose into energy, and glucagon increases blood levels when they drop too low.
Cancer develops gradually: first, one cell that does not resemble healthy cells appears in the gland, which grows, multiplies and creates a tumor. Over time, such a formation becomes larger and larger and damages not only the pancreas itself, but also the organs located next to it.
Such cells appear due to many reasons - hereditary predisposition, exposure to harmful substances, various diseases or random failures. The immune system manages to cope with most of them, but some still manage to deceive our natural defenses and disguise themselves as healthy.
Unlike normal cells, which spend their entire lives in a strictly defined place in the tissue, cancer cells are able to move throughout the body. They enter the circulatory and lymphatic systems. The lymphatic system complements the cardiovascular system. The lymph circulating in it - the intercellular fluid - washes all the cells of the body and delivers the necessary substances to them, taking waste from them. In the lymph nodes, which act as “filters,” dangerous substances are neutralized and removed from the body. systems, with their help they move to any parts of the body located far from the gland, become fixed in them and create new cancerous tumors - metastases.
Gradually, oncology destroys more and more vital organs, which stop working and fail.
Types of Pancreatic Cancer
The main difference between types of oncology is which glands they affect.
Adenocarcinoma
– in most cases occurs in the ducts Ducts are thin tubes through which digestive juice flows from the pancreas to the duodenum. and accounts for up to 95% of all cases of pancreatic cancer. It develops in exocrine cells that produce enzymes - substances that enter the intestines and are involved in the digestion of fats, proteins and carbohydrates.
Neuroendocrine tumors
- are formed in those responsible for the production of hormones Hormones are substances that are created by our glands, enter various organs through the bloodstream and tell them how to act - to work or rest, to secrete something or absorb something. cells:
- insulinomas - those that secrete insulin, which transfers sugar from the blood to other cells;
- glucagonomas – those that produce glucagon, which releases glucose from the body’s reserves;
- gastrinomas – those that create gastrin, which regulates the acidity of gastric juice;
- somatostatinomas - those that produce somatostatin, which controls the release of a whole group of hormones produced by other organs.
Forecast
Pancreatic cancer is one of the most unfavorable in terms of prognosis. This is due to the fact that this pathology progresses very quickly, without showing any signs. The consequences of surgical intervention on the pancreas cannot be accurately predicted. Surgical intervention can be prescribed only in 30-40%, and the five-year survival rate after surgery is only 50-60%. Without surgery, with palliative treatment, it does not exceed 1-2 years. And only 3-4% of patients who did not undergo surgery can overcome the 5-year survival threshold.
Causes of pancreatic cancer
Scientists do not know exactly what exactly causes pancreatic cancer - they only know the so-called risk factors that increase the likelihood of its development.
- Genetics
. The disease is more common in people whose blood relatives have already been diagnosed with a similar condition. In addition, some genetic syndromes are associated with it: - Lynch syndrome, which increases the chances of several forms of cancer in people under the age of 50; - Hippel-Lindau, leading to the formation of various benign - not dangerous, and malignant - life-threatening neoplasms; - Peutz-Jeghers, whose owners develop polyps - tissue growths - in the gastrointestinal tract. - Age
. This type of cancer can occur at any age, but mostly occurs after 55 years of age. - Toxins
. Exposure to hazardous substances used in dry cleaning or metalworking may increase your risk of developing the disease.
Those with the following health problems have an increased chance of becoming a patient of an oncologist:
- cirrhosis – degeneration of healthy liver tissue into connective tissue;
- Helicobacter pylori infections - bacteria that cause gastritis and stomach ulcers;
- diabetes mellitus – the body’s inability to transfer glucose from the blood to tissue cells;
- obesity;
- chronic pancreatitis - inflammation of the pancreas.
Some Lifestyle
can also contribute to the development of cancer:
- smoking, since smoke contains toxic substances - carcinogens, which increase the likelihood of dangerous tumors;
- excess weight;
- lack of physical activity, the absence of which disrupts the functioning of all systems and organs of the body, created by nature for movement;
- a diet high in red meat and fat, but low in fruits and vegetables;
- drinking large amounts of alcohol over a long period of time.
Symptoms and signs of pancreatic cancer
The first signs of the disease often do not appear immediately - most of them appear only after the tumor grows to a large size.
Once it becomes large enough, or its cells spread to other tissues, a person will experience the following symptoms:
- Pain.
The growing mass puts pressure on nerves and other organs, clogs the digestive tract and causes pain in the abdomen or back. - Darkening of urine.
Our body has a special liquid - bile, which is necessary for digesting food, which is produced by the liver. It is stored in the gallbladder, from there it passes into the intestines and is excreted in the feces. When cancer grows and blocks its excretory duct, too much bilirubin, a red-yellow pigment, accumulates in the body. Its excess enters the urine and turns it brown. - Weight loss.
Pancreatic cancer often deprives a person of appetite, which ultimately leads to weight loss. In addition, some types of dangerous tumors produce hormones. Hormones are substances that are created by our glands, enter various organs through the bloodstream and tell them how to act - to work or rest, to secrete something or absorb something. , making it difficult to absorb nutrients from foods, and a person loses weight, even if he follows a normal diet. - Jaundice.
The skin and whites of the eyes turn yellow due to blockage of the bile duct and the accumulation of bilirubin in the body, which stains them. - Nausea and vomiting.
Unpleasant sensations occur if the tumor affects substances involved in digestion, increases the amount of acid in the stomach, or blocks the release of partially digested contents into the intestines. - Excessive hunger or thirst.
These symptoms are signs of diabetes, a disease in which the body does not produce enough insulin to control blood sugar levels. They occur after cancer destroys the cells that produce this essential substance. - Itching.
Itching and irritation often develop due to the accumulation of excess bilirubin in the skin. - Red blistering rash.
Develops with glucagonoma, a tumor of the pancreas that leads to the production of excessive amounts of the hormone glucagon. - Enlarged gallbladder.
If the bile duct is blocked by a tumor, the flow of bile from it is disrupted, and the bladder enlarges, after which pain appears in the abdominal area. - Light or greasy stools.
The tumor disrupts the functioning of the pancreas and the release of enzymes, making fat difficult and incompletely digested. It ends up in the stool, which looks greasy and doesn't sink - it floats. The color of stool is affected by bilirubin - the less it is, the lighter the waste products. - Diarrhea.
It occurs in various types of pancreatic cancer and can be a sign of a tumor with an unusual name - VIPoma. It secretes a special substance that sends too much water into our gastrointestinal tract, the excess of which causes severe watery diarrhea. In addition, cancer often interferes with the proper absorption of what is eaten, which leads to digestive problems and diarrhea. - Swelling, redness and pain in the leg.
All these are signs of thrombosis, that is, the presence of blood clots in the vessels of the legs. Often these signs become the first dangerous symptoms of pancreatic cancer. If such a formation breaks away from the wall of the vein and enters the lung, a person experiences thromboembolism - blockage of the pulmonary artery. - Weakness, confusion, sweating and rapid heartbeat.
Such symptoms are caused by insulinomas - tumors that produce insulin, the excess of which leads to a decrease in blood sugar levels. A strong drop in its level can lead to fainting or coma - a condition in which a person loses consciousness and vital body functions are disrupted.
Pancreatic tumors
Treatment of benign tumors is only surgical: distal resection of the pancreas, resection of the head of the pancreas, pancreaticoduodenectomy, tumor enucleation. After the operation, a mandatory histological examination is carried out to clarify the type of tumor.
For malignant neoplasms, the main directions of therapy are selected based on the clinical situation. If a patient is diagnosed with a malignant carcinoid or hormonally active cancer localized in the head of the pancreas, pancreaticoduodenectomy is performed, preserving the pyloric part of the stomach. For gastrinomas, gastrectomy, selective vagotomy, and pancreaticoduodenectomy are often performed, but leading gastroenterologists and surgeons are still debating the effectiveness and appropriateness of these surgical procedures.
Complex therapy for pancreatic tumors may include radiation and polychemotherapy (with a high proliferation coefficient, active hormone synthesis, malignancy and metastasis of the tumor). Palliative treatment of malignant neoplasms aims to restore the outflow of bile and pancreatic juices, eliminate the inflammatory process in the biliary tract, and improve the patient’s quality of life. For palliative purposes, the following operations are performed: external drainage of the bile ducts according to Kerr and Halstead, percutaneous transhepatic drainage of the bile ducts, cholecystectomy, endoscopic bougienage of the tumor stricture of the extrahepatic bile ducts, endoscopic stenting of the common bile duct, etc.
Conservative therapy for benign neuroendocrine tumors with low levels of hormone production and mild manifestations of endocrine hypersecretion includes a combination of sandostatin and omeprazole. In the treatment of a tumor such as gastrinoma, a combination of H2-blockers of histamine receptors, anticholinergics and proton pump inhibitors is actively used.
Prognosis and prevention of pancreatic tumors
The prognosis for malignant tumors of the pancreas is extremely unfavorable, which is associated with their asymptomatic course and late diagnosis. Radical tumor removal is possible only in every tenth patient, in every second patient the tumor recurs, and in 95% distant metastases are detected within the first 12 months after surgery. Complex therapy does not significantly improve survival rates: within five years, no more than 5% of patients with malignant tumors of the pancreatic zone remain alive.
The prognosis for benign pancreatic tumors is favorable – in nine out of ten patients a complete cure can be achieved. In addition, benign neoplasms of this localization are casuistically rare. There is no specific prevention of pancreatic tumors, however, maintaining a healthy lifestyle, proper nutrition, and adequate rest reduce the likelihood of the formation of any tumors in the body.
Diagnosis of pancreatic cancer
It is not easy to detect the disease in the early stages, since the pancreas is located behind the stomach and cannot be felt, and in the initial stages a person has virtually no symptoms.
Diagnostics is a very important moment, because it is needed not only to detect cancer, but also to select the correct therapy. When choosing a clinic, it is advisable to give preference to an institution where there are all the necessary specialists who will carry out the necessary procedures. At Onco, you can not only undergo an examination, but also receive a full course of treatment from real professionals in their field - without queues, delays, nerves and the need to repeat tests.
The doctor begins the diagnosis with an examination - this way he can detect changes in the size of the liver, gallbladder and spleen, and in the later stages of the disease, notice the accumulation of fluid in the abdominal cavity.
If cancer is suspected, the doctor will prescribe an ultrasound
– a quick, inexpensive and safe procedure for the patient, which is not enough to make an accurate diagnosis.
If, as a result of this, the specialist is alarmed by something, he will suggest undergoing endosonography
, or endosonography - examination of the gland using a thin flexible tube inserted into the duodenum. This procedure allows you to better examine the organ, since the sensor is located quite close to it.
Blood analysis
the presence of tumor marker
CA 19-9
- a substance produced by cells in the gastrointestinal tract, indicates the presence of a pancreatic tumor - its amount increases in almost all patients with a similar diagnosis.
– computer and MRI
– magnetic resonance imaging, they provide a detailed picture in which the gland, its size and precise outlines are clearly visible. In addition, these tests are used to detect metastases - additional cancerous tumors in other tissues.
To study the condition of the ducts, the doctor prescribes cholangiopancreatography
– X-ray examination, the images of which, after the administration of a special substance, clearly show the condition of the organs.
Diagnosis is confirmed by biopsy
– studying a small part of the pancreas in the laboratory.
Thoracoabdominal department of the oncology center Lapino-2
Stages of pancreatic cancer
In total, doctors distinguish 5 stages of this type of oncology:
Stage 0:
carcinoma in situ - cancer cells are in the uppermost layers of the gland or its ducts, but they have not spread to other tissues.
1:
the size of the tumor does not exceed 4 centimeters, and it does not extend beyond the pancreas.
2:
the formation may be larger than 4 cm, nearby tissues are not affected, cancer cells are found in the three nearest lymph nodes - tiny organs of the lymphatic system that retain and neutralize dangerous substances.
3:
one or more cancerous foci of any size that are located within the pancreas or in nearby blood vessels, and at least 4 nearby lymph nodes are damaged.
Stage 4:
tumor cells have spread throughout the body and created additional formations in it - metastases. They can be found in an organ located far from the gland - for example, in the liver or bones.
Pancreatic tumor treatment:
Surgical methods:
Pancreaticoduodenal resection – removal of the head and body of the pancreas, duodenum 12, part of the common bile duct and stomach.
Tail pancreatic resection is the removal of the distal part of the pancreas along with the spleen and lymph nodes.
Palliative surgery is performed when the tumor is unresectable, its purpose is to make the person’s life easier.
Chemotherapy is the introduction into the patient’s body of chemotherapy drugs that destroy cancer cells.
Radiation therapy (radiotherapy ) is the irradiation of cancer cells with a small dose of x-rays, during which they are destroyed.
Pancreatic cancer treatment
Treatment of pancreatic cancer is not an easy task, and its success depends on many factors: the type of cancer, its stage, the patient’s age, his state of health and even personal preferences.
The goal of treatment is not always the complete removal of oncology, since this is not always possible - in advanced stages, you can only slow down its development, stop its spread throughout the body, or alleviate symptoms.
One doctor cannot cope with this task - several of them will be needed, including a surgeon, oncologist, chemotherapy, radiologist and others. You can get the necessary procedures at Onco - we have a whole team of world-class specialists who will do everything possible to defeat cancer. We guide patients “from” to “to” – from examination and diagnosis to any treatment. With us you don’t have to waste time, worry and think about where to look for help - you will receive a clear action plan, following which you will get the best result.
There are several treatment options for this type of cancer:
Surgery:
allows you to eliminate cancer cells from the body if the tumor can be detected before it has time to leave the gland. Doctors carry out 3 main types of such intervention:
- Whipple surgery
- removal of the head of the organ, part of the stomach, duodenum, lymph nodes and other tissues. - Distal pancreatectomy
- removal of the tail or body of the pancreas, and possibly the spleen. - Total pancreatectomy
- removal of the spleen and the entire gland. A person can live without them, but may develop diabetes because the body will no longer produce insulin.
Palliative surgery.
Its goal is not to treat cancer as such, but to relieve its symptoms, such as obstruction of the bile duct or duodenum. If necessary, the specialist creates an anastomosis - a channel through which bile can exit the liver, bypassing the ducts blocked by the tumor. The procedure helps minimize pain and eliminate digestive problems. Another option is to install a small stent - a spacer in the bile duct, thanks to which the passage in it remains open. When used, less tissue is damaged and it is easier to tolerate, since the surgeon makes a small incision and uses an endoscope - a thin flexible tube.
Embolization:
injection of a substance into the artery that prevents blood from reaching cancer cells. Without food and oxygen, they die and the tumor stops growing. Side effects of this procedure include abdominal pain, nausea, fever, infection and the risk of blood clots in the injection area.
Ablation:
using heat or cold to destroy cancer. The method works for formations smaller than 2.5 centimeters, and has side effects - pain, infection and internal bleeding.
Chemotherapy:
injection of toxic drugs that kill cancer cells and stop their spread. The doctor prescribes it as an independent procedure or simultaneously with other treatment methods, including to relieve symptoms in the later stages of the disease. It is carried out in cycles of 2-3 weeks with periods of rest, giving the body time to recover. Patients receiving it often experience hair loss, nausea, vomiting and constant fatigue.
Targeted therapy:
a more modern approach that stops the development of altered cells by affecting the substances necessary for their growth. Unlike chemotherapy, such drugs have clear targets - molecules that are present only in cancer tumors, due to which they have less impact on healthy tissues and the body as a whole.
Immunotherapy:
Helps the body's immune system recognize and destroy cancer cells that manage to evade and resist our natural defenses. It is given as an IV every 2-3 weeks and side effects include fatigue, cough, rash and joint pain.
Radiation therapy:
destroys or reduces formation due to exposure to radiation. The procedure is also used in later stages, and helps relieve the symptoms of the disease, as it can remove or minimize blockage of the ducts. It is given alone or in combination with other treatments, usually 5 days a week for several weeks. Patients receiving it experience skin problems, gastrointestinal disorders and fatigue, which usually improve with time.
Pancreas cancer
Pancreas cancer– a malignant neoplasm developing from the epithelium of glandular tissue or pancreatic ducts.
The most common risk factors for pancreatic cancer include:
Smoking
. People who smoke face a risk of developing pancreatic cancer twice as likely as non-smokers.
Alcohol abuse
. Alcohol abuse can lead to pancreatitis, which can ultimately lead to the development of pancreatic cancer.
Poor nutrition
. Eating large amounts of foods rich in carbohydrates and animal fats can cause gland cancer. If your diet includes enough fruits and vegetables, the risk of cancer is reduced.
Age factor
. People over the age of 60 are more susceptible to developing this disease.
Gender
. Men have a higher predisposition to pancreatic cancer than women.
Heredity
. The risk of the disease increases significantly if you have close relatives who have had pancreatic cancer.
Diabetes
. Elevated sugar levels in diabetes are one of the predisposing factors to the development of cancer.
Obesity
. Obesity itself does not cause cancer, but together with other factors it can increase the likelihood of developing cancer. The risk of pancreatic cancer in obesity depends on where the fat deposits are located. For people who have them predominantly in the abdominal area, this risk is higher.
Precancerous diseases
. Among them, special attention is paid to chronic pancreatitis, adenoma (benign tumor) of the pancreas, as well as cystic formations.
Forms of pancreatic cancer
The following types of tumors are classified by location:
- Cancer of the head of the pancreas.
- Pancreatic body cancer.
- Pancreatic tail cancer.
Pancreatic cancer is classified depending on the part of the pancreas in which the tumor formed:
- the department that produces digestive secretions (exocrine);
- the department that produces insulin and other hormones (endocrine).
Exocrine pancreatic cancer
- Adenocarcinoma. The most common form, observed in 80% of pancreatic cancer cases.
- Squamous cell carcinoma.
- Cystadenocarcinoma. Occurs during malignant degeneration of a benign cystadenoma.
- Acinar cell carcinoma. It occurs rarely (about 1.5%), most often in young people.
- Undifferentiated cancer.
Endocrine pancreatic cancer
- Insulinomas form in cells that produce insulin.
- Glucagonomas form in cells that produce glucagon.
- Gastrinomas form in cells that produce gastrin.
- Somatostatinomas are formed in cells that produce somatostatin and others.
Stages of pancreatic cancer
Stage I - a small tumor up to 2 cm in size, separated from other tissues, located in the pancreas. There are no metastases (new foci of malignant cells).
Stage II - pancreatic tumor larger than 2 cm. There are no metastases in the nearest regional lymph nodes.
Stage III - a tumor of any size, with single metastases to regional lymph nodes.
Stage IV - a tumor of any size with distant metastases.
Symptoms of the disease
Pancreatic cancer can occur without any symptoms for a long time. Unfortunately, its diagnosis occurs at fairly late stages, in which the tumor has already spread to neighboring organs and lymph nodes.
The main signs of pancreatic cancer include the following:
Pain.
Is an early symptom. Localized in the upper abdomen, as well as in the left hypochondrium. If the body and tail of the pancreas are affected, pain may radiate to the lower back or interscapular region. These pains can change in intensity with changes in body position, and they are mistakenly attributed to pain due to sciatica.
Dyspepsia.
Compression of the duodenum by a tumor is manifested by a feeling of heaviness and fullness in the stomach, even with small amounts of food eaten. Rotten belching appears; in severe cases, vomiting of food that was eaten several hours ago is added. There is a decrease in appetite, weakness, aversion to meat, fatty foods, alcohol, tobacco, coffee.
Losing weight.
Body weight decreases without any predisposing reasons.
Diabetes
. When the pancreatic islets that produce insulin are destroyed, symptoms of diabetes mellitus may appear - patients begin to complain of extreme thirst, dry mouth, itching of the skin and mucous membranes.
Jaundice.
Compression of the common bile duct leads to obstructive jaundice. The skin and urine darken, the feces, on the contrary, become light, skin itching appears, and a distended gallbladder is felt, usually painless.
Stool disorders
. A decrease in the flow of bile and enzymes into the intestinal lumen leads to impaired digestion. Diarrhea, steatorrhea (increased fat content in feces), and sometimes constipation appear. When bleeding, the stool may be “charcoal” in color.
Splenomegaly and hypersplenism.
If the tumor compresses the splenic vein, symptoms of hypersplenism may develop - anemia, leukopenia, thrombocytopenia in a general blood test, and splenomegaly - an increase in the size of the spleen.
Ascites
. This is a late symptom; its presence indicates that the peritoneum is involved in the process, or metastases have reached the portal vein.
Symptoms of endocrine tumors
Insulinoma
(tumor with insulin production). May be accompanied by the following symptoms: hand tremors, weakness, loss of consciousness, hunger, rapid heartbeat. Often even coma occurs. These manifestations occur due to a sharp drop in blood glucose.
Gastrinoma
(a tumor in which the production of gastrin is suppressed).
Accompanied by heartburn and increased acidity, a stomach ulcer appears that does not go away even as a result of treatment. The level of acidity can be determined using intragastric pH-metry
.
Glucagonoma
(the tumor produces glucagon). Accompanied by symptoms in the form of weight loss with severe thirst and increased urination. A red-brown rash also appears, the tongue becomes smooth and turns bright orange. These manifestations are explained by an increase in blood sugar.
It should be borne in mind that none of the symptoms can be called early or specific for pancreatic cancer. Therefore, any new complaints - heaviness in the epigastric region or right hypochondrium, nausea, pain in the upper abdomen or lower back, yellowness of the sclera - should be a reason for examination.
A change in the nature of chronic diseases such as pancreatitis and diabetes mellitus may indicate the addition of pancreatic cancer to them. Such conditions require immediate medical attention.
Diagnosis of pancreatic cancer
Laboratory examination methods
Certain laboratory data are important for diagnosing pancreatic cancer. With cancer of the head of the pancreas, leukocytosis, an increase in ESR, thrombocytosis, and a sharp increase in bilirubin are often observed.
A stool test can be used to evaluate the functioning of the bile ducts.
In case of cancer of the body and tail of the pancreas, a general blood test usually also shows leukocytosis, thrombocytosis, and accelerated ESR. An important marker for diagnosing cancer of the body and tail of the pancreas is an increase in lipase levels.
Cytological examination
The duodenal fluid is examined for the content of cancer cells. Detection of tumor cells in the duodenal contents confirms the diagnosis.
Instrumental diagnostic methods
Ultrasound examination (ultrasound)
- allows you to identify large formations in the pancreas, changes in the bile and pancreatic ducts.
Computed tomography (CT)
— along with ultrasound, is currently the method of choice for diagnosing pancreatic cancer. CT can detect space-occupying lesions up to 2 cm in diameter in the pancreas, as well as dilation of the bile ducts and pancreatic duct, liver metastases and extrahepatic spread of the primary tumor.
Radiography
- this study is one of the main methods that allows us to establish characteristic signs of changes in the position of the pancreas and other organs.
Endoscopic retrograde cholangiopancreatography (ERCP)
- This method allows you to perform an x-ray examination of organs from the inside. The endoscope is inserted into the duodenum, and a probe is pulled through the endoscope channel to deliver a contrast agent injected into the pancreatic and bile ducts. An image of the ducts is then obtained using X-ray equipment.
Magnetic resonance imaging (MRI)
- can be used to diagnose pancreatic tumors. Valuable is the ability to obtain a detailed image of the abdominal cavity, which makes it possible to identify metastases in the peritoneum and gallbladder, as well as the condition of the bile ducts.
Special diagnostic methods
Laparoscopy
- one of the surgical diagnostic methods that allows you to identify metastases in the liver, peritoneum, and also perform a biopsy.
Biopsy
- can be performed to clarify the stage of the disease and select medical tactics.
Pancreatic cancer treatment
The main treatment for pancreatic cancer is surgery. The extent of surgery and organ removal depends on the location of the tumor and its size. Resection can be complete (total pancreaticoduodenectomy) or partial (removal of the tail or body of the pancreas).
Palliative therapy does not eliminate pancreatic cancer completely. Treatment is aimed at alleviating the patient’s condition, reducing pain, eliminating intestinal obstruction and obstructive jaundice.
In the postoperative period, chemotherapy and radiation therapy are performed.
Chemotherapy as a separate treatment method is used only if other measures are not applicable. Chemical therapy can stop pancreatic cancer.
Doctors classify malignant neoplasms of the pancreas as category C25
in the International Classification of Diseases ICD-10.
Professional articles related to pancreatic cancer:
Kabanov M.Yu., Soloviev I.A., Yakovleva D.M. and others. The choice of the volume of minimally invasive drainage interventions in patients with cancer of the head of the pancreas // Bulletin of the Russian Military Medical Academy. 2013. 1(41). pp. 97–101.