Insulinoma
During the course of insulinoma, phases of relative well-being are distinguished, which are periodically replaced by clinically pronounced manifestations of hypoglycemia and reactive hyperadrenalineemia. During the latent period, the only manifestations of insulinoma may be obesity and increased appetite.
An acute hypoglycemic attack is the result of a breakdown in the adaptation mechanisms of the central nervous system and counter-insular factors. The attack develops on an empty stomach, after a long break in food intake, more often in the morning. During an attack, the blood glucose level drops below 2.5 mmol/l.
Neuroglycopenic symptoms of insulinoma may resemble various neurological and psychiatric disorders. Patients may experience headache, muscle weakness, ataxia, and confusion. In some cases, a hypoglycemic attack in patients with insulinoma is accompanied by a state of psychomotor agitation: hallucinations, incoherent cries, motor restlessness, unmotivated aggression, euphoria.
The reaction of the sympathetic-adrenal system to sudden hypoglycemia is the appearance of tremor, cold sweat, tachycardia, fear, and paresthesia. As the attack progresses, an epileptic seizure, loss of consciousness and coma may develop. Usually the attack is controlled by intravenous glucose infusion; however, having come to their senses, patients do not remember what happened. During a hypoglycemic attack, myocardial infarction may develop due to acute malnutrition of the heart muscle, signs of local damage to the nervous system (hemiplegia, aphasia), which can be mistaken for stroke.
With chronic hypoglycemia in patients with insulinoma, the functioning of the central and peripheral nervous system is disrupted, which affects the phase of relative well-being. In the interictal period, transient neurological symptoms, visual impairment, myalgia, decreased memory and mental abilities, and apathy occur. Even after removal of insulinoma, decreased intelligence and encephalopathy usually persist, leading to loss of professional skills and previous social status. In men, with frequently recurring attacks of hypoglycemia, impotence may develop.
A neurological examination in patients with insulinoma reveals asymmetry of periosteal and tendon reflexes, unevenness or decrease in abdominal reflexes, pathological reflexes of Rossolimo, Babinsky, Marinescu-Radovic, nystagmus, paresis of upward gaze, etc. Due to the polymorphism and nonspecificity of clinical manifestations, patients with insulinoma may be diagnosed erroneous diagnoses of epilepsy, brain tumor, vegetative-vascular dystonia, stroke, diencephalic syndrome, acute psychosis, neurasthenia, residual effects of neuroinfection, etc.
Pancreatic tumor - symptoms and treatment
The first step in planning the treatment of pancreatic tumors is to determine the morphological type of cancer and its resectability. In case of a locally advanced process, in addition to standard surgical intervention, a cyber-knife, nano-knife, stereotactic radiation therapy, proton therapy, etc. can be used.
Ductal tumors usually require extensive resections to remove all involved tissue. Partial removal of this type of cancer is impractical due to its rapid growth and progression. But for non-ductal cancer, the scope of the operation can be reduced. In some cases, partial resection of the tumor and even its complete removal (enucleation) are allowed.
First of all, the possibility of radical surgical removal of a ductal tumor depends on its relationship with large blood vessels located in this area. If the tumor is resectable, treatment begins with surgery; in other cases, chemotherapy is indicated at the first stage (possibly in combination with radiation therapy). After several courses, a repeat study is carried out. If the tumor has responded well to treatment (its size has decreased), the issue of surgical intervention is decided again.
Due to the fact that most patients with pancreatic tumors are, as a rule, elderly, treatment of this pathology is always a difficult task [9].
Surgery
As in the vast majority of cases of malignant neoplasms of internal organs, the only method of radical removal of the primary pancreatic tumor is surgery. Considering that the diagnosis is usually made at advanced stages of the disease, operations are extensive and require partial resection of adjacent organs [10]:
- When cancer is located in the head of the pancreas, not only the head is removed, but also resection of the stomach, bile ducts, duodenum and part of the small intestine is performed.
- When cancer is localized in the body or tail of the pancreas, the entire gland is removed as a single block with the tissues involved in the process. They try to save the spleen, but if this is not possible, it is also removed. Technically, this operation is simpler than resection of the head of the pancreas, but after total removal of the organ, such patients are forced to take lifelong insulin replacement therapy and enzymes.
Given the large volume of operations, plastic surgery is required after them, which is aimed at restoring the patency of the digestive system and biliary tract. After this, multi-course chemotherapy according to the FOLFIRINOX regimen is mandatory. The need for combined treatment is due to the following reasons:
- In most cases, pancreatic cancer is represented by ductal adenocarcinoma, which must be regarded as a primary generalized process, i.e. at the time of diagnosis there is reason to assume the presence of distant micrometastases.
- The cause of death after radical tumor removal is precisely distant metastases.
Chemotherapy
Chemotherapy for ductal carcinoma does not prevent either the development of relapse or the growth of metastases, but it increases the period of relapse-free survival, temporarily restraining the generalization of the process [4].
For conditionally unresectable cancer, the first stage of treatment is chemotherapy (if there is no jaundice, otherwise palliative bile drainage operations are performed).
There are several advantages to this tactic. Firstly, during treatment, a group of patients with an unfavorable prognosis is identified, in whom progression begins already during chemotherapy. In this case, further surgery is not advisable. Secondly, preoperative chemotherapy allows for a systemic effect on the body, destroying micrometastases. This has a beneficial effect on life expectancy and quality of treatment. Thirdly, preoperative therapy can be carried out in almost all patients. At the same time, after extensive operations, subsequent treatment is impossible in a quarter of patients due to the deterioration of their condition and the development of complications.
Due to the fact that pancreatic cancer is often diagnosed at late stages, the question arises of providing palliative care to such patients (palliative care implies improving the quality of life of a patient with an incurable disease). The key point at this stage may be bile drainage. For this purpose, several types of operations are carried out:
- Bypass anastomosis - an artificial “path” is formed bypassing the tumor, along which bile from the liver will enter the small intestine. This is a rather traumatic and outdated technique, but in some cases (if the tumor is “impassable” or other operations are not performed in a particular clinic for various reasons) it may be an option.
- Stenting of the bile ducts - a stent is installed into the lumen of the duct at the place of its compression, which will maintain its patency.
- Percutaneous transhepatic duct drainage - bile is drained out using drainage, which is installed above the site of bile duct obstruction.
Clinical observation
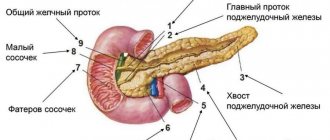
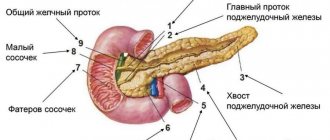
Patient Sh., 16 years old, was admitted to the Federal State Budgetary Institution Endocrinology Center due to complaints of attacks of loss of consciousness followed by retrograde amnesia, accompanied by weakness and dizziness. From the anamnesis it is known that such attacks occur for 3 months. She was examined by doctors several times at the time of the attack, but glycemia was not measured. During the next attack, loss of consciousness was recorded, and therefore the girl was hospitalized in the intensive care unit, where hypoglycemia (1.5 mmol/l) was recorded. The condition was resolved with infusion therapy with glucose solution. The child was transferred to the endocrinology department, where regular glycemic monitoring recorded low values (2.0–2.5 mmol/l). Magnetic resonance imaging (MRI) of the abdominal organs revealed a mass formation in the area of the tail of the pancreas measuring 10 × 7 × 6 mm (Fig. 1). Have you been diagnosed with pancreatic insulinoma? Hyperinsulinism.” For further examination, the child was sent to the Research Institute of Pediatric Endocrinology of the Federal State Budgetary Institution Endocrinology Center.
At the time of admission to the Federal State Budgetary Institution Endocrinology Center, an objective examination did not reveal any pathology. In the department, a fasting test was carried out, based on the results of which organic hyperinsulinism was diagnosed: after 14 hours, an increased level of insulin (31.6 µU/ml) was noted against the background of hypoketotic hypoglycemia (glycemia - 2.4 mmol/l, ketonemia - 0.1 mmol /l). Multislice computed tomography (MSCT) of the abdominal cavity - in the tail of the pancreas there is an oval-shaped formation measuring 12 × 10 mm, the density of the formation is 175 units N (Fig. 2). Conclusion: formation of the tail of the pancreas (neuroendocrine tumor, Grage I?).
Rice. 1. Magnetic resonance imaging. In the area of the posterior sections of the tail of the pancreas, a rounded lesion is determined, weakly hyperintense on T2WI, weakly hypointense on T1WI, accumulating contrast in the arterial phase, quickly washing it out, measuring 9 × 7 × 6 mm (arrow).
Rice. 2. Computer tomogram. The structure of the pancreas is heterogeneous due to the presence in the tail of an oval-shaped formation, hypercontrasting in the arterial phase, measuring 12 × 10 mm (arrow).
The girl was examined for the main biochemical and hormonal markers of the components of MEN1 syndrome, and no abnormalities were found. A molecular genetic study of the MEN1 gene was also carried out - no mutations were identified in the studied gene. In the hormonal blood test, the indicators were within the reference values: parathyroid hormone 34.58 pg/ml, IPGF-1 542.1 ng/ml, growth hormone 3.74 ng/ml, prolactin 186.1 mU/l, cortisol 150 nmol/l, ACTH 14.76 pg/ml, free T4 12.58 pmol/l, TSH 1.034 mIU/l. According to ultrasound examination of the thyroid gland and parathyroid glands, no space-occupying formations were detected. MRI of the brain showed no changes in the pituitary-sellar region. For the period of preoperative preparation, in order to prevent hypoglycemic syndrome, the girl was prescribed proglycem (diazoxide) at a dose of 100 mg/day, against which stabilization of glycemic parameters was noted. With a diagnosis of “organic hyperinsulinism. “Insulinoma of the pancreas,” the patient was transferred to Children's City Clinical Hospital No. 7 named after. BEHIND. Bashlyaeva for surgical treatment.
On July 13, 2016, the child underwent surgical intervention under endotracheal anesthesia - laparoscopic resection of the pancreas, drainage of the omental bursa. A 5-mm trocar was inserted under the umbilicus, and carboxyperitoneum was applied under a pressure of 14 mm Hg. Art. and a flow of 5.5 l/min, 5 mm optics were introduced. Additional 5-mm trocars were inserted to the right and left of the umbilicus and in the left lumbodorsal region. The stomach along the greater curvature is temporarily fixed to the anterior abdominal wall with traction sutures. The gastrocolic ligament is widely dissected. The posterior layer of the peritoneum is dissected along the upper and lower edges in the area of the tail of the pancreas. A tunnel was created behind the gland, through which a nipple catheter was passed and the gland was retracted anteriorly (Fig. 3). Using monopolar coagulation, the tail of the gland is separated from the splenic artery and vein. Using EnSeal, a transverse resection was performed at the border of the body and tail of the pancreas. The pancreatic stump is sutured with a continuous enveloping suture PDS 3-0 (Fig. 4). Changing the 5-mm trocar in the periumbilical region to a 10-mm trocar, through which the resected pancreatic fragment is removed from the abdominal cavity. The omental bursa was drained with tubular drainage through the left trocar access. The trocars have been removed. Stitches on wounds. Aseptic dressings. Operation time – 1 hour 40 minutes. Blood loss – 50.0 ml.
Rice. 3. Intraoperative photo. The pancreas is taken on a holder and retracted anterior to the splenic vessels.
Rice. 4. Intraoperative photo. Suturing the pancreatic stump with a wrapping suture using PDS II 4-0 thread.
Macroscopic examination of the resected pancreatic fragment reveals a whitish nodule measuring 1 × 1 cm with a capsule of dense consistency. Microscopic examination reveals a node of trabecular structure without growing into the capsule (Fig. 5). Outside the tumor, pronounced hyperplasia of the islets of Langerhans is observed. When conducting an immunohistochemical study, a positive reaction of tumor cells to markers of neuroendocrine differentiation is noted - with antibodies to insulin (Fig. 6), synaptophysin and chromogranin A, Ki-67 proliferation index (MIBI) - 1%. Conclusion: neuroendocrine tumor of the pancreas G1 (material was consulted by the doctor of the Department of Fundamental Pathomorphology of the Federal State Budgetary Institution ERC L.S. Selivanova).
Rice. 5. Pancreas. A clearly demarcated capsule from the tumor node. Hematoxylin and eosin staining. ×100.
Rice. 6. Pancreas. Immunohistochemical study with antibodies to insulin, positive reaction. ×400.
In the postoperative period, euglycemia was observed, which did not require additional therapy. On the 5th day, there was an increase to 150 ml of discharge from the omental bursa with an alpha-amylase content of 30,902 units/l. Along with the ongoing antibacterial therapy, octreotide (Sandostatin) 100 mcg 3 times a day was added to the treatment. From the 12th day, a significant decrease in discharge from the drainage was noted, which became serous in nature. Amylase levels in the exudate are 171 units/l. A control ultrasound of the abdominal organs did not reveal any free fluid in the projection of the pancreas. The drainage was removed on the 15th day. She was discharged on the 20th day in satisfactory condition.
results
The duration of laparoscopic operations varied from 1.5 to 2.5 hours, with an average of 2.1 ± 0.2 hours. The duration of robotic operations was slightly longer: from 2 to 5 hours, with an average of 3.1 ± 0.8 hours. This was due to the need to prepare the robotic complex. During laparoscopic operations, 4 conversions to laparotomy were made out of 10, and during robot-assisted operations, 2 out of 11. The 3D image provided by the robotic complex was clearer than during laparoscopy and more often made it possible to detect insulinoma in a superficial location. The treatment was effective in all observations; the patients showed no signs of hyperinsulinism. Histological and immunohistochemical examination of the surgical material in all patients confirmed the diagnosis of pancreatic insulinoma G1. No intraoperative complications were noted. The structure of postoperative complications is presented in the table. Among the postoperative complications, despite the prophylaxis with somatostatin analogues, acute pancreatitis predominated, manifested mainly by postoperative swelling of the gland with the formation of peripancreatic fluid accumulations and external pancreatic fistulas. To eliminate these conditions, modern minimally invasive technologies were used - percutaneous punctures and drainage of acute fluid collections under ultrasound control. The fistulas closed on their own; no repeated surgical interventions were performed for this reason. In 1 observation, due to suppuration of fluid accumulation, an abscess formed in the left subphrenic space with the development of peritonitis, which required laparoscopy, sanitation and drainage of the abdominal cavity. In 1 observation, distal resection of the pancreas was performed after conversion; the postoperative period was complicated by infected pancreatic necrosis. Traditional and minimally invasive surgical interventions were repeatedly used for treatment. As a result of this serious complication, the patient developed pancreatoprivate diabetes mellitus type 2, for the treatment of which insulin was prescribed. There were no deaths. The duration of hospital stay for patients operated on laparoscopically was 17 ± ± 3 days, for robot-assisted operations - 12 ± 2 days, for conversion to laparotomy - 39.5 ± 7 days.
Structure of postoperative complications. Note: * – complications that developed after conversions.
| Intervention | Number of observations, abs. | ||||
| Acute pancreatitis, acute parapancreatic fluid collection | Acute pancreatitis, external fistula | Acute pancreatitis, infected pancreatic necrosis | Abscess of the left subphrenic space, peritonitis | Total | |
| Laparoscopic enucleation | 2 | 1* | – | 1 | 4 |
| Laparoscopic distal resection of the pancreas | – | 1* | – | – | 1 |
| Robot-assisted enucleation | – | 2 (1*) | – | – | 3 |
| Robot-assisted distal pancreatic resection | – | – | 1* | – | 1 |
Complications
sources: pexels.com
The course of insulinoma directly depends on whether the tumor is malignant or benign. In any case, most patients experience symptoms of hypoglycemia and associated difficulty concentrating and dizziness. Later, headaches and nausea appear, which greatly reduces the quality of life of the sick. Speech or vision disturbances, hand tremors, and, as the disease progresses, muscle cramps and pain often occur.
If treatment for insulinoma , given the doctor's recommendations, is not started on time, the tumor can spread to other areas of the body. Therefore, early diagnosis and subsequent treatment are necessary. As a rule, removal of insulinoma occurs through surgery, quite easily and without complications.
Pathogenesis
β-cell adenomas, constantly releasing insulin even at low glucose concentrations, cause the development of chronic hypoglycemia . Hyperinsulinism also causes increased glycogen breakdown in the liver and muscles. Glucose is an important component of metabolism and a source of energy for all tissues, especially the brain. The brain does not have glucose reserves, so about 20% of the glucose entering the body is consumed for its function. If the supply of glucose to the cerebral cortex stops, irreversible changes develop in its cells (death of cortical elements) and cognitive and other mental disorders occur.
Hypoglycemia causes the release of catecholamines , which is manifested by weakness , anxiety , sweating , rapid heartbeat, trembling, and excitability. As a result of hypoglycemia, all types of metabolism in the brain slow down, vascular tone decreases and blood flow to the brain increases due to vascular spasm in the periphery. All this leads to the development of cerebral edema .
Treatment of insulinoma
The first step after confirmation of insulinoma is, as a rule, complete surgical removal of the tumor. Additionally, both before and after surgery, it is possible to use special medications: Octeroide and Diazoxide. They inhibit uncontrolled insulin releases.
If pathological examination of the surgical specimen confirms the malignancy of the tumor, a diagnostic search for metastases is carried out. And the patient is prescribed an individual treatment plan, consisting of chemotherapy and, if necessary, radiation.
Cost of insulinoma treatment in Germany
The full scope of therapeutic actions necessary for the patient’s recovery and rehabilitation after the disease is calculated based on the diagnostic measures used to identify the characteristics of the development of the tumor, and the actual methods of treatment: chemotherapy, radiation or surgery. All information about prices for support services during recovery and treatment, as well as for medications used during this period, are discussed with the patient as necessary, depending on the presence or absence of those studies that are used in his case.
Discussion
The use of endovideosurgical technologies for the treatment of pancreatic insulin was effective in both laparoscopic and robot-assisted interventions. The disadvantage of these operations compared to traditional ones is the impossibility of palpation inspection of the pancreas in order to localize small insulinomas. This problem can be solved by the use of intraoperative laparoscopic ultrasound. The duration of robot-assisted operations is longer compared to laparoscopic ones, which is due to the need to prepare the robotic complex. It should be noted that robot-assisted operations have a number of advantages compared to laparoscopic ones: in addition to the comfort of the surgeon and the minimal amount of work of the assistant during operations for insulinomas, ensuring optimal images using 3D technology plays a particularly important role, which allows reducing the number of conversions to search for insulinoma [ 9]. The precision of working with tissues when using a robotic complex also allows minimizing trauma to the pancreas. The greatest number of complications was observed in patients who underwent conversion due to the inability to localize insulinoma and the need for palpable inspection of the pancreas. Complications occurred least often in patients who underwent robot-assisted surgery; in this group, the results correspond to the literature data [1, 7]. We believe that this is due to the above-mentioned precision of working with pancreatic tissue, minimizing its trauma, thereby reducing the likelihood of developing postoperative pancreatitis. In the vast majority of cases, minimally invasive technologies were successfully used to treat postoperative complications.
Causes
The cause of insulinoma is the degeneration of beta cells of the islets of Langerhans. In most cases, we are talking about a benign adenoma, but in 10% of cases it is an adenocarcinoma, which often metastasizes to the liver.
How the degeneration of cells in the pancreas area and the formation of insilunoma occurs still remains unclear. Noteworthy is the significantly frequent occurrence of insulinoma in patients suffering from MEN-1 syndrome (Wermer syndrome), which manifests itself in neoplasms in the pituitary gland, pancreas and parathyroid gland.