Fistulography was done for the first time 100 years ago, filling the fistula with ordinary Vaseline and barium. Since that time, X-ray machines and contrast agents have changed, but the technique has remained “hundred-year-old.”
- What is fistulography?
- Types of fistulography
- Purpose of fistulography
- Indications for fistulography
- Contraindications
- Benefits of fistulography
- Preparation for the procedure
- How is fistulography performed?
- Decoding the results
Types of fistulography
By type, fistulography is called in accordance with the anatomical zone of the location of the fistula, if it is the esophagus, then fistulography will be called esophageal, bladder - vesical FG, in any part of the intestinal tube - intestinal FG, as well as gastric, rectovaginal, bone, and so on .
Different contrast solutions divide the type of FG into iodine-contrast and barium sulfate. Since both contrast agents are soluble in either water or oil, they are additionally marked as to whether an aqueous or oil suspension was used.
Indications for use
This technique is applicable when studying fistulas of different origins:
- esophagus;
- intestines;
- Bladder;
- biliary tract;
- gastric tissue;
- colon, small intestine, rectum;
- ears;
- skin;
- respiratory system.
Fistulography technology is used to study fistulas formed as a result of foreign body penetration. Fistulography of the bile ducts is prescribed a week or two after surgery to exclude complications in the postoperative period. X-rays with a contrast agent are also done for symptoms of purulent bone lesions. Therefore, this research is in demand in orthopedics, dentistry and traumatology.
Purpose of fistulography
Fistulography is used either to make a final diagnosis or to determine treatment tactics.
Diagnosis of superficial purulent fistulas is simple - just feel the fistula tract under the skin and press on it until the contents exit the external opening: pus, feces, urine, and so on.
X-ray examination helps determine:
- where the pathological channels come from;
- with the massiveness of the lesion;
- with the location and branching of passages;
- with the presence of hidden streaks of pus;
- involving nearby organs in the inflammatory process;
- with the volume of scar changes after inflammation subsides;
- with the presence of foreign bodies or tumor infiltration.
Detailed X-ray information allows you to choose the optimal treatment method.
Diagnostics
With fistulography you can:
- measure the length of the fistula canal;
- understand the direction of the fistula canal;
- determine the configuration of the fistula tract;
- see the presence of branches of the fistula;
- determine the location of the internal fistula opening;
- detect connections with hollow organs (intestines, bladder, vagina, urethra);
- detect the presence of pus in the fistula canal;
- see whether there is a foreign body or not, determine the relationship with it;
- find the source of the fistula - sequestration, abscess;
- identify the presence of connections between fistula canals.
The information revealed during the examination is extremely important for determining a further treatment plan.
Indications for fistulography
The indication for an X-ray contrast study is any fistula or suspicion that the inflammatory process is complicated by the formation of a fistula.
It is advisable to perform fistulography before treatment - knowledge of the structure of the lesion and the condition of the surrounding tissues in the damaged area helps to choose the optimal tactics and excise all pathological and scar tissue that impedes the healing process and causes a chronic course with relapses.
FG is not required for all fistulas; for example, with a small superficial fistula tract, before surgery it is enough to palpate it or do an ultrasound to choose the method of treatment: surgery, biological glue or tamponade.
What is fistulography?
Fistulography is an x-ray research method that allows you to detect the presence of fistulas in articular and bone tissues. In most cases, such a diagnosis is carried out during a comprehensive examination of the skeletal system, which is necessary to identify possible pathologies.
The basis for this technique is a contrast agent, which, when using X-ray radiation, can give a clear picture of the disease, the presence of fistulous tracts, as well as the severity and area of the lesion.
Content:
- What is fistulography?
- Indications for the procedure
- Contraindications for fistulography
- Types of procedure and its course
- Summing up
Using this diagnostic method, it is possible to identify the occurrence and development of the inflammatory process, the occurrence of an abscess, as well as possible foreign bodies in the tissues of the body. Fistulography also determines the direction of existing fistula tracts, which in the future makes it possible to more accurately and quickly determine the appropriate therapy.
The contrast agent for this diagnosis is most often an alcohol or oil solution of iodine. Before the examination begins, the fistula tracts are thoroughly cleaned, after which the required amount of contrast agent is injected into them, which, having passed along the entire length of the fistula, makes it possible to determine their length and direction. In some cases, for particularly sensitive patients or with severe pain, this diagnosis is carried out under local anesthesia.
This study is used primarily for complete information about the identified fistula, the duration of its course, the degree of development of the disease, as well as its location. Fistulography is also used repeatedly in case of an already identified disease to correct previously prescribed therapeutic procedures.
This study is prescribed by the attending physician, who also determines the frequency of its use. Such diagnostics are re-prescribed for those patients who have not had a positive result with the treatment methods used for a long time.
Contraindications
Contraindications are few and depend on the condition of the pathological focus and are related to the physical capabilities of the patient’s body.
Local contraindications:
- bleeding from the fistula tract;
- the location of the passage near a large vessel, the wall of which is easily damaged due to inflammatory softening of tissues;
- formation of purulent-necrotic masses against the background of acute inflammation;
- fistula as a result of the disintegration of a malignant tumor.
General contraindications:
- the patient’s serious condition due to decompensation of chronic illnesses or the terminal stage of the disease, which does not allow active therapeutic actions;
- allergy to contrast agent;
- pathology during pregnancy, when any x-ray examination is undesirable.
Advantages
Compared with previously used methods of studying fistulous tracts using the fistulography method, more information can be obtained about their features, regardless of location and size. The presence of contrast allows you to take pictures from different angles, revealing the smallest details of the formation.
The advantage of the procedure is the minimal list of contraindications. It includes intolerance to the contrast used, the presence of bleeding, disturbances in the functioning of the heart or respiratory tract, and the development of an acute infectious disease. Pregnant women are not prescribed fistulography. The restrictions also apply to patients in particularly serious condition.
If purulent discharge is observed from the fistula, this method helps to identify the source of infection. This allows you to determine the optimal course of treatment. The patient will not experience any pain during fistulography, and this is also an additional advantage of this technique. According to experts, only MRI can compete with this procedure in terms of effectiveness.
How is fistulography performed?
First, an x-ray of the damaged area is taken without contrast injection.
Anesthesia is not always necessary, since the anesthetic does not penetrate the inflammatory infiltrate.
The surgeon empties the passages as much as possible from the secretion, treats them with an antiseptic solution, then inserts the tip of the catheter into the external hole and tightly fills the passages with contrast from a syringe. The outlet is tightly clamped with a swab and adhesive tape to prevent the contrast from leaking out. Next, photographs are taken from the front and side. After the examination, the contrast agent is removed by decanting or suctioning with a syringe, the passages are washed and a clean bandage is applied.
Advantages of fistulography at the CELT clinic
In order to eliminate pain or discomfort during the procedure, and also to obtain all the data that is necessary for a full diagnosis, contact the CELT multidisciplinary clinic. We employ radiologists with over 15 years of experience who are well acquainted with all the features of fistulography. By contacting us, you can count on:
- European quality of service;
- Possibility of pre-registration and no queues;
- High diagnostic accuracy;
- The procedure is carried out by experienced diagnosticians.
You can find out the cost of fistulography in our clinic by reading the price lists or calling us: +7 (495) 788-33-88.
Decoding the results
X-ray images are developed and sent to the radiologist and operating surgeon. A joint interpretation of specialists helps to get to the clinical truth and most fully solve the previously posed diagnostic tasks, which are indicated in the section “Goals of FG”.
Patients of our clinic should not worry - no pathology will escape the attention of our specialists, the study will be carried out according to the classical canons, surgical rules and x-ray instructions.
Book a consultation 24 hours a day
+7+7+78
General characteristics of the procedure
Having become acquainted with a brief description of fistulography, we can begin to consider it further; this will help to better understand what the procedure is, tell us about the features of such diagnostics, and give an idea of its effectiveness.
Thanks to this examination, the doctor receives the most reliable information about the size of the fistula tract, its location in relation to other organs, the presence of branches and tracts. Thus, it becomes obvious that fistulography is the most effective non-invasive medical examination option that exists today. Only MRI can compete with it.
Fistulas of the rectum (chronic paraproctitis)
Symptoms, clinical course
Complaints.
Usually the patient is worried about the presence of a fistula opening (wound) on the skin in the anus, discharge of pus, ichor, which is why he is forced to wear a pad, wash the perineum or sitz baths 1-2 times a day. Sometimes the discharge is profuse and causes skin irritation and itching. Pain with good drainage of a complete fistula is rarely a concern, as it is characteristic of an incomplete internal fistula. It is caused by a chronic inflammatory process in the thickness of the internal sphincter, in the intersphincteric space and inadequate drainage when the anus is closed. Typically, the pain intensifies at the time of defecation and gradually subsides, since when the anal canal is stretched at the time of passage of the fecal lump, the incomplete internal fistula drains better.
Course of the disease. Very often the disease occurs in waves; against the background of an existing fistula, there may be an exacerbation of inflammation in the perirectal tissue. This occurs when the fistula tract is blocked by purulent-necrotic masses or granulation tissue. In this case, an abscess may occur, after opening and emptying of which the acute inflammatory phenomena subside, the amount of discharge from the wound decreases, the pain disappears, the general condition improves, but the wound does not heal completely, a wound no more than 1 cm in diameter remains, from which blood continues to flow. purulent discharge is the external opening of the fistula. With a short fistula, the discharge is usually scant; if the discharge is profuse and purulent, there is most likely a purulent cavity along the fistula. Bloody discharge should alert you to malignancy of the fistula.
During periods of remission, pain is not typical for rectal fistula. The general condition of the patient at this time is satisfactory. With careful observance of hygienic measures, the patient may not suffer particularly from the presence of a fistula for a long time. But periods of exacerbation greatly affect the quality of life. The appearance of new foci of inflammation, the involvement of the anal sphincter in the process lead to the appearance of new symptoms of the disease, a long-term inflammatory process affects the general condition of the patient, asthenia, headache, poor sleep, decreased performance are observed, the psyche suffers, and potency decreases.
Complications
The presence of a rectal fistula, especially a complex one, with infiltrates and purulent cavities, accompanied by frequent exacerbations of the inflammatory process, can lead to a significant deterioration in the patient’s general condition. In addition, severe local changes may occur, causing significant deformation of the anal canal and perineum, scarring of the muscles that compress the anus, resulting in the development of anal sphincter insufficiency. Another complication of chronic paraproctitis is pectenosis - cicatricial changes in the wall of the anal canal, leading to decreased elasticity and cicatricial stricture. With long-term existence of the disease (more than 5 years), in some cases malignancy of the fistula is observed.
Diagnosis of chronic paraproctitis
Diagnosis of chronic paraproctitis is not so difficult. Typically, patients themselves turn to the doctor with complaints about the presence of a fistula in the perineal area or purulent discharge from the anus. On external examination, if it is a complete rectal fistula, you can see the external opening. With an incomplete internal fistula, there is only an internal opening, there is no external opening on the skin.
Naturally, the examination of the patient should be preceded by the collection of an anamnesis, which clarifies the duration of the disease, the characteristics of the onset and course of the process, the frequency of exacerbations, the nature of previous treatment, and the presence of concomitant diseases is determined. During the interview, attention is also paid to the general condition of the patient (weight loss, pallor, etc.), his neuropsychic status. Information about the nature and amount of discharge from the fistula can help in the diagnosis of other diseases also characterized by the appearance of fistulas (actinomycosis, teratoid formations, Crohn's disease), suggest the presence of purulent leaks and cavities with abundant discharge of pus. It is important to ask about the functions of the intestines (constipation, diarrhea, bleeding) and anal sphincter, especially if the patient has previously undergone anal surgery.
It is better to examine a patient with a rectal fistula after cleansing the intestine of contents (enemas, laxatives). It is more convenient to examine the patient in a gynecological chair in the position of the patient on his back with his legs apart. During the examination, attention is paid to the condition of the skin of the perineum and buttocks, the distance from the external fistula opening to the anus is assessed, the location of the fistula opening around the circumference of the anus is noted, etc. Based on the location of the external fistula opening, the location of the internal fistula opening can be tentatively assumed. In this case, you need to focus on the line connecting the ischial tuberosities. If the external fistula opening in the patient's supine position is located below this line, most often the internal opening is found in the posterior crypts, but if the external opening of the fistula is located above this line, the internal opening should first be looked for in the crypts along the anterior semicircle. But there are exceptions to the rules. By the distance of the external opening from the anus, one can sometimes judge the depth of the fistula tract in relation to the external sphincter. Of course, this is not the main landmark, but nevertheless, the passage, located medially from the external sphincter or passing through a small portion of it, often has an external opening close to the anus.
Rectal fistulas due to acute paraproctitis are characterized by the presence of one external opening; if openings are found to the right and left of the anus, one should think about a horseshoe fistula. The presence of multiple external holes is more characteristic of a specific process. During examination, the amount and nature of discharge from the fistula is assessed. Ordinary (banal) paraproctitis is characterized by pus-like discharge, yellowish in color, odorless. If, when pressing on the affected area, pus is released abundantly, then there is a cavity (s) along the course of the fistula.
The tuberculous process is accompanied by copious liquid discharge from the fistula. With actinomycosis, the discharge is scanty, sometimes crumb-like, there are usually several fistula openings, the fistula tracts can be long and well palpable under the skin of the perineum and buttocks, the skin around the external openings has a bluish tint. Malignancy is quite rare. At the same time, the nature of the discharge from the fistula changes: it becomes bloody with an admixture of mucus.
During an external examination, attention is also paid to the presence of deformation of the perineum, scars, whether the anus is closed, whether it is gaping, whether or not there is maceration of the perianal skin, traces of scratching, etc. If the patient complains of poor retention of gases and feces, it is mandatory to check the reflex with perianal skin and cremasteric reflexes by marking the skin with a probe or a non-sharp needle. This is done before palpation and digital examination of the rectum.
Palpation of the perianal area and perineum allows you to determine the presence of a scar process along the fistula. When the fistula tract is located in the subcutaneous-submucosal layer, i.e. intrasphincterically, or when the tract goes through a small portion of the anal sphincter, it can be easily identified in the form of a cord from the external fistula opening to the rectum. When the fistula tract is not determined by palpation, we can say with confidence that the fistula is transsphincteric or even extrasphincteric. By palpation along the fistula, infiltrates and purulent leaks can sometimes be detected.
During a digital examination of the rectum, the tone of the rectal sphincter is determined first of all without volitional effort and during volitional compression of the anus by the patient. This data must be included in the patient’s examination protocol. The long-term existence of fistulas with exacerbations of the inflammatory process often lead to the development of anal sphincter insufficiency; previous surgical interventions can also have consequences, so this type of study must be taken very seriously. A digital examination determines the localization of the internal opening of the fistula, which is usually located in one of the Morgani crypts. Based on the location of the internal opening, the following types of fistulas are distinguished: posterior, anterior, lateral. Most often, fistulas are posterior.
It is useful to supplement a digital examination of the rectum with palpation from the perineum, i.e., conduct a bimanual examination. Digital examination can reveal other diseases of the rectum, anal canal, and prostate gland. Women undergo a vaginal examination. The presence of a fistulous tract going into the vagina and the condition of the rectovaginal septum are best judged by simultaneous examination through the rectum and vagina.
The dye test should be used in all patients with rectal fistula. For this purpose, a 1% solution of methylene blue is most often used. The paint marks the internal opening of the fistula. The staining of the crypt is best seen during anoscopy. The absence of staining of the internal opening even with the addition of hydrogen peroxide does not indicate that there is no connection with the intestine, but that there is an inflammatory process in the area of the internal opening and the passage is temporarily closed. In such a situation, the fistula tract should be washed with antiseptic solutions for several days and then the dye test should be repeated. Prescribing fistulography to identify the tract and internal opening in case of a negative dye test is inappropriate - the study is informative only if the fistula has good patency.
Probing the fistula makes it possible to judge the direction of the fistula tract, its branching in the tissues, the presence of purulent cavities, and the relationship of the tract to the external sphincter. It is better to use a buttoned metal probe. It is carefully inserted into the external fistula opening and further advanced along the way, controlled using the index finger of the free hand inserted into the intestine. Rough manipulations are inappropriate, as it is not only very painful, but also dangerous due to the possibility of making a false move.
When the fistula has a short and straight course, the probe freely penetrates the intestinal lumen. If the passage is tortuous, it is often not possible to penetrate the internal hole with a probe. If there is a purulent cavity, the probe moves. With multiple external fistula openings, all passages are usually probed.
In the presence of an intrasphincteric or shallow transsphincteric fistula, the probe goes towards the anal canal. If the fistula tract is high, then the probe goes up, parallel to the rectum. By the thickness of the tissue bridge between the finger inserted into the intestine and the probe, one can judge the relationship of the fistula tract to the external anal sphincter.
For all patients with rectal fistulas, sigmoidoscopy is required, which is needed to identify the condition of the rectal mucosa and the presence of other diseases (neoplastic diseases, inflammatory diseases, etc.).
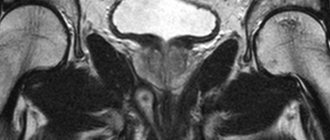
If upon examination it seems that the patient has a trans- or extrasphincteric fistula of the rectum, it is necessary to supplement the examination with fistulography. X-ray examination using a barium enema is usually used in the diagnosis of rectal fistula as an auxiliary one when it is necessary to differentiate chronic paraproctitis from other diseases.
Mentioned above was the need to assess the function of the anal sphincter, especially with long-term existence of the fistula and repeated operations for it. In this case, the most informative research method is sphincterometry.
Of course, in patients with rectal fistulas, it is sometimes necessary to conduct other additional studies if the presence of competing diseases is suspected, as well as differential diagnosis to identify concomitant diseases of other organs and systems. But the main diagnostic methods in the presence of a rectal fistula are: external examination, palpation, digital examination of the anal canal and rectum, paint test, probing of the tract, ano-, sigmoidoscopy, fistulography for high fistulas, heavy discharge and probing of the probe.
Ultrasonography provides great assistance in the topical diagnosis of the fistula tract.
Classification of fistulas
Depending on the location of the fistula tract in relation to the external sphincter of the anus, intra-, trans- and extrasphincteric rectal fistulas are distinguished.
The simplest fistulas are intrasphincteric fistulas. They are also called subcutaneous-submucosal, marginal. The fistula tract, as a rule, is direct, the cicatricial process is not pronounced, and the disease is usually short-lived. The external fistula opening is most often localized near the anus, the internal one can be in any of the crypts.
Diagnosis of this type of fistula is quite simple: palpation of the perianal area allows one to determine the fistulous tract in the submucosal and subcutaneous layers; a probe inserted into the external fistula opening usually freely passes into the intestinal lumen through the internal opening or approaches it in the submucosal layer. The dye test in patients with such a fistula is usually positive. Sphincter function is preserved. Fistulography and other additional research methods are usually not required.
Transsphincteric fistulas of the rectum are more common than extrasphincteric fistulas. Moreover, the relationship of the fistula tract to the external sphincter can be different: the tract can go through the subcutaneous portion of the sphincter, through the superficial, i.e., deeper, and even deeper - through the deep portion.
The higher the passage is located in relation to the sphincter, the more often there are not straight, but branched passages, purulent cavities in the tissue, the scarring process is more pronounced in the tissues surrounding the passage, including the sphincter.
In 15-20% of cases, extrasphincteric fistulas are observed, in which the passage is located high, as if going around the external sphincter, but the internal opening is located in the crypt area, i.e. lower. Such fistulas are formed as a result of acute ischio-, pelvio- and retrorectal paraproctitis. They are characterized by the presence of a long, tortuous course; purulent streaks and scars are often found. Often, the next exacerbation of the inflammatory process leads to the formation of new fistula openings; sometimes the inflammatory process moves from the cellular space of one side to the other - a horseshoe-shaped fistula appears. A horseshoe fistula can be either posterior or anterior.
Extrasphincteric fistulas are classified according to the degree of complexity. With the first degree of complexity of the extrasphincteric fistula, the internal opening is narrow without scars around it, there are no abscesses or infiltrates in the tissue, the course is quite straight. With the second degree of complexity, there are scars in the area of the internal opening, but there are no inflammatory changes in the tissue. In the third degree, extrasphincteric fistulas are characterized by a narrow internal opening without a scarring process around, but there is a purulent-inflammatory process in the tissue. With the fourth degree of complexity, they have a wide internal opening, surrounded by scars, with inflammatory infiltrates or purulent cavities in the cellular spaces.
In case of transsphincteric and extrasphincteric fistulas of the rectum, the examination of the patient must be supplemented with fistulography, ultrasonography, and determination of the function of the anal sphincters. These studies are necessary in order to distinguish chronic paraproctitis from other diseases that may cause fistulas.
Differential diagnosis
Rectal fistulas usually have to be differentiated from adirectal tissue cysts, osteomyelitis of the sacrum and coccyx, actinomycosis, tuberculous fistulas, fistulas in Crohn's disease, and epithelial coccygeal tract.
Cysts of perirectal tissue, related to teratomas, often suppurate and empty outward. In this case, a fistula forms in the perianal area, which must be distinguished from paraproctitis. Palpation from the skin of the perineum and digital examination of the rectum in the presence of a cystic formation allows, in the vast majority of cases, to detect a round formation of dense elastic consistency with clear boundaries. Most often, cysts are drained through a fistula on the skin and then there is no connection between the external opening of the fistula and the lumen of the rectum. At the same time, the probe and the paint do not reveal this connection - it simply does not exist. But sometimes a cyst can open simultaneously onto the skin and into the lumen of the rectum - a complete fistula occurs. In such cases, the internal opening in the intestine is located high, above the level of the crypts, while in a normal fistula it is usually localized in one of the crypts. Discharge from a cryptogenic rectal fistula outside of an exacerbation is scanty and purulent; from the cystic cavity, discharge can be abundant, mucous in nature, with crumbly inclusions, sometimes putty- or jelly-like. In the presence of a cyst, rectoscopy reveals some narrowing of the lumen and bulging of one of the intestinal walls. During fistulography, the cavity of the cyst is filled, its contour is usually clear, smooth, in contrast to ordinary paraproctitis, when when filling the leaks and cavities, the contour is uneven, the course itself is convoluted and narrow. An X-ray in the presence of a teratoma reveals an expansion of the retrorectal space. Ultrasound examination of the perirectal tissue spaces is of great help in diagnosis.
Osteomyelitis of the pelvic bones can also lead to the formation of fistulas in the perineum, sacrococcygeal and gluteal regions. In chronic paraproctitis, there is most often one external fistula opening, in osteomyelitis there may be several of them, they are usually located far from the anus, and there is no connection with the intestinal lumen. X-ray of the pelvic bones and spine allows you to make the correct diagnosis.
Fistulas with actinomycosis are usually multiple, the skin around the external openings has a bluish tint, the fistula tracts can be long and well palpable under the skin of the perineum and buttocks, the connection with the intestinal lumen is not detected. Discharge from fistulas is scanty, sometimes crumbly.
With tuberculosis of the lungs and intestines, there may also be banal fistulas of the rectum. Suspicion of a specific process is caused by cases when liquid pus is abundantly released from fistulas; histological examination reveals numerous confluent granulomas with caseous necrosis.
Fistulas in Crohn's disease occur against the background of the underlying disease as a complication. Characteristic of Crohn's disease is the presence of ulcers-fissures in the intestine, while with ordinary fistulas, inflammatory changes in the rectal mucosa are absent or minimal.
Rectal fistulas occasionally have to be differentiated from fistulas caused by inflammation of the epithelial coccygeal duct when they open close to the anus. This helps with the detection of the primary openings of the coccygeal tract and the absence of connection between these fistulas and the lumen of the rectum.
Malignancy of a rectal fistula rarely occurs; at the same time, the discharge from it becomes bloody with an admixture of mucus. A reliable diagnostic method is a cytological examination of a scraping from the fistula tract, and it is better to do the scraping from the deep part of the tract, rather than from the area of the external opening. If necessary, elements of the tract itself are subjected to histological examination.
Treatment of chronic paraproctitis
The only radical method of treating rectal fistulas is surgical, i.e. the presence of a fistula is a direct indication for surgery. Of course, there are contraindications to radical surgery, mainly severe diseases of various organs and systems in the stage of decompensation. If it is possible to achieve an improvement in the condition after conservative treatment, then surgery becomes possible.
The timing of radical surgery is determined mainly by the clinical course of the disease. In case of exacerbation of chronic paraproctitis with the formation of an abscess, it is necessary to open the abscess and only after the elimination of the purulent process operate for the fistula. It is not advisable to delay radical treatment for a long time, since the exacerbation may recur; the inflammatory process with subsequent scarring of the wall of the anal canal, sphincter and pararectal tissue can lead to deformation of the anal canal and perineum and the development of anal sphincter insufficiency. If there are infiltrates along the fistula, active anti-inflammatory therapy is carried out - antibiotics, physiotherapy, after which surgery is performed. If the process is chronic and there is no exacerbation, the operation is performed as planned. If a period of stable remission has begun, the fistula openings have closed, the operation should be postponed, since in these conditions there are no clear guidelines for performing radical intervention, the operation may not only be ineffective in relation to the fistula, but also dangerous due to the possibility of damage to tissues not involved actually into a pathological process. The operation should be performed when the fistula reopens.
The most common types of operations for rectal fistulas:
1. dissection of the fistula into the lumen of the rectum;
2. excision of the fistula into the lumen of the rectum (Gabriel’s operation);
3. excision of the fistula into the lumen of the rectum with opening and drainage of the leaks;
4. excision of the fistula into the lumen of the rectum with suturing of the sphincter;
5. excision of the fistula with a ligature;
6. excision of the fistula with movement of the mucous membrane or mucomuscular flap of the distal rectum to eliminate the internal opening of the fistula.
The choice of surgical method is determined by the following factors:
1. localization of the fistulous tract in relation to the external anal sphincter;
2. the degree of development of the cicatricial process in the intestinal wall, the area of the internal opening and along the course of the fistula;
3. the presence of purulent cavities and infiltrates in the perirectal tissue.
Surgery for rectal fistulas requires knowledge of anatomy, physiology and clinical experience. Therefore, planned treatment of patients with rectal fistulas should be carried out only in specialized hospitals and they should be operated on by specialists - coloproctologists.
Urgent operations during exacerbation of chronic paraproctitis can be performed in general surgical hospitals, but after the inflammation subsides, radical treatment should be carried out by specialists. The very high risk of complications with these interventions makes it necessary to approach the surgical treatment of rectal fistulas with caution.
The main complications after surgery are recurrence of the fistula and insufficiency of the anal sphincter. The causes of relapse can be errors in the choice of surgical technique, technical errors, as well as defects in the postoperative management of the patient.
Forecast. Surgical treatment of marginal, submucosal fistulas of the rectum, as well as low transsphincteric ones, leads to a permanent cure and is not accompanied by any serious complications. High-level fistulas (deep trans- and ex-transphincteric) can also be healed without functional impairment. In case of recurrent fistulas, long-term inflammation, the presence of leaks and cicatricial changes in the intestinal wall, sphincter and perirectal tissue, the results are much worse. Hence the rule: operations for rectal fistulas should be performed in a timely and professional manner.