Symptoms of appendiceal infiltrate
The infiltrate develops 2-3 days after the onset of appendicitis, while the clinical picture of acute appendicitis itself is erased - there is no severe pain, general health does not suffer.
Upon examination, a dense, voluminous, painful formation is determined in the right iliac region. Body temperature rises to 38.5 degrees.
Appendiceal infiltrate has two development paths - abscess formation (suppuration of the infiltrate) and reverse development with “resorption” of the inflammatory tumor.
Abscess formation of the appendicular infiltrate is manifested by an increase in the inflammatory reaction: body temperature rises to 39-40 degrees, symptoms of general intoxication appear, pain in the right iliac region intensifies.
DENSE APPENDICULAR INFILTRATE
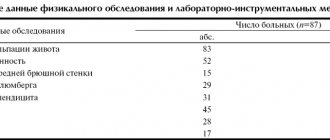
Appendiceal infiltrate (AI) is the second most common complication of acute appendicitis (AA) [1,8]. The main reasons for this are the delayed admission of patients to the surgical hospital due to diagnostic errors at the prehospital level and late presentation of patients for medical care [3]. Probably, in the foreseeable future, another reason will appear related to the enthusiasm for antibacterial treatment of uncomplicated forms of OA, when an incorrectly selected antibacterial therapy regimen will contribute to complications of OA. The relevance of the topic is due to the high mortality rate of patients with AI, reaching 10% according to various authors, and the lack of unity in treatment tactics due to a uniform approach to different periods of its course [1,2]. At the same time, AI with an unfavorable course is a morphological substrate for other complications (periappendiceal abscess, peritonitis), so its timely diagnosis and rational treatment are important. AI in its clinical course has two stages of development: early, corresponding to a “loose” infiltrate, and late, in which “dense” AI (PAI) is formed. However, not all authors focus on this division, suggesting that in case of “loose” AI (RAI), a diagnosis of local peritonitis should be made [7]. Other researchers additionally highlight AI identified in the pre- and intraoperative period [5]. In English-language literature the term AI is not used. PAI in the structure of complications of OA is less common than “loose”. Difficulties in recognizing it are due to differential diagnosis with cancer, especially in the elderly, which requires additional laboratory and instrumental studies. Various atypical positions of the vermiform appendix (AP) only complicate the diagnostic algorithm. The combination of data obtained during clinical examination and ultrasound examination (ultrasound) of the abdominal cavity is important in making a correct diagnosis. During the collection of anamnesis, clarification of the timing of the disease, and upon palpation of the abdomen, identification of a dense, moderately painful formation in the right iliac region (RIL), help to make a correct preliminary diagnosis. Ultrasound makes it possible to carry out differential diagnosis with other diseases of the abdominal organs, determine the degree of “maturity” of the infiltrate and carry out dynamic monitoring of the conservative treatment of PAI. Ultrasound criteria for PAI include: clear contours of an irregularly shaped infiltrate, with a homogeneous or hyperechoic structure, absence of fluid inclusions, a dense capsule along the periphery, without signs of abscess formation and free fluid in the abdominal cavity [4,6]. The use of other non-invasive instrumental research methods (computed tomography, irrigoscopy, colonoscopy), most often, is due to the need to exclude oncological diseases of the abdominal cavity and retroperitoneal space [9]. The use of diagnostic laparoscopy (DL) for PAI should be limited, since this procedure does not carry any therapeutic meaning. Attempts to separate dense adhesions of a conglomerate of organs are contraindicated, unsuccessful and fraught with complications. In addition, although DL is minimally invasive, it is still an operation that requires endotracheal anesthesia, installation of a trocar, and is characterized by complications both in the early and late postoperative period. We must not forget about the economic component, which increases when using DL. Thus, in the course of our ongoing study, an analysis was carried out of 36 patients with PAI who were in the Faculty Surgery Clinic named after S.P. Fedorova VMedA from 2003 to 2009. During diagnostic measures, DL was performed in 2 patients without attempts to separate the conglomerate. The reasons for performing DL in the 1st patient were an unclear clinical picture, which persisted during dynamic observation in the form of dubious peritoneal and appendicular symptoms in the absence of a palpable formation in the PPO, as well as a high level of leukocytosis with a shift to the left and the presence of a heterogeneous infiltrate with free fluid in the small area. pelvis. The performance of DL in another patient was not due to any need and was of a clarifying nature. In the remaining 34 patients, the diagnosis was established on the basis of clinical and laboratory-instrumental examination. Treatment of PAI is conservative. Includes anti-inflammatory, detoxification and antibacterial therapy, physiotherapeutic procedures. Some authors supplement treatment with immunotherapy, hyperbaric oxygen therapy, and enzyme administration. Previously, radiation therapy was used to quickly resolve the infiltrate and prevent the development of adhesions, but in modern conditions it is practically not performed. The endolymphatic method of administering antibiotics is of practical importance, in which patients recovered faster and were discharged from the hospital. Most often, a combination of metronidazole with third-fourth generation cephalosporins or aminoglycosides is used. Dynamic monitoring of conservative therapy is carried out using ultrasound, the purpose of which is to assess the size of the infiltrate and diagnose its abscess formation. Another instrumental method of monitoring treatment is irrigoscopy, performed to exclude a colon tumor or its inflammatory disease. Old age, toxic-anemic syndrome, and lack of positive dynamics during complex therapy for PAI serve as alarming signals for cancer. The above-mentioned irrigoscopy, supplemented by the determination of tumor markers, colonoscopy and CT, allows us to clarify the diagnosis. In the case of an unfavorable course of PAI, abscess formation occurs. The use of minimally invasive diapeutic treatment methods in the form of puncture or drainage of the abscess (depending on its size) under ultrasound navigation allows one to avoid laparotomy. However, a prerequisite for implementation is the presence of a diagnostic “window” to the abscess. If the course is favorable, the infiltrate resolves, the treatment period ranges from 10 to 20 days. Patients are discharged from the hospital with a recommendation to perform a planned appendectomy (EA) after 3 months. The question of the need to perform interval AE and its method (“open” or laparoscopic (LAE) remains debatable. In the Faculty Surgery Clinic of the VMedA, all patients with chronic appendicitis undergo LAE, which helps prevent the formation of adhesions in the abdominal cavity. Thus, the rational use of modern equipment - and minimally invasive methods for diagnosing and treating PAI, avoiding unnecessary laparotomy. The high visualization properties of ultrasound, its accessibility and non-invasiveness, determine great practical importance in carrying out differential diagnosis between PAI and PAI. The creation of ultrasound examination protocols in Russian hospitals will help reduce diagnostic errors However, we should not forget that the above instrumental research methods should be used thoughtfully and they only complement the clinical examination, which in PAI is highly informative.
Bibliography
1. Avanesova V.A., Ermolov A.S., Pakhomova G.V. Clinic, diagnosis and treatment of appendiceal infiltrate. Surgery.Journal named after. N.I. Pirogov. 2008; 12: 8-11 2. Varzin S.A., Ushkats A.K. Surgical tactics for acute pathology of the abdominal organs. A short practical guide. St. Petersburg: “Konus”, 2002.-128 p.; 3. Kurygin A.A., Bagnenko S.F., Kurygin Al.A, Sinenchenko G.I. Diseases of the vermiform appendix of the cecum: monograph. St. Petersburg: Indienko A.N., 2005.- 260 p.; 4. Krieger A.G., Fedorov A.V., Voskresensky P.K., Dronov A.F. Acute appendicitis. Moscow, 2002 -244 p. 5. Laipanov B.K. Differentiated approach to minimally invasive surgery for complicated forms of acute appendicitis. Abstract for the academic degree. Art. Ph.D. honey. Sci. Moscow. 2014 6. Piskunov V.N., Zavadovskaya V.D., Zavyalova N.G. Ultrasound diagnosis of acute appendicitis. Bulletin of Siberian Medicine. 2009;4:140-149. 7. Pugaev A.V., Achkasov E.E. Acute appendicitis. M.: Triada-X, 2011. -168 8. Sedov V.M. Appendicitis. SPb.: “St. Petersburg Medical Publishing House”, 2002.-232 p.; 9. Paulson EK, Coursey CA, CT protocols for acute appendicitis: time for change. AJR Am J Roentgenol. 2009 Nov; 193(5) 1268-71
Treatment of appendiceal infiltrate
Abscess formation of the infiltrate is an indication for emergency surgery. In the absence of abscess formation, conservative therapy is carried out in a hospital setting, followed (after 2-3 months) by a planned appendectomy.
Essential drugs
THERE ARE CONTRAINDICATIONS. CONSULT YOUR DOCTOR.
- Ceftriaxone (an antibiotic of the third generation cephalosporin group). Dosage regimen: IM, IV, adults and children over 12 years of age, the average daily dose is 1-2 g of ceftriaxone once a day or 0.5-1 g every 12 hours. In severe cases or in cases of infections caused by moderately sensitive pathogens, the daily dose can be increased to 4 g.
- Cefepime (IV generation cephalosporin antibiotic). Dosage regimen: adults and children weighing more than 40 kg with normal renal function 0.5-1 g intravenously (for severe infections up to 2 g) or deep intramuscularly at intervals of 12 hours (for severe infections - after 8 hours ).
- Metronidazole (antiprotozoal, antibacterial agent). Dosage regimen: IV for adults and children over 12 years of age, a single dose is 0.5 g. The rate of IV jet or drip administration is 5 ml/min. The interval between injections is 8 hours.
- Amoxiclav (broad-spectrum bactericidal antibacterial agent). Dosage regimen: intravenously, adults and children over 12 years of age or weighing more than 40 kg - 1.2 g of the drug (1000 + 200 mg) with an interval of 8 hours, in case of severe infection - with an interval of 6 hours.
- Tienam (antimicrobial, bactericidal, antibacterial agent). Dosage regimen: IV, by infusion: ≤ 500 mg - over 20-30 minutes, > 500 mg over 40-60 minutes. The average daily dose is 2000 mg (4 injections). The maximum daily dose is 4000 mg (50 mg/kg). The dose is adjusted taking into account the severity of the condition, body weight and renal function of the patient.
- Vancomycin (antibacterial, bactericidal agent). Dosage regimen: adults, 0.5 g intravenously every 6 hours or 1.0 g every 12 hours. Infusion duration is at least 60 minutes, rate is 10 mg/min.
Diagnostics
Diagnosis of appendiceal infiltrate is carried out in three stages. First, the abdomen is palpated and the patient is interviewed. This is usually enough to make a diagnosis. To confirm it, a blood test is done, which should confirm the presence of inflammation in the body. If the infiltrate cannot be palpated upon palpation (this may be due to the incorrect position of the appendix) or the tests give an atypical picture of the disease, further examination with X-ray or MRI is prescribed. These methods allow a more accurate diagnosis to be made. All tests are carried out very quickly, as there is a risk of abscess of internal organs.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0.01 | 2 | 2 | 2 | 2 | 2 | 2 | 0.01 | 2 | 2 | 2 | 2 | 2 | 2 |
Treatment
Appendiceal infiltration is treated depending on the stage of the disease. If it was detected early, most doctors now prescribe conservative treatment. It consists of taking anti-inflammatory drugs, bed rest and a light diet. Usually these are boiled purees or porridges that do not cause excessive peristalsis. Body temperature is measured regularly so as not to miss the moment if the disease suddenly progresses to an acute stage. Under no circumstances should you take painkillers, as this blurs the picture of the disease. If purulent pockets are detected in the infiltrate, surgical intervention is performed, since at this stage independent healing is no longer possible.
Infiltrate
Infiltrate is the accumulation in the tissues of the body of cellular elements that are unusual for this area, as well as blood and lymph. Its formation is accompanied by an increase in tissue volume, it becomes denser, changes color, and pain is felt at the site.
Treatment and prognosis of this condition depend on the type and cause of its occurrence:
- Inflammatory infiltrate.
- Its development is caused by injury and the spread of infection. Infiltrates can be intramuscular, subcutaneous, and they also form in the chest and abdominal cavity.
- An inflammatory infiltrate is an effusion of blood cells into the tissue. When an infection occurs, it becomes purulent. In addition to suppuration with the formation of phlegmon and abscess, the infiltrate can resolve, sclerosis, or heal with the formation of a scar.
- Tumor infiltrate.
- It develops with the invasive growth of a tumor, when tumor cells grow into healthy tissue, gradually destroying it.
In medicine, there are several more varieties of this condition.
Pulmonary
It is an accumulation of various cells in the lung tissue. In this case, the tissue becomes denser, increases in volume, and the functioning of the respiratory system becomes more difficult. The reason for the formation of lung infiltrate is the penetration of infection and parasites (ascariasis), tumor development, and an allergic process.
To determine pathology, X-ray examination plays a decisive role. Blood tests are also prescribed to determine the nature of the disease and possible pathogens.
Treatment depends on the cause of the pathology. Therapy is prescribed by a pulmonologist.
Postoperative
Infiltration after surgery is a complication resulting from surgery. The cause of the development of pathology is infection and tissue trauma.
Also, the occurrence of infiltrates is facilitated by impaired blood circulation in the area of intervention and reduced resistance to infections in the postoperative period.
The pathology develops gradually. It is detected in the first or second week after surgery. A person’s temperature rises, pain appears in the abdominal area, and stool retention occurs. In the area of intervention, the doctor determines a painful lump.
Infiltrate is dangerous because it stops the healing of the postoperative wound and causes it to fester, so immediately when it is detected, the surgeon prescribes antibiotic therapy.
Post-injection
Pathology develops at the site of subcutaneous or intramuscular injections. Most often, infiltration occurs after injections into the gluteal muscle: pain appears, and a compaction is detected on palpation. The skin turns red, the temperature rises to low-grade levels.
The cause of development is a violation of the rules for administering injections (blunt needles, rapid administration of the drug, frequent injections into the same area, failure to comply with asepsis rules).
To treat infiltration, local agents (iodine mesh), physiotherapy methods (electrophoresis), UHF and antibiotic therapy are used.
Appendiceal infiltrate
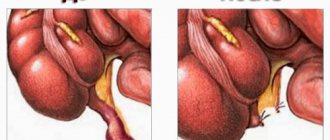
This is a complication of acute appendicitis, which manifests itself in the form of tissues of the appendix fused together with organs located nearby (cecum, small intestine, omentum).
The formation forms 2–5 days from the onset of the disease. After the formation of the infiltrate, acute pain in the right iliac region is replaced by dull and aching pain. Inflammation is also detected in the blood (increased ESR, leukocytosis). The temperature rises to low-grade levels. Over time, the seal may fester or resolve. The formation is treated conservatively: the doctor prescribes antibiotics and physiotherapeutic procedures. After 2 months, a planned appendectomy is performed.