The frequency of complaints of constipation and other problems with bowel movements increases significantly in older people. They may tell family members that their stool is very hard, that straining is painful, or that the process is too slow and intermittent. These symptoms often significantly impair quality of life and require intermittent or continuous use of laxatives.
The most complete information on the incidence of constipation in older people is from the United States. It occurs in 36-45% of the population over 65 years of age. In more than half of cases, symptoms require drug treatment. It has been found that complaints of constipation become more frequent in the presence of chronic diseases (diabetes mellitus, depression and arterial hypertension).
Causes
The reasons for the increase in constipation in older pensioners have been well studied.
First of all, these are the features of the diet. It has been established that nutrition for constipation in the elderly is often inadequate, since the proportion of products of plant origin decreases. At the same time, appetite decreases, which is why older people eat less food. The second aspect of the problem is a decrease in physical activity. Chronic disorders, joint problems, and forced bed rest inhibit the motor activity of the gastrointestinal tract, which provokes the development of constipation.
Physiological changes in the lower rectum also play an important role. With age, the muscle fibers of the walls are gradually replaced by connective tissue. This can be facilitated by pathologies of the anorectal area: proctitis, hemorrhoids, anal fissure, ulcerative colitis.
Doctors have noted that the likelihood of the disease increases in citizens with heart failure, diabetes mellitus and neurodegenerative disorders (Alzheimer's disease, Pick's syndrome). The progression of these diseases leads to disruption of the neuronal regulation of the digestive system.
Also, the appearance of constipation can be caused by taking medications of various groups:
- antacids;
- iron supplements for anemia;
- antibacterial drugs (cephalosporins, macrolides, fluoroquinolones);
- thiazide and loop diuretics;
- neuroleptics;
- tranquilizers;
- narcotic analgesics.
A dangerous prerequisite for increased constipation in older people is the development of colorectal cancer. This malignant neoplasm is one of the most common causes of death from cancer in the world. In addition to difficulty defecating, the progression of cancer is usually accompanied by weakness, loss of body weight, the appearance of blood in the stool and the development of anemia.
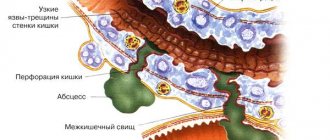
Inflammatory diseases of the gastrointestinal tract can also provoke problems with stool. At older ages, the likelihood of detecting Crohn's disease, ulcerative colitis and proctitis increases. In such cases, in addition to constipation, other symptoms can be found: abdominal pain, decreased appetite, increased body temperature, and “inflammatory” changes in the blood.
Laxatives to relieve constipation
Mild laxatives are often prescribed as first aid for constipation in older people. They allow you to get rid of unpleasant sensations and nagging pains that arise due to problems with stool. Existing laxatives usually contain the following components that help combat constipation:
- agents that can cause chemical irritation of the intestinal receptor apparatus. These include senna, rhubarb, gutallax, phenolphthalein, castor oil, etc.;
- agents that can inhibit water absorption. This group includes sodium sulfate, magnesium sulfate, Carlsbad salt, etc.;
- drugs that help increase the volume of intestinal contents. These are bran, agar-agar, methyl cellulose, seaweed;
- means that soften stool. These include vaseline and almond oils, liquid paraffin, etc.
Up to contents
Symptoms and diagnosis of constipation
In the medical sense, the word “constipation” combines various symptoms that are accompanied by a deterioration in the quality of bowel movements. Many people may perceive them differently, which makes diagnosing this condition difficult.
Doctors now use the Rome III criteria for diagnosing functional bowel diseases. According to these recommendations, constipation is defined as a decrease in the frequency of bowel movements less than 4 times a week. At the same time, older people may complain of:
- frequent, prolonged and painful straining during bowel movements;
- hard consistency of stool;
- regular feeling of incomplete bowel movement of the rectum;
- the need for mechanical removal of feces using enemas;
- feeling of a “plug” in the lower abdomen;
- loose stools only after taking laxatives;
- feeling of heaviness in the lower abdomen.
To make a diagnosis of chronic functional constipation, it is necessary that the symptoms bother the patient for at least 3 months over the past six months. The doctor must also exclude the presence of organic pathology (for example, inflammation or tumor).
These symptoms usually develop gradually. Their severity can vary significantly depending on diet, physical activity and certain medications. Therefore, they usually turn to outsiders for help only when bowel retention seriously affects daily life.
Often this disease is the first symptom of dangerous disorders of the digestive system (for example, cancer or ulcerative colitis). Therefore, all adult patients who seek medical help are recommended to undergo an endoscopic examination (colonoscopy) and/or computed tomography with contrast injection. This allows us to exclude tumors and active inflammatory process.
Symptoms of constipation in older people
Constipation is a disorder of intestinal function, which is manifested by the following symptoms:
- an increase in the time intervals between acts of defecation compared to the individual physiological norm;
- difficulty in defecation (even while maintaining normal stool frequency);
- systematic insufficient bowel movement.**
It is worth remembering that normal indicators of the frequency of bowel movements vary from person to person, and if a person goes to the toilet quite rarely, but this does not cause him discomfort and does not leave a feeling of incomplete bowel movement, it may be premature to talk about constipation.
Up to contents
Modern treatment of constipation
Treatment of functional constipation always begins with nutritional correction. Patients are advised to increase the proportion of fiber products in their diet, drink at least 1.5 liters of fluid per day (unless they have heart or kidney failure), and increase physical activity. Gymnastics or other active exercises for bowel retention should last at least 45 minutes a day. These simple recommendations allow 30-40% of people to get rid of the problem.
Your doctor will tell you how to get rid of constipation in old age that arose after the prescription of a new medicine. During a second consultation, the specialist will change the medication (if it has available analogues) or completely cancel it.
Certain physical exercises also make defecation easier. For example, it is recommended to massage the front wall of the abdomen in a clockwise direction, repeat drawing in the abdomen while inhaling, or purposefully compress and relax the otkhodnik. The duration of the exercises should be 5-7 minutes.
Attention is also paid to the correct position during bowel movements. To speed up the process of bowel movements, it is recommended to slightly bend your torso forward. In this case, it is advisable to bend your legs as much as possible at the knees and hip joints.
Due to its high prevalence, constipation today is considered a socially significant disease. In developed countries, the incidence of constipation in the population ranges from 10 to 17–19% [1–3]. This is due to the fact that over the past 100 years the nature of nutrition has changed, the amount of dietary fiber consumed in the diet has decreased and physical activity has decreased.
The frequency of stool in healthy people varies and depends on the nature of nutrition, lifestyle, and habits. Temporary retention of stool should not in all cases be considered as a sign of any pathological condition. However, the occurrence of constipation in middle-aged or elderly people should primarily cause oncological alertness.
According to E.K. Hammad, G.A. Grigorieva, after excluding cases of constipation associated with lifestyle characteristics, the anatomical features of the colon dominate among the causes of chronic constipation (CS) in the age group under 20 years; at the age of 20–40 years – pathology of the anorectal zone; after 40 years, psychogenic, neurogenic, endocrine, gastroenterological causes of constipation and causes associated with pathology of the anorectal zone are equally common [4].
According to the definition, constipation (obstipation, constipation (lat.) - pressed, crowded together) should be considered a delay in bowel movement for more than 48–72 hours, accompanied by difficulty in defecation, a feeling of incomplete evacuation with the passage of a small amount (less than 100 g) and increased stool hardness (types I or II on the Bristol scale). Some authors consider fecal weight less than 35 g/day to be an objective criterion for constipation [5].
The problem of constipation worsens with age, and among people over 60 years of age, constipation occurs in 50–60% [6]. According to the MUSA population study, 34.3% of respondents gave an affirmative answer to a direct question about constipation; only 16.5% of them met the Rome criteria. The frequency of constipation increases with age and is 3.6% in the group from 18 to 24 years old, 7.5% from 25 to 34 years old, 15.8% from 35 to 44 years old, 17.8% from 45 to 54 years old, from 55 to 64 years old – 21.5, over 65 years old – 32.8% [1]. In elderly and senile patients with multimorbidity, the presence of constipation aggravates the course of both concomitant pathology of the gastrointestinal tract (GIT) and other organs and systems. In the work of O.B. Yanovoy et al. it has been proven that constipation is one of the three main factors that increase the risk of developing reflux esophagitis (relative risk [RR] = 1.65 with 95% confidence interval [CI] 1.05–2.6; p = 0.02) , and elimination of constipation in patients with gastroesophageal reflux disease leads to a decrease in the frequency of taking proton pump inhibitors (in the “on demand” mode) in 23.1 versus 2.5% of patients with persistent constipation (p <0.05) [7].
According to one large review, the decrease in quality of life in chronic diseases is comparable to that in patients with coronary heart disease, bronchial asthma, and chronic inflammatory-dystrophic diseases of the joints [8]. Severe constipation increases the risk of cardiovascular events in older postmenopausal women by 23% (RR=1.28, 95% CI – 1.08–1.53), and moderate constipation by 1.13 times (95% CI – 1.03 –1.24) [9].
Another problem for patients in older age groups with multimorbidity is forced polypharmacy. Some medications can cause intestinal motility problems. These include tricyclic antidepressants, antiparkinsonian (anticholinergic, dopaminergic) drugs, antacids containing aluminum hydroxide or calcium carbonate, M-anticholinergics, analgesics (codeine, morphine and its derivatives), antitussives, which include codeine and its derivatives, diuretics ( torasemide, saluretics), some representatives of antihypertensive drugs: angiotensin-converting enzyme inhibitors, verapamil, clonidine, antibiotics (cephalosporins, etc.), ferrous and trivalent iron preparations. The effect on intestinal motility depends on the dose and duration of use of the drug.
Sometimes, even when interviewing the patient, it is possible to determine whether the constipation is primary, i.e. when morphological changes in the colon are not detected or a symptom of organic damage to the gastrointestinal tract, and in some cases a manifestation of extragastrointestinal diseases. Diseases that may cause constipation are presented in the table.
When collecting an anamnesis, the doctor must establish how long ago the complaints began, find out the nature of stool in childhood and try to trace a possible connection between constipation and a change of place of residence, diet, etc. A short medical history, onset of the disease after 50 years of age, loss of body weight for no apparent reason, episodes of fever, family history (for the presence of malignant tumors), intestinal bleeding or a positive stool test for occult blood, anemia, leukocytosis, accelerated ESR) are indications for in-depth examination of the gastrointestinal tract, primarily esophagogastroduodeno- and colonoscopy.
Since the risk of colorectal cancer increases after 50 years, this category of patients also requires a detailed examination of the intestines.
Chronic disease can be primary or secondary. Constipation is considered primary, or functional, if its cause cannot be associated with morphological changes in the intestine.
Secondary constipation develops due to diseases of the colon, pharmacological and nutritional influences that cause disturbances in its structure and motility. From the point of view of the pathogenesis features, chronic diseases are divided into three options:
- constipation due to intestinal dyskinesia (functional constipation and irritable bowel syndrome (IBS) with a predominance of constipation;
- constipation due to slow movement of intestinal contents through the colon (inert colon);
- constipation due to impaired coordination of the muscular system that provides defecation (dyssynergic defecation), which accounts for up to 25% of the total number of functional constipation [10].
In 2006, the Rome Criteria (Rome III) for functional gastrointestinal disorders formulated the criteria for the diagnosis of chronic functional constipation, which has the International Classification of Diseases code K 59.0 [11, 12].
To make a diagnosis, at least two of the following criteria must be present for at least 3 months, with onset 6 months before diagnosis:
- straining during at least 25% of bowel movements;
- rough or hard stools in at least 25% of bowel movements;
- a feeling of incomplete evacuation in at least 25% of bowel movements;
- sensation of anorectal obstruction/blockage for at least 25% of bowel movements;
- need for manual techniques to relieve at least 25% of bowel movements (eg, digital evacuation, pelvic floor support);
- less than three bowel movements per week;
- inability to pass stool independently without the use of laxatives;
- insufficient criteria for IBS.
The main criterion for the diagnosis of IBS (K 58), which fundamentally distinguishes it from chronic functional constipation, is the presence of abdominal pain or discomfort associated with defecation and/or changes in the frequency and/or shape of stool.
Treatment of constipation
Treatment should begin with recommendations for lifestyle changes. However, for patients of older age groups this is not an easy task.
Increasing the amount of dietary fiber in the diet. The recommended intake is 25–32 g/day, which corresponds to approximately 400–450 g of vegetables and fruits. To prevent or reduce excess gas formation in the intestines, the patient’s attention should be focused on gradually (over several weeks) increasing the daily intake of vegetables and fruits. Heat processing of food also helps reduce gas formation.
Take a sufficient amount of fluid (on average at least 1.5 l/day).
Physical activity. For example, a daily 30-minute brisk walk.
Forming the habit of daily bowel movement at the same time (more physiologically in the morning - after breakfast, which triggers the gastroileal Porges symptom: rapid movement of the contents of the ileum into the cecum when the gastric mucosa is irritated by food) in the patient’s usual conditions.
Already at the stage of dietary recommendations, the patient can be prescribed bran. The amount of bran should be increased from 1–2 teaspoons to 6–8 tablespoons over 2–4 weeks [13].
Bran can serve as an example of the principle of rational pharmacotherapy for elderly and senile patients, namely multi-purpose monotherapy, i.e. the ability to use the systemic effects of one remedy for the simultaneous correction of impaired functions of several organs or systems (L.B. Lazebnik, 1993).
As basic therapy, each patient with chronic functional constipation should be prescribed substances that increase the volume of intestinal contents (methylcellulose, bran, flax seed, etc.), because the combination of these substances with other groups of laxatives has a synergistic effect, which makes it possible to increase the effectiveness of constipation therapy.
The use of magnesium sulfate, castor oil, aloe, and senna as laxatives is mentioned in Egyptian papyri and documents of Ancient Greece, incl. and in the Aphorisms of Hippocrates.
When prescribing laxatives, it is necessary to remember that with their long-term (over 6-12 months) use, psychological dependence and, along with this, the phenomenon of addiction can develop.
Classification of laxatives by mechanism of action
Causing chemical irritation of receptors: anthraquinones (derivatives of senna, buckthorn), diphenols (bisacodyl, sodium picosulfate), castor oil.
Having osmotic properties: salts (magnesium sulfate), weakly absorbed di- and oligosaccharides (lactulose), polyhydric alcohols (sorbitol), polyethylene glycol.
Increasing the volume of intestinal contents: ballast substances (methylcellulose, bran, flax seed, psyllium, etc.)
Helping soften stool and improve its slip (liquid paraffin, petroleum jelly).
A study conducted in Russia in 2011 by IPSOS and business analytics when studying the constipation therapy market showed that 67% of people suffering from constipation are treated independently, based on recommendations from the Internet, neighbors and popular scientific publications, 13% seek advice from pharmacist, 11% are not treated at all and only 13% seek help from a doctor. Before contacting a doctor, 70% of patients had already tried various methods of therapy [14].
According to J. Tack et al., the level of dissatisfaction with the effects of laxatives both in our country and in other countries is about 47% [2]. This may be due to the following reasons: the lack of an integrated approach to the treatment of constipation, the patient’s lack of understanding of the need to regularly adhere to the selected regimen and the desire to get a quick effect.
When prescribing a drug to treat constipation, the doctor must clearly understand the purpose of the prescription and the expected duration of treatment.
Irritating drugs are effective for the treatment of “traveler’s constipation” (no more than 7 days), but cannot be recommended as monotherapy to normalize stool in patients with chronic functional constipation, because With long-term use, addiction quickly develops.
Osmotic laxatives: polyethylene glycol, polyhydric alcohols (sorbitol), saline laxatives (magnesium sulfate), act only in the intestinal lumen, without causing systemic side effects. By binding water in the intestinal lumen, they increase the volume of intestinal contents and thereby stimulate peristalsis. These drugs are highly effective and can be prescribed for periods ranging from several weeks to several months.
Poorly absorbed di- and oligosugars (lactulose) have prebiotic properties and, due to the growth of saccharolytic bacteria in the intestine, change the intraluminal pH, increasing the osmotic pressure in the intestinal lumen. This causes an increase in the volume of intestinal contents and stimulates propulsive intestinal motility.
Common disadvantages of these drugs include bloating and rumbling. These side effects can be overcome by individually selecting the dose and gradually increasing it.
Vaseline oil (Oleum vaselini seu Parafinum liquidum, “liquid paraffin”) helps soften stool, facilitate its sliding through the intestine and has a weak stimulating effect on intestinal motility. Used orally once a day, 1-2 tablespoons, 2 hours after meals. The duration of therapy is no more than 5 days, because Long-term use of petroleum jelly can cause malabsorption of fat-soluble vitamins A, E, K, as well as intestinal atony. Please note that due to irritation of the mucous membrane of the rectum and anal canal, for elderly and senile patients, when taking petrolatum oil orally, the risk of fecal incontinence and incontinence may increase.
Below are the results of a meta-analysis of 31 studies (808 patients were examined) that compared the effectiveness of different groups of laxative drugs [15] (see figure).
In the absence of effect when taking all the previously listed laxatives as mono- or combination therapy, the drug of choice remains the full agonist of type 4 serotonergic receptors (5-HT4) prucalopride, which has a pronounced laxative effect in 73% of patients at a dose of 2 mg [ 20]. This drug activates 5-HT4 receptors located in smooth muscle and neurons of the neuromuscular plexus in the intestinal wall, which leads to increased peristalsis by stimulating second messengers (acetylcholine and calcitonin), contraction of proximal smooth muscle fibers and relaxation of peripheral smooth muscle fibers. The pharmacokinetics of prucalopride has a direct correlation with the dose in the range of up to 20 mg/day.
With long-term use of the drug once a day at a dose of 2 mg, addiction does not develop. Unlike its predecessor tegaserod, prucalopride in therapeutic doses does not have side effects on the cardiovascular system in the form of the development of life-threatening arrhythmias.
Taking into account the principle of multi-target monotherapy to stimulate the functioning of the colon, it is possible to recommend taking drugs that do not belong to the group of laxatives. Such a drug is the opioid receptor blocker trimebutine, which reduces the duration of colonic transit from 105±19 to 60±11 hours versus placebo (from 103±17 to 95±10 hours), p<0.001, increasing the electrophysiological activity of the intestine in patients with chronic idiopathic constipation with dosage of 100–200 mg 3 times a day [16].
There is currently insufficient evidence to support the effectiveness of using non-absorbable antibiotics and probiotics to treat constipation. Only a few studies have shown that Bifidobacterium animalis can accelerate colonic transit in both healthy people and patients with IBS, and Lactobacillus casei and Bifidobacterium lactis DN-173010 are effective for chronic constipation [17‒19].
The problems of constipation in old age include a decrease in the pain threshold [19], a decrease in serotonin levels and the frequent development of depression. Taking into account the direct correlation of the development of constipation against the background of major depression, recommendations for the management of such patients from the point of view of a psychosomatic approach have been developed [20].
According to N.P. Chernus et al. [21], anxious and asthenic depression were most often associated with a more severe variant of functional constipation. The addition of an antidepressant to standard therapy improved the psychoemotional state of patients with functional constipation and achieved long-term remission.
Successful treatment of constipation at any age, incl. and in patients of older age groups, is to establish the causes of occurrence and the correct choice of treatment program.
Exercises
If organic pathology is excluded, special exercises can be used to treat constipation. Such exercises are aimed at strengthening the abdominal muscles and improving blood supply to internal organs.
| Initial position | How to do | |
| 1 | Standing, feet shoulder-width apart, hands on waist. | Perform circular movements with your torso. |
| 2 | Lying on your back. | Raise your legs bent or straight. |
| 3 | Lying on your back. | Perform circular movements with your legs, imitating riding a bicycle. |
Also, for the treatment and prevention of constipation, it is useful to walk more, swim, and do yoga.
Diet
Diet plays an important role in preventing constipation. It is necessary to develop a diet: eat food at the same time, 5-6 times a day in small portions. It is not recommended to grind food or frequently prepare purees and jelly. It is better to boil or steam foods.
You should exclude from your diet foods and drinks that slow down bowel movements and cause increased gas formation:
- bread and pasta made from premium flour;
- baked goods;
- rice and semolina porridge, lentils;
- smoked meats;
- strong tea, coffee and cocoa;
- whole milk;
- beans and peas.
Eating foods that stimulate peristalsis and provide a laxative effect will help combat constipation:
- Foods that contain a lot of fiber: beets, zucchini, carrots, cucumbers, pumpkin, apples, pears, apricots, plums, black currants, gooseberries.
- Buckwheat and oatmeal, bread and pasta from durum wheat, bran.
- Dried fruits: prunes, dried apricots, raisins, figs.
- Vegetable oils that improve intestinal motility: sunflower, olive, corn, flaxseed.
- Fermented milk products that have a laxative effect: kefir, yogurt, fermented baked milk.
In the presence of tumor formations, diseases of the stomach and intestines, it is not recommended to consume a lot of fiber, as this can lead to the formation of a fecal impaction.