The lymph nodes of the abdominal cavity are a large group of lymph nodes that provide lymph flow to the organs of this area. For a number of different reasons, these nodes can become enlarged and inflamed. Due to their deep location, the lymph nodes in the abdominal cavity are not palpable, so a pathological process can be suspected by indirect symptoms. It is important to know the localization and function of the lymph nodes in the abdomen in order to promptly pay attention to the body’s alarm signals and consult a doctor.
1.General information
Lymphocytes are one of the most important immune factors, which are a type of white blood cells (leukocytes). The main task of lymphocytes is to remember (immune memory) and destroy foreign, infected, mutated cells, including tumor cells. An increased level of lymphocytes in the blood in the absence of clinical manifestations of infection - or any other symptoms - is considered as a possible early sign of the oncological process. However, in some cases the concentration of lymphocytes themselves increases malignantly; multiplying chaotically, uncontrollably and inadequately (in relation to the internal situation in the body), they accumulate in the lymph nodes and other organs, which leads to the development of a specific clinical picture.
This kind of pathology of the lymphatic system is designated by the collective term “lymphoma” and includes a group of rare hematological diseases. There are two histologically and clinically different types of lymphomas: Hodgkin's lymphogranulomatosis (accounts for no more than one percent of the total volume of registered oncopathology) and the so-called. non-Hodgkin's lymphoma, which occurs much more often than the first type (about 70% of all malignant lymphomas).
Intestinal lymphoma, therefore, is one of the types of lymphoma, which is characterized by a pathologically rapid, progressive accumulation of lymphocytes mainly in the intestine. From a statistical point of view, intestinal lymphoma is less common than any other localization option, and is almost always of the non-Hodgkin type.
A must read! Help with treatment and hospitalization!
Features of the abdominal lymph nodes
The main feature of the abdominal lymph nodes is their location. Mesenteric lymph nodes are located in the peritoneum, so they cannot be palpated. They ensure the drainage of lymph from the abdominal organs, protecting against infection, removing toxins and ensuring the normal functioning of the immune system.
With inflammation of the abdominal lymph nodes, it is difficult to make a diagnosis on your own. This is due to the fact that the symptoms are more reminiscent of an intestinal infection or flu with dyspeptic disorders. Children under 12-13 years of age are more likely to experience inflammation of the lymph nodes of the abdominal cavity and retroperitoneal space than adults, which is explained by the weak immunity of the child’s body.
Having understood what mesenteric lymph nodes are, we should take a closer look at their location and functions. Pathologies of this group of lymph nodes are dangerous due to complications. In addition, this group of lymph nodes reacts sharply to oncological pathologies of internal organs, so it is important to be able to identify dangerous symptoms in a timely manner, but not to brush off the discomfort, expecting that it will go away without treatment.
Location and functions
Symptoms of the acute stage increase over 1-5 days depending on the person’s immunity; in young children it develops within a few hours
The location of the lymph nodes in the abdomen is quite confusing, since they are a large conglomerate of organs of the lymphatic system located in the peritoneum, in the lower abdomen, near all abdominal organs and along the aorta.
The main groups of abdominal lymph nodes:
- mesenteric lymph nodes;
- para-aortic lymph nodes;
- paracaval lymph nodes;
- parapancreatic nodes.
All these lymph nodes are combined into one large group - the retroperitoneal lymph nodes. The mesenteric lymph nodes provide lymph drainage from the posterior wall of the abdomen and intestines. Enlargement of mesenteric lymph nodes in adults and children is an alarming symptom that can appear against the background of various pathologies.
The para-aortic lymph nodes of the intra-abdominal region are located along the aorta.
Paracaval lymph nodes are located near the inferior vena cava.
All lymph nodes located near the pancreas, liver and gallbladder are called parapancreatic.
The functions of this group of lymph nodes are filtration of intercellular fluid (lymph), removal of toxins and infectious agents. Lymph nodes act as a filter, ensuring the normal functioning of the abdominal organs and the entire body as a whole. They are an important component of the human immune system, and therefore react acutely to episodes of decreased immunity.
Normal sizes
Lymph nodes in the abdomen of women, men and children are located the same, but their exact number is unknown. In general, the number of lymph nodes is an individual physiological feature; exact norms have not been established. For example, the number of celiac lymph nodes ranges from 9 to 15.
The size of the lymph nodes is another physiological feature. So, on average, mesenteric lymph nodes do not exceed 10 mm in diameter.
It is believed that the normal diameter of the lymph node is from 3 to 15 mm. At the same time, in humans, some nodes can reach 50 mm in diameter, which will not be considered a deviation from the norm. As a rule, internal lymph nodes are much smaller than superficial ones.
Each abdominal lymph node has an individual size, but the norm will depend on where it is located. Thus, the splenic nodes are quite small and are rarely more than 5 mm in diameter. Para-aortic lymph nodes can reach 10 mm, but mesenteric lymph nodes are most often also small in size - about 3-7 mm.
The normal sizes of lymph nodes in children are the same as in adults. It is worth noting that in children under 3-5 years of age, the lymph nodes are always slightly enlarged, which is due to the peculiarities of the child’s immune system.
2. Reasons
The etiopathogenesis of lymphomas, including intestinal lymphoma, has currently been studied and insufficiently clarified.
It is believed that the predisposing factor is a general weakness of the immune system, i.e. patients, for example, with HIV/AIDS are clearly at risk. There is also evidence that the likelihood of “triggering” lymphoma increases significantly with long-term use of hormone-containing drugs, as well as in the presence of intestinal parasitosis (hence a certain endemicity of the disease: in the poorest African countries its prevalence is higher). In addition, certain age and gender trends have been established: the peak incidence occurs in the category of people over 50 years of age, the majority of whom are men.
Visit our Gastroenterology page
Stages of lymph node cancer
The stage of lymph node cancer is determined based on the clinical picture and the extent of the tumor lesion. The Ann Arbor classification is used for this:
Stage 1 - the lymph nodes of only one lymphatic zone are affected.
Stage 2 - lymph nodes of 2 or more zones on one side of the diaphragm are affected.
Stage 3 - lymph nodes on both sides of the diaphragm are affected.
Stage 4 - cancer extends beyond the lymphatic system and affects other organs and tissues, for example, the liver, bone marrow.
This classification is supplemented by the Cotswold modification:
- A - B-symptoms are absent.
- B - there is at least 1 B-symptom.
- E—foci of extranodal lesions are detected.
- S - there is damage to the spleen.
- X - massive cancerous damage to tissues and internal organs.
3. Symptoms and diagnosis
The clinical picture is formed by numerous and, as a rule, significantly pronounced symptoms, none of which, however, is pathognomonic (unambiguously indicating this disease). The diagnosis of “intestinal lymphoma” is assumed based on a specific combination of such manifestations as significant enlargement and palpable tenderness of the lymph nodes, pain (usually aggravated by defecation and/or eating), fever and general malaise, various dyspeptic symptoms, and hyperhidrosis. Sometimes there is an admixture of blood in the stool. One of the features of intestinal lymphoma that distinguishes it from other oncological diseases is the rapid appearance and increase in clinically significant symptoms, which leaves a chance for early correct diagnosis.
It should be noted that intestinal lymphomas vary widely in terms of aggressiveness, growth rate, specific localization (usually the small intestine, less often the large intestine, very rarely total damage to the entire intestine occurs), histological characteristics, as well as staging in each specific case of seeking help.
The decisive diagnostic method is biopsy. Some clinical variants of intestinal lymphoma, especially in advanced forms, are characterized by an extremely unfavorable prognosis, while others (up to 50%) are considered curable.
About our clinic Chistye Prudy metro station Medintercom page!
Symptoms of lymph node cancer
Symptoms of cancer of the lymphatic system are very diverse, but they can all be combined into three large groups:
- Enlarged lymph nodes, or lymphadenopathy. Lymph nodes enlarge gradually and painlessly. If they are located close to the surface of the skin, such as in the neck, armpit or groin, they are easily visualized or palpated. Often patients themselves turn to the doctor when they discover such a problem. If the disease begins with damage to the internal lymph nodes, there may be symptoms associated with compression of the internal organs, such as pain, coughing, etc. However, these signs appear when the cancer grows large enough to cause compression of the organs.
- B-symptoms. This is a triad of symptoms - persistent fever not associated with infection, night sweats and weight loss. The presence of B-symptoms in cancer of the lymphatic system is of great importance for determining the stage of the disease and influences the choice of treatment method.
- Symptoms that develop when cancer spreads from the lymph nodes to internal organs. Here the symptoms can be very diverse. The membranes of the brain, bones, and spleen are often affected. Accordingly, neurological manifestations occur (head pain, vomiting, blurred vision), bone pain, decreased cerebral hematopoiesis, etc.
4.Treatment
Once the diagnosis is established and confirmed, a standard oncological treatment regimen is prescribed, usually with surgical removal of foci of malignant lymphocyte accumulation and mandatory subsequent chemotherapy. Currently, the possibilities of innovative treatment methods (immunotherapy, HIFU therapy, etc.) are being intensively and effectively studied, which gives grounds for reasonable optimism in terms of prospects.
It must be emphasized that the prognosis for intestinal lymphoma (as with any other oncological diseases) critically depends on the timely detection and identification of pathology, especially since in this case early reliable diagnosis is quite possible. Therefore, if you have any combination of the symptoms described above, you should consult a doctor immediately.
Enlarged lymph node syndrome as a pediatric problem
The cause of enlarged lymph nodes in most cases is processes not related to hematological malignancies: most often these are general pediatric, infectious, immune and other conditions
The fact that a pediatrician quite often discovers enlarged lymph nodes (LNs) in his patients and he has to quickly find an answer to the questions “why?” and “what to do?”, allows you to do without a long introduction. Thus, when conducting pediatric screening and subsequent analysis of 1607 diagnoses of acute and chronic diseases in children and adolescents aged 5–17 years, it was revealed that lymph node diseases were detected in 3.35% of cases [6]. Traditionally, when enlarged lymph nodes are detected, without taking into account other components of this syndrome (history, general clinical picture, local symptoms), the pediatrician thinks about an oncohematological disease. As a result, such patients make up 40% of all patients of oncohematologists [7], which seems unjustified. The frequency of newly diagnosed cases of oncohematological diseases in our country is low. The incidence of acute leukemia is 4.0 - 5.0 cases per 100,000 children per year, non-Hodgkin's lymphoma - 0.9 - 1.1 per 100,000 children per year. This makes it clear why the overwhelming majority of children with enlarged lymph nodes return from hematologist appointments to pediatricians with a diagnosis of lymphadenitis. That is, the reason for the increase in lymph nodes in most cases is processes not related to hematological malignancies: general pediatric, infectious, immune and other conditions. Based on the above, we decided to present our point of view on swollen lymph node syndrome.
| Figure 1. Submandibular lymph nodes in lymphogranulomatosis (ultrasound, 7.5 MHz) |
| Figure 2. Submandibular node in tuberculosis (ultrasound, 7.5 MHz) |
LN enlargement can result from lymphadenitis (LA) and lymphadenopathy (LAP).
LA is an inflammation of the lymph nodes that occurs as a complication after various purulent-inflammatory diseases and specific infections (tuberculosis, actinomycosis, plague, etc.). LA is usually a secondary process.
LAP is a systemic enlargement of lymph nodes, not associated with inflammation (effects of certain medications, proliferation, metastasis, etc.).
The epidemiology of PA and PAP has not been developed. One can only note that, according to I. S. Tarasova [6], in continuous mass studies of children in the Bryansk region, LA occurs, as one would expect, somewhat more often (1.86% among all examined) than PAP (1.49 % of the total contingent).
Methods for studying lymph nodes should be standardized as much as possible. In clinical practice, complaints are assessed (local pain, local or general increase in temperature, general somatic complaints), anamnesis (epidemiological history, duration of onset, localization of enlarged lymph nodes in one or several groups, their simultaneous increase or gradual increase, speed of disease manifestation, etc.) . Examination of the patient is of particular importance. Along with a thorough general pediatric examination by system, it is necessary to pay attention to the number of altered lymph nodes and their location by group. The size of the lymph nodes should be assessed only objectively: in millimeters or centimeters. Comparison of the size of LU with grain, peas, cherries, hazelnuts or walnuts, which is accepted in our country and widely recommended in the domestic literature, is irrational, gives incomparable results and should be eliminated. It is necessary to carefully record the ratio of enlarged lymph nodes to each other. For example, the location of lymph nodes according to the “solar system” type (one large lymph node in the center and on the periphery of it lymph nodes of smaller diameter) is typical for tuberculous lymphadenitis [2]. LNs can be elastic, dense, with fluctuation phenomena. The adhesion of the lymph nodes to neighboring nodes and surrounding tissues, the presence or absence of pain on palpation, must be described. It is necessary to examine and describe the condition of all accessible lymph nodes: occipital, submandibular, anterior and posterior cervical, supra- and subclavian, axillary, elbow, inguinal, popliteal. Inspection and palpation data are supplemented, confirmed and clarified by instrumental techniques. First of all, these are non-invasive imaging methods used to study deep-lying lymph nodes. They allow you to accurately determine the size of lymph nodes, changes in groups of lymph nodes that are inaccessible to inspection and palpation, characteristics of the capsule, adhesion, topographical features, internal structure; exclude conditions simulating lymph node enlargement (tumors not originating from lymph nodes, hematomas, kidney anomalies, etc.). It is extremely important to obtain information about the condition of the liver and spleen. In terms of accessibility and speed of obtaining information, echography (ultrasound) ranks first. LNs with a diameter of less than 1.5 cm are close in density to the surrounding adipose tissue, are rarely visualized, and it is almost impossible to limit their tumor damage from other causes of enlargement only according to ultrasound data. Such lymph nodes are observed primarily in infectious processes, reactive lesions, and in children with hemoblastoses - in a state of complete remission. LNs with a diameter of 1.5 - 2 cm are well visualized if they are projected onto echo-negative structures or change the usual topographic-anatomical relationships. The entire spectrum of ultrasound changes can be reduced to several main groups [3].
1. The enlargement of individual lymph nodes is assessed as small if they do not lose their usual ultrasound picture, retain the capsule, clarity and evenness of the contour, and do not change the topic of the organ. This type is typical for infectious lesions, especially tuberculosis, viral hepatitis, collagenosis, immunodeficiency, hemoblastosis in children at low risk.
2. Further growth of lymph nodes leads to the appearance of masses merging with each other, pushing aside the vessels. It is observed with purulent melting of a group of lymph nodes, with hemoblastosis, metastatic tumors.
3. Compression or pushing aside of internal organs. In this case, hydronephrosis may occur due to compression of the ureters, significant displacement of the uterus and bladder. Typically for extremely unfavorable variants of myeloid leukemia, Hodgkin's lymphoma and non-Hodgkin's lymphoma.
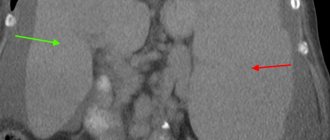
Ultrasound findings can be confirmed by computed tomography (CT). Additionally, CT allows one to clarify the structure of lymph nodes, their topographic relationships, and detect other groups of lymph nodes.
If it makes sense to evaluate superficial lymph nodes only echographically, and mesenteric and retroperitoneal lymph nodes are almost equally well detected by ultrasound and CT, then intrathoracic lymph nodes are detected almost exclusively radiographically.
| Comparison of the size of lymph nodes with grain, peas, cherries, hazelnuts and walnuts, which is accepted in our country and widely recommended in the domestic literature, is irrational, gives incomparable results and should be eliminated |
Diagnostic methods such as isotope scintigraphy and lymphography can be used according to very strict indications in specialized clinics or limitedly in dynamic studies and are not used in widespread practice.
Reliable identification of the causes of lymph node enlargement is possible only by histological methods. In this case, the material should be obtained only by open biopsy of lymph nodes, although modern techniques of fine-needle biopsy make it possible to obtain reliable results. The previously recommended puncture biopsy gives a very high percentage of false-positive and false-negative results.
LN enlargement can be schematically [5, 11] presented (with a description of some practically significant but little-known forms) as associated with infection (IA) and not associated with infection (PAP).
1. LA of viral nature.
- cytomegaly.
- Infectious mononucleosis.
- measles.
- rubella.
- psittacosis.
- Ardmore's syndrome.
An infectious disease, most likely of a viral nature, the peak incidence is observed in the fall, and is transmitted by airborne droplets.
The contagiousness index is high, the incubation period is 3-10 days. It begins with pharyngitis, rhinitis, low-grade fever. It occurs with a generalized enlargement of lymph nodes, a painful enlarged liver (less commonly, splenomegaly), myalgia, and chest pain. Recovery without consequences. 2. LA for bacterial infections.
- caries.
- abscess.
- cat scratch disease. Called Bortanella (Rochalimeae) hensella. More often, bilateral inflammation of lymph nodes (including mesenteric and intrathoracic) with general and skin nonspecific symptoms, which occurs benignly with spontaneous recovery, is caused by skin wounds from cats, dogs, and, less often, from foreign sharp objects. Granulomatous hepatitis, splenomegaly, encephalitic reactions, and convulsive syndrome have been described [8, 10]. It is observed mainly in children and adolescents, mainly in late autumn and winter.
- Borreliosis. Known as pseudolymphoma. Lymphoproliferative lesions of lymph nodes and skin during infection with Borrelia burgdorferi after a tick bite. Transitions to malignant lymphomas have been described.
- Tuberculosis. Along with the typical forms of tuberculosis, one should remember about the so-called. atypical mycobacteriosis. According to F. Miller [2], up to 50% of submandibular lymph nodes in children under 5 years of age are caused by atypical strains of mycobacteria (in particular, the avium type), and the probability of mycobacterial lesion of lymph nodes is higher, the younger the child (Fig. 1).
- Sepsis.
- Allergic subsepsis. It is also considered as a variant of juvenile rheumatoid arthritis, the so-called. Still's disease.
- Syphilis. The rate of increase in the incidence of syphilis in children is significantly higher than that in adults. Thus, the incidence of syphilis among adults increased 15.8 times over 4 years, and among children - 21 times. 65.6% of children became infected through sexual contact [1].
- Genito-anorectal symptom complex is a complication of chronic PA in chlamydia serotypes L1-L3 with periproctitis, chronically recurrent perianal and perineal fistulas, strictures and fibrosis of the genitourethral tract, and elephathiasis of the vulva. It occurs mainly in female patients.
3. LA for fungal diseases.
- histoplasmosis.
4. LA for parasitic diseases.
- echinococcosis.
5. LA for protozoal infections.
- toxoplasmosis. The subclinical variant is cervical subacute necrotizing PA. Clinically - painful, often cervical PA, with spontaneous remission after 3 - 6 months, fever, exanthema. Neutropenia. Histologically - coagulative necrosis with histiocytic and immunoblastic cells without granulomas, without neutrophils. Differential diagnosis is carried out with malignant lymphomas, tuberculosis, histiocytosis, and according to histology (vasculitis) - with systemic lupus erythematosus.
- kala-azar.
- malaria.
Forms not associated with infections (PAP)
1. Medicinal PAWS.
- Hydantoin derivatives (diphenin, etc.) are anticonvulsants. With this complication of therapy, PAP is considered autoimmunoblastic.
- allopurinol (used in the treatment of hyperuricemia, including myeloproliferative conditions).
- anti-leprosy drugs (used in gastroenterology for the treatment of chronic colitis, in rheumatology - for the treatment of arthritis and spondyloarthritis, especially those associated with the histocompatibility antigen HLA B-27).
- post-vaccination.
- against the background of foreign bodies.
2. With systemic processes in the body.
- collagenosis (in this case, the greatest increase in lymph nodes is still recorded in infected variants of diffuse connective tissue diseases, that is, there is a combination of LA and PAW).
- local tumor-like amyloidosis. Traditionally described as a pathology exclusively of adults [4]. However, we found this form of dysproteinosis in 2 of 44 children with systemic amyloidosis. Local tumor-like amyloidosis in our patients occurred with a pronounced general paraspecific reaction, which, in combination with a palpable mass in the abdominal cavity, initially led to an erroneous diagnosis of lymphoma.
- Lubarch amyloidosis, genetically determined. Generalized PAP, orthostatic hypotension, obstructive infiltrative cardiomyopathy, splenomegaly, neuropathy, carpal tunnel syndrome.
- Dorfman-Rosai syndrome (intermittent benign lymphadenopathy). Probably an autoimmune disease with benign proliferation of plasma cells, histiocytes, and fibroblasts. The peak incidence is in the first 10 years of life. It occurs with bilateral cervical, often generalized lymph node enlargement, fever, leukocytosis, erythema nodosum. According to our observations, if internal organs are damaged, the prognosis is poor. The prognosis worsens in the presence of simultaneous immunodysfunction (accelerated ESR, dysproteinemia).
- Leiner's desquamative erythroderma. Most likely, a defect in leukocyte chemotaxis and deficiency of the complement fragment C5. The disease manifests itself in the first 3 to 4 months of life. It manifests itself as a generalized enlargement of all lymph nodes, secondary erythroderma, nail dystrophy, anemia, vomiting, and diarrhea. More common during breastfeeding. Familial cases are known. The prognosis is favorable.
3. Granulomatosis
- sarcoidosis
- allergic granulomatosis Churg-Strauss. Combined with a history of atopy. Manifests itself in the form of bronchial asthma, severe eosinophilia, PAP, neuropathy, skin ulcers, damage to the heart, lungs, intestines and vasculitis of small arteries and veins.
- multicentric reticulohistiocytosis. Systemic granulomatous disease with the formation of skin nodules, destructive arthritis, and damage to internal organs. It proceeds according to the type of psoriatic arthropathy.
- Lipomelanotic reticulosis (Pautrier-Waringer syndrome) is a localized or generalized increase in lymph nodes as an accompaniment of dermatoses, primarily melanoerythroderma.
| Figure 3. Atypical histiocytes in the lymph node punctate with histiocytosis X. Romanovsky staining. X900 |
4. PAW for hemoblastoses.
- acute leukemia.
- non-Hodgkin's lymphomas.
- Hodgkin's lymphoma (according to the old terminology - lymphogranulomatosis).
- alpha heavy chain disease (Mediterranean lymphoma). Observed mainly in childhood and adolescence, the clinic is caused by severe malabsorption syndrome, which is the result of lymphoproliferative processes with infiltration of the small intestine and mesenteric paws.
- gamma heavy chain disease. It is caused by monoclonal gammopathy and occurs as a lymphoproliferative systemic disease.
- histiocytic syndromes
5. LAP in metastasis of solid tumors to lymph nodes.
6. Paraneoplastic reactions [12].
- POEMK complex. Paraneoplastic symptom complex (especially often with sclerosing plasmacytomas) = polyneuropathy + organomegaly + endocrinopathy + dysglobulinemia (M-gradient) + skin lesions.
7. PAP in primary immunodeficiency conditions (PID).
- common variable immune deficiency.
- autoimmune lymphoproliferative syndrome.
- granulomatosis septic. A heterogeneous group of immune defects, united by incomplete intracellular phagocytosis of catalase-positive microbes as a result of deficiency of hydrogen peroxide and atomic oxygen [11]. Currently, 4 different molecular defects are known: a) X-chromosome-linked recessive defect of cytochrome B558 heavy chains; b) autosomal recessively inherited defect of light chains of cytochrome B558; c) defect of 47 kd cytosol factor; d) defect of 65 kd cytosol factor. Clinical signs: acute abscess infections of the skin, lungs, gastrointestinal tract, lymph nodes, liver, spleen caused by catalase-positive bacteria (staphylococci, enterobacteria), as well as aspergillus; chronic granulomatous inflammation in the gastrointestinal tract and urinary tract with possible stenosis; decreased production of atomic oxygen and hydrogen peroxide in response to soluble and opsonized stimuli.
| Data from examination and palpation of lymph nodes must be confirmed and clarified by instrumental methods. First of all, non-invasive imaging methods used to study deep lymph nodes |
8. Genetically determined PAWS [9].
- Klippel-Trenaunay syndrome. Combination of local lymphangiomas and hemangiomas.
- syndromes with hereditary lymphedema. Wever-Smith and Milroy syndromes.
- pulmonary muscular hypertrophy - muscular cirrhosis of the lung. The proliferation of smooth muscle fibers is perialveolar, peribronchial, interstitial, interlobar. Enlarged lymph nodes at the hilum of the lungs. DD is carried out with sarcoidosis, tuberculosis, pulmonary emphysema, alveolar-capillary block syndromes. The diagnosis is verified only histologically.
9. Acquired immunodeficiency syndrome (AIDS).
In the process of diagnosing diseases that occur with an increase in lymph nodes, the efforts of pediatricians, infectious disease specialists, immunologists, and oncohematologists are combined. The main role in this case is given to the pediatrician, since most PAs and PAPs in children are associated with an infectious process. At the same time, one cannot insist on the infectious genesis of lymph node enlargement if a two-week course of antibiotic therapy did not lead to a significant improvement in the clinical, laboratory and instrumental picture. In favor of the oncohematological genesis of changes in lymph nodes is indicated by an increase in their diameter to 4 cm or more, stony density, tuberosity, formation of conglomerates of lymph nodes, their adhesion to surrounding tissues, intrathoracic conglomerates, especially in the upper mediastinum, intraperitoneal conglomerates.
A clear knowledge of the variety of causes of lymph node enlargement will help pediatricians in the diagnosis and differential diagnosis of this syndrome.
Literature
1. State report on the state of health of the population of the Russian Federation in 1994. M., 1995. p. 43. 2. Miller J. Tuberculosis in children and adolescents. M.: Medicine, 1984. p. 296. 3. Nazarenko O. R. Comparative value of echography in assessing the condition of the abdominal organs in children with acute lymphoblastic leukemia. Author's abstract. dis. ... Ph.D., M., 1997. p. 24. 4. Nikhamkin L. I. Local tumor-like amyloidosis of the mesentery. Archives of Pathology, 1966. 4. p. 76 - 78. 5. Samochatova E.V., Vladimirskaya E.B., Zhestkova N.M., Navolotsky A.V. et al. Hodgkin’s disease in children. M.: Altus. - 1997. 96. 6. Tarasova I. S. Clinical and hematological characteristics of children under various radiation dose loads. Author's abstract. dis. ... Ph.D. M., 1997. p. 25. 7. Chernov V.M., Finogenova N.A., Shakhtalin V.V., Sidorovich G.I. Structure of hematological morbidity of children in the city of Klintsy, Bryansk region. In the book: Medical aspects of the influence of low doses of radiation on the body of children and adolescents. Obninsk - Moscow, 1992. p. 92 - 95. 8. Dangman BC, Albanese BA, Kocia M. Cat scratch disease with fever of unknoun origin: imaging features and association with new causative agent Rochalimea henselae. Pediatrics, 1995. v. 5. p. 767 - 771. 9. Emery A., Rimoin D. Principles and practice of medical genetics. 1988. V. 1, 2. 10. Flexman J. Bortanella henselae is a causative agent of cat scratch disease in Australia. J. Infect., 1995. V. 31. No. 3. p. 241 - 245. 11. Leiber B. Die klinischen Syndrome. Muenchen, 1990, Bdd. 1.2. 12. Siegenthaler W. Differential diagnosis innerer Krankheiten. Stuttgard, 1993. s. 800.
Prevention
As part of prevention, it is recommended to avoid exposure to risk factors that cause lymph node cancer, if possible. Individuals at risk are advised to undergo regular medical examinations.
| More information about treatment at Euroonco: | |
| Oncologist-hematologist | RUB 11,500 |
| Chemotherapy appointment | RUB 6,900 |
| Emergency oncology care | from 12,100 rub. |
| Palliative care in Moscow | from 44,300 rubles per day |
| Radiologist consultation | RUB 11,500 |
Book a consultation 24 hours a day
+7+7+78
Treatment of cancer of the lymphatic system
Treatment of lymph node cancer will depend on the histological type of the tumor, the stage of the disease, the age of the patient and his general condition. For each type of lymphoma, its own treatment protocols have been developed, taking into account the listed factors. In general, the following methods are used:
- Chemotherapy.
- Radiation therapy.
- Surgical intervention.
- Targeted therapy.
- Other treatments.
Chemotherapy
Chemotherapy is the mainstay of treatment for the vast majority of lymphatic cancers. Treatment consists of several blocks, for example, remission induction, remission consolidation and maintenance therapy. In some cases, when the tumor is very aggressive or there are relapses, high-dose chemotherapy is used followed by stem cell transplantation.
Chemotherapy drugs can be administered systemically (orally or intravenously) or locally, particularly into the spinal canal. This is necessary in cases where there is a high risk of damage to the membranes of the brain and spinal cord.
Radiation therapy
As an independent method of treating cancer of the lymphatic system, radiation therapy is rarely used, for example, for localized lesions of relatively benign lymphomas.
Radiation therapy is also used as palliative treatment to reduce symptoms of the disease. For example, to relieve bone pain, reduce the volume of tumor mass due to compression of internal organs, etc.
Surgery
Surgical interventions for lymph node cancer are performed for palliative purposes, to eliminate life-threatening conditions. For example, with perforation of the gastrointestinal tract, with the development of obstructive jaundice, etc. As the main method of treatment, surgery is used for isolated damage to internal organs, for example, the gastrointestinal tract, but in this case chemotherapy is still necessary.
Other treatments
Treatment regimens for many types of lymphomas include the use of targeted drugs, immunotherapy, monoclonal antibodies, etc. Such methods make it possible to achieve remission in a larger number of patients, improve treatment results in the event of relapses, and increase overall life expectancy.
Diagnosis of lymph node cancer
Diagnosis of cancer of the lymphatic system requires a comprehensive approach, which is aimed at confirming the diagnosis and determining its stage.
The diagnosis is made only after a pathomorphological examination of a fragment of the affected lymph node. For this purpose it is necessary to perform a biopsy. The resulting material is poured with paraffin and preparations are made from it, cutting the tumor into a thin layer so that it can be examined under a microscope. Additional laboratory diagnostic methods are also used, for example, immunohistochemical staining, molecular genetic tests, etc.
To determine the stage of the disease, radiation diagnostic methods are used:
- PET-CT.
- CT.
- MRI.
- Ultrasound.
- Scintigraphy.
With their help, affected lymph nodes and extralymphatic foci are visualized.
Forecast
The prognosis of lymph node cancer depends on many factors. The key points here are:
- Type of lymphoma.
- Prevalence of the process.
- Patient's age.
- General condition of the patient at the time of diagnosis.
- Possibility of radical treatment.
In general, when treating stage 1-2 lymphomas, it is possible to achieve a complete 5-year remission in more than 80% of cases. Unfavorable prognostic signs are: age over 60 years, involvement of the bone marrow in the process and the presence of extralymphatic lesions.