Main function of the gallbladder
The gallbladder is located under the liver
The gallbladder is an organ located on the lower surface of the liver and adjacent to it. It performs a storage function, which, as the name implies, means the accumulation of bile coming from the liver.
This organ is located in the right longitudinal hepatic groove and has a relatively small size - its length varies from 8 to 14 cm, and its width is no more than 5 cm. In addition to this main function, the gallbladder has a number of other, no less important:
- Concentration - bile coming from the liver to the gallbladder is concentrated and changes its density
- Absorption - bile components can be absorbed through the wall of the organ, which helps cleanse the body
- Evacuation - as a result of contraction of the gallbladder during the digestion process, bile is released into the duodenum
- Valve - depending on the processes occurring in the body, it ensures the passage or obstruction of bile into the intestines.
These functions are important, however, in addition to them, there are a number of others - with the direct participation of this organ, the lipase enzyme is activated, on which the digestion of fats depends, and the growth of pathogenic intestinal microflora slows down.
How to prevent relapses?
Removing the gallbladder does not guarantee the recurrence of gallstones. That is why, in addition to frequent and balanced meals in small portions, you need to add natural choleretic agents to your new habits. In 10% of operated patients, cholecystitis appears after removal of the gallbladder. If everything happens again, the doctor will prescribe artificial choleretic drugs, but it’s better not to let things get to that point. Be sure to drink immortelle, milk thistle, tansy, and barberry. When choosing such fees, be sure to consult your doctor.
Milk thistle oil is considered the mildest natural remedy for the proper flow of bile. It contains the active ingredient silymarin, a natural hepatoprotector. In addition to the choleretic effect, this oil removes formed toxins from the liver along with bile.
As you can see, consequences after removal of the gallbladder do occur. But the changes are not significant - it is enough to eat healthy foods and healthy vegetable oils.
Violations in the work of the body
Due to its very modest size, this small organ and the importance it has in the human body are often underestimated. However, if its functioning is disrupted, a person has serious problems. The reasons for the malfunction of this organ can be considered:
- Psycho-emotional factor - any stress, emotional overload, nervous shock and other problems associated with the mental sphere of life negatively affect the functioning of the biliary system.
- Hormonal imbalance or hormonal disorders. In the female body, this cause is most often provoked by the onset of the menstrual cycle or menopause. The hormonal balance is also greatly influenced by the state of pregnancy and subsequent childbirth.
- Pathologies of the liver and kidneys, formation of stones (calculi).
- Diabetes.
- Inflammation caused by an advanced infection or severe cold.
The main problem of disruption of the proper functioning of the gallbladder is the accumulation and poor passage of bile, which, in turn, is accompanied by very painful symptoms:
- Colic and prolonged spasms
- Dull pain in the hypochondrium
- Prolonged nausea and vomiting
- Bad taste in mouth
- Fever, shaking and chills
- Constant fatigue.
On average, the body of a healthy adult accumulates about 50 ml of bile in the gallbladder. Up to 30 ml of fluid can accumulate in a child's gallbladder. However, with serious diseases, the volume of accumulated bile increases, which may indicate problems associated not only with this organ, but also with the liver.
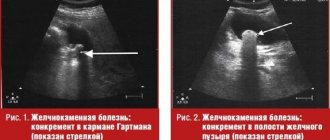
Diagnosis of diseases in the most effective way is done using ultrasound of the abdominal cavity and gallbladder, including. Radioisotope aspects of diagnostics are used as additional research methods.
Newspaper "News of Medicine and Pharmacy" Gastroenterology (304) 2009 (thematic issue)
Anomalies of the biliary tract are congenital defects and malformations, accompanied by a violation of the drainage function of the biliary system, the development of pathological processes and, as the latter progress, manifesting certain symptoms (Fig. 1). Until now, there is no generally accepted classification and nomenclature of variants and anomalies in the development of the organs of the biliary system. Thus, some authors believe that all changes in the biliary system (from minor deviations to deformities incompatible with life) are anomalies. According to others, only defects and malformations that are accompanied by a violation of the drainage function of the biliary system should be classified as anomalies. It is noted that the biliary system has wide limits of individual variability. There are different points of view on the issue of inheritance of gallbladder anomalies. These deviations can be inherited either dominantly or recessively. One of the factors in the development of tissue dysplasia (in particular cysts) is chlamydial infection. However, it should be noted that anomalies and malformations of the biliary tract in most cases are accompanied by impaired motility of the gallbladder. In this regard, anomalies can be considered a risk factor for the development of functional and organic pathology.
Anomalies of the bile ducts
Biliary atresia
There are three main anatomical variants of atresia:
a) the distal part of the external bile ducts, gallbladder; b) external bile ducts; c) intrahepatic bile ducts.
The main clinical sign is progressively increasing jaundice. It appears from the first days of life, sometimes at 2–4 weeks after birth. The skin, sclera and mucous membranes become grayish-green, and at the peak of jaundice they acquire a saffron hue. The stool becomes acholic on the 2nd–3rd day. In the future, acholia may be intermittent, which is associated with the diffusion of bilirubin from the blood vessels into the intestines. Sometimes stool may have a light lemon color as a result of the release of a small amount of bile pigments by the intestinal glands or the activity of intestinal microflora. There is a gradual increase in the size of the liver, its consistency becomes dense, and the edge becomes pointed. Enlargement of the spleen is observed in parallel or slightly later. Signs of portal hypertension appear: dilation of the veins on the anterior abdominal wall, ascites, bleeding from varicose veins of the esophagus and stomach. With the development of intestinal paresis, the size of the abdomen increases, flatulence, vomiting, diarrhea, malnutrition, and anxiety develop. By the 4–5th month of life, signs of liver failure appear, which leads to the death of the child at 8–10 months of life.
The level of hemoglobin, red blood cells, leukocytes, platelets, prothrombin and fibrinogen in the blood decreases. The content of direct and, over time, indirect bilirubin and alkaline phosphatase increases. For a long time, transaminase activity remains normal. A urine test reveals bile pigments in the absence of urobilin. As the disease progresses, all types of metabolism are disrupted.
During diagnosis, imaging is not enough to exclude the diagnosis of bile duct atresia. Confirmation of atresia is the absence of discharge of contrasting bile into the intestine, so radiography should be performed 3, 6 and even 24 hours after administration of the contrast agent. The most appropriate diagnostic methods are direct cholangiography, laparoscopy and liver biopsy.
Differential diagnosis should be carried out with physiological jaundice, hemolytic disease of the newborn, bile thickening syndrome. Physiological jaundice usually disappears within 2–3 weeks of life, the color of stool and urine does not change. Hemolytic disease of newborns is characterized by anemia, increased levels of indirect bilirubin, and intense staining of stool and urine. There is information about the incompatibility of the blood of mother and fetus according to the Rh factor or the ABO system. Bile thickening syndrome most often disappears spontaneously or after the administration of cholekinetics.
For atresia of the extrahepatic bile ducts, surgical treatment is effective, which is best carried out before 11 months. With atresia of the intrahepatic ducts the prognosis is unfavorable.
Hypoplasia of interlobular intrahepatic bile ducts
There are two forms of the disease - syndromic and isolated (non-syndromic). These forms can be distinguished based on the results of a morphological study of a significant number of portal tracts.
Syndromic tubular hypoplasia is characterized by anatomical changes only in the intrahepatic bile ducts in the absence of extrahepatic pathology. This form is usually combined with various developmental anomalies (cardiovascular system, face, spinal column). In children in the first 3 months of life, signs of cholestasis appear (jaundice, discoloration of stool, itching). Jaundice has a recurrent course, and the severity of skin itching remains stable. The degree of stool discoloration varies periodically. The liver enlarges. On palpation it is painful, soft-elastic or dense consistency, the surface is smooth, the edge is rounded. The spleen is often enlarged. Xanthomas may appear on the hands, in the area of the elbow and knee joints, the back of the neck, popliteal fossae, in the groin area, around the anus, which indicates the severity of the process and the duration of cholestasis. Characteristic is periodic moderate hyperbilirubinemia, combined with high levels of total lipids and cholesterol. There is a significant increase in alkaline phosphatase and a moderate increase in transaminases. Hypoplasia of the interlobular intrahepatic bile ducts is combined with other developmental anomalies. These may be facial changes: a convex forehead, deep-set eyeballs, moderate hypertelorism, sometimes retraction of the root of the nose, the chin is reduced in size, sharp, raised and directed upward. A systolic murmur is often heard at the apex, and right ventricular hypertrophy is detected. An angiographic study reveals hypoplasia or stenosis of the pulmonary artery, less often - coarctation of the aorta, vertebral anomalies (lack of fusion of the anterior arches of one or more vertebrae without the development of scoliosis, fusion of the lateral parts of the vertebral bodies). There may be a delay in physical, mental and sexual development.
Isolated tubular hypoplasia is characterized by intrahepatic cholestasis, which develops against the background of the normal anatomical structure of the intrahepatic bile ducts. Clinical manifestations are similar to those of extrahepatic bile duct atresia. However, they are less pronounced and appear in the first months of life. Sometimes this anomaly can be asymptomatic. At the age of 5 months, itchy skin often appears. Subsequently, hepatomegaly develops, then splenomegaly, osteoporosis, and xanthomas. In a biochemical blood test, an increase in the levels of bilirubin, cholesterol, lipids, alkaline phosphatase and transaminases activity, a decrease in prothrombin levels and a disturbance in calcium metabolism are observed. Steatorrhea develops. The course of isolated tubular hypoplasia is severe, often accompanied by the formation of liver cirrhosis with the development of hemorrhagic syndrome and portal hypertension.
Differential diagnosis must be carried out with diseases occurring with cholestasis syndrome. Severe familial intrahepatic cholestasis (Byler's disease) is characterized by a moderate increase in the level of conjugated bilirubin with normal levels of cholesterol and total lipids. The administration of cholestyramine and phenobarbital for Byler's disease leads to a temporary reduction in skin itching. Familial benign cholestasis (Summerskill disease) is characterized by a relapsing course. There is an alternation of periods of pronounced clinical manifestations (from 2 months to 2 years) and remission (from 1–6 months to 8 years). The period of exacerbation is characterized by the presence of jaundice and skin itching; urine becomes dark in color, feces are discolored. High hyperbilirubinemia, increased levels of bile acids, alkaline phosphatase activity, and a significant increase in lipids and cholesterol are detected in the blood. In Aagenes syndrome, intrahepatic cholestasis persists for 1–6 years. Hyperbilirubinemia, increased activity of alkaline phosphatase, transaminases, β-lipoproteins, α2-globulins and hypoproteinemia are pronounced. Patients often develop hemorrhagic phenomena, anemia, rickets, and growth retardation is observed, which disappears after the end of the period of cholestasis.
To treat this disease, patients are prescribed a diet enriched with protein, low in fat in the form of triglycerides, and fat-soluble vitamins A, D, E, K - parenterally. The use of cholestyramine and phenobarbital is effective. For portal hypertension in combination with hemorrhagic syndrome, splenectomy with splenorenal or portocaval anastomosis is indicated.
Common bile duct cysts
Most often, the first signs of the disease develop at the age of 3–5 years. Patients experience paroxysmal abdominal pain, intermittent jaundice; as it increases, abdominal pain intensifies, increased body temperature, weakened stool coloration, and darkened urine. An earlier onset of the disease is possible in the presence of significant narrowing of the distal bile duct in combination with cholangitis. Older children complain of a feeling of discomfort, heaviness in the epigastric region, and nausea. Some patients may develop a picture of an “acute abdomen.” Upon palpation of the abdomen at the lower edge of the liver, a tumor-like formation of elastic consistency without clear contours is determined, the size of which increases during the period of exacerbation. An increase in body temperature indicates the addition of inflammation. Ruptures and perforation of cysts with the development of acute perforated peritonitis and malignant degeneration of the cyst wall are possible.
For diagnosis, cholangiography is of greatest importance, in which congenital dilatation of the common bile duct is determined. Intense jaundice prevents cholangiography. Duodenal intubation is characterized by the release of a large amount of dark bile (portion B) and a decrease in tumor formation after the introduction of cholekinetics (magnesium sulfate, olive oil) through the probe into the intestinal lumen. It is possible to use radioisotope methods. In this case, it is possible to detect the accumulation of the isotope in the dilated duct. Using sonography, it is possible to identify a cyst, determine its size and relationship with surrounding tissues. This study is especially informative in the absence of clinical manifestations of the anomaly and when the size of the cyst is small.
Differential diagnosis is carried out with viral or congenital hepatitis, echinococcosis, cysts of various locations (liver, mesentery, omentum), Wilms tumor, right-sided hydronephrosis, cholelithiasis, bile duct atresia, retroperitoneal tumors, diseases occurring with enlarged lymph nodes (lymphogranulomatosis, lymphosarcoma, etc. .).
Caroli disease
(multiple cystic dilatations of the intrahepatic bile ducts). There are isolated cystic dilatations of the intrahepatic bile ducts and their combination with fibrocholangiocystic disease of the liver. Isolated dilatation of the ducts is manifested by symptoms of chronic cholangitis; stones are found in dilated ducts in the absence of portal hypertension syndrome. During an exacerbation, patients are bothered by pain in the right hypochondrium, anorexia, increased body temperature, and itchy skin. There may be moderate jaundice, an enlarged painful liver, increased bilirubin levels, transaminase activity, and alkaline phosphatase.
The main diagnostic methods are sonography, computed tomography, cholangiography, and liver puncture biopsy (Fig. 2a, b).
For treatment, antibiotics and choleretic agents are indicated. In some cases (with a relatively localized process), segmental liver resection or lobectomy is performed.
Hepatic duct abnormalities
are characterized by the confluence of the right or both hepatic ducts into the cervical part of the gallbladder, and therefore bile from the liver, bypassing the common hepatic duct, enters directly into the gallbladder, cystic, and then the common bile duct.
Accessory bile ducts are quite common and can open into any part of the extrahepatic biliary system or connect extrahepatic bile ducts in the absence of connection with the liver.
Anomalies of the common bile duct
characterized by doubling or ectopia of its outlet. They are asymptomatic and are discovered during surgery due to gallbladder disease.
Elongated cystic duct
leads to the development of biliary dyskinesia, cholecystocholangitis, which can be complicated by peritonitis.
Change in the level of confluence of the cystic duct
predisposes to impaired bile outflow and the development of cholecystocholangitis.
Absence of cystic duct
characterized by the presence in the cervical region of the gallbladder of a wide lumen connecting the cavity of the gallbladder with the common bile duct.
Cystic duct hypoplasia and fibrosis
characterized by the presence of bends and narrowing of its lumen along its entire length. This contributes to the development of dyskinetic disorders of the biliary tract or chronic cholecystocholangitis.
Gallbladder abnormalities
There are several types of gallbladder anomalies:
a) shape anomalies (kinks, septa, gallbladder in the form of a bull’s horn, hook-shaped, S-shaped, rotor-shaped, in the form of a Phrygian cap); b) position anomalies (intrahepatic, interposition, inversion, dystopia, rotation); c) quantity anomalies (agenesis, duplication, diverticula); d) size anomalies (hypogenesis, giant gallbladder).
Agenesis
- isolated absence of the gallbladder. This condition is rare, mainly in girls, and is accompanied by compensatory dilation of the common bile duct. The disease is often asymptomatic. In older children, there is a tendency to develop dyskinetic disorders of the biliary tract, cholangitis and cholelithiasis due to the development of sclerotic processes in the sphincter of Oddi. The main diagnostic method is x-ray examination. In this case, on radiographs there is no shadow of the gallbladder (symptom of a “silent” bladder) and the expansion of the common bile duct is determined.
Accessory (double) gallbladder
characterized by the presence of two gallbladders with independent cystic ducts or a divided bladder consisting of two chambers with a common excretory duct. Clinical manifestations are often absent. Detection of an anomaly often occurs accidentally during an X-ray or sonographic examination. However, over time, complaints of a feeling of heaviness in the stomach after eating may appear. The cause of the pain syndrome is dyskinetic phenomena due to pressure differences in the gallbladders or chambers of the divided bladder. The development of inflammatory changes, cholelithiasis, and the formation of hydrocele of the gallbladder is possible. To make a diagnosis, sonography is used in combination with x-ray examination. Treatment is aimed at improving the flow of bile, eliminating inflammation, and preventing stone formation.
Intrahepatic gallbladder
is a common deviation. An independent anomaly has no clinical manifestations. There is a tendency to cholelithiasis. The clinical picture of cholecystocholangitis in this case has a number of features. There is a predominance of liver symptoms: rapid enlargement of the liver, increasing jaundice and fermentemia. With the development of acute cholecystitis, the symptoms resemble liver abscess. Ultrasound examination reveals the contours of the gallbladder surrounded by liver parenchyma. According to indications, cholecystostomy or cholecystectomy is performed.
Mobile gallbladder
covered on all sides by peritoneum and connected to the liver by the mesentery. This determines its mobility. The nature of the clinical manifestations is determined by the development of volvulus and its degree. Usually these are intense paroxysmal pain in the upper abdomen, accompanied by nausea and vomiting. If necrosis of the gallbladder develops, a picture of acute peritonitis appears with an increase in body temperature to high numbers, diffuse abdominal pain, vomiting, and positive symptoms of peritoneal irritation. For diagnosis, cholecystography is the most informative, which must be performed in a vertical and horizontal (on the back) position; sonography can also be used. In such a situation, emergency surgical intervention is necessary.
Among the anomalies of magnitude
Most often, hypoplasia of the gallbladder occurs, usually in combination with a hypoplastic cystic duct. This is most often observed in cystic fibrosis. There are no clinical manifestations. With an enlarged gallbladder, the development of dyskinetic disorders and inflammatory changes is possible, which leads to disruption of the passage of bile. In some cases, surgical treatment is indicated.
Shape anomalies
- constrictions or kinks of the gallbladder, leading to its deformation. When bent, the longitudinal axis is disrupted, the bladder curls up in the form of a snail, and it can be fixed with adhesions to the duodenum or transverse colon. When constriction occurs, narrowing of the gallbladder occurs along the entire circumference or part of it. Most often, constrictions and kinks are congenital. In most cases, this is due to a disproportion in the growth of the gallbladder and its bed. Deformations of the gallbladder play an important role in disrupting the passage of bile. The congestion caused by this over time leads to the development of dystrophic changes in the wall of the bladder and its contractile function. Various types of deformations of the gallbladder interfere with the normal function of the organ and disrupt motility, mainly of the hypotonic type. One of the most important factors influencing the function of a hollow organ is the structure of the outlet section, the outflow path. Congenital or acquired pathology in the cervical-ductal zone early and significantly affects the functional ability of the entire organ. In the compensation stage, sonographic examination can observe normal contractility of the bladder or hyperkinetic dyskinesia. However, the bladder's reserves are quickly depleted, and it becomes large and flabby. Chronic disruption of the outflow of bile can lead to the development of cholecystitis and stone formation. In clinical practice, it is not always possible to decide whether existing deformities are congenital or acquired. Acquired deformities, unlike congenital ones, are varied and sometimes bizarre. The contours of the bubble are uneven, and pointed protrusions are often found. To carry out differential diagnosis, sonography is used after taking a choleretic breakfast. If there is a congenital kink, the unusual shape of the gallbladder is preserved, but if the kink is caused by pericholecystitis, the shape of the bladder changes.
Abnormalities in the shape of the gallbladder may be associated with the presence of a diverticulum. A diverticulum is a sac-like protrusion of the bladder wall in a limited area. The protrusion itself develops as a result of the activity of the gallbladder. The basis for this is the local absence of the elastic frame of the wall. Clinically, this pathology can manifest itself as pain due to stagnation of bile. The narrower the opening between the diverticulum and the bladder cavity, the more likely stagnation is. This contributes to the development of inflammation and cholelithiasis. Sonographically and with cholegraphy, a clearly defined additional formation is revealed, which is not separated from the shadow of the bubble during polypositional examination. After taking a choleretic breakfast, the diverticulum contracts noticeably more slowly compared to the gallbladder. The main direction of treatment is the correction of dyskinesia and the prevention of inflammation.
Classification of diseases
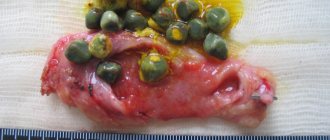
Gallstones
The main disease of the gallbladder is its dysfunction, that is, disruption of the organ’s functioning. However, the dysfunction itself has two types of classification:
- Slow or hypomotor dysfunction. Characteristic symptoms of this dysfunction are a feeling of pressure and fullness, dull aching pain under the ribs on the right, bitterness in the mouth, vomiting and constipation, flatulence and bloating.
- Hypermotor or rapid dysfunction. Most often it occurs against a background of increased stress or psycho-emotional overload. Pain with this type of dysfunction often radiates to the back or the heart area, provided that other common symptoms of the pathology of this organ persist.
The symptoms of each type depend not only on the cause of the complication, but also on the stage of development of the disease, on the degree of its neglect.
Treatment methods
The main task in identifying gallbladder pathologies is to normalize and stabilize the patient’s condition. Most often, this is enough to follow bed rest, a special diet and avoid stressful situations. The diet that doctors recommend when problems related to the gallbladder arise allows bile not to stagnate, but to empty all ducts in a timely manner.
The main idea of this diet is to split your daily diet into 5-6 servings of food, provided they are small. In addition, the last meal should be quite late, so that the problem organ disperses bile throughout the body even at night (during sleep). Healthy foods that can and should be consumed on a special diet that restores the functioning of the gallbladder are:
- Meat, poultry and fish
- Mushroom dishes
- Low-fat broths and soups
- Products containing natural fats in large quantities.
As a medicinal treatment for diseases, drugs such as atropine sulfate, Besalol and Eufillin help well. They are taken both in the form of intramuscular injections and in the form of capsules and tablets. For severe and persistent pain, it is recommended to take a painkiller - No-shpu or Papazol.
It should be noted that although the dosage of each drug is purely individual, the prescription of the drug for children differs significantly in quantity from the treatment for adults. To obtain more accurate information, you should carefully study the instructions included with the medication or consult your doctor.
Not only medications, but also ordinary herbs and herbs that are more gentle than chemicals will help relieve unpleasant symptoms of the gallbladder.
Herbs such as St. John's wort, valerian and mint, sage, calendula, thyme and chamomile, plantain, flax, celandine, and a number of others improve the performance of the diseased organ. Infusions brewed on the basis of these medicinal herbs can significantly improve the condition of the body (especially if you correctly combine traditional medicine and medications prescribed by a doctor).