Gastric outlet stenosis is a condition accompanied by mechanical obstruction (closure) of the pyloric portion of the stomach or duodenum.
Causes of mechanical obstruction
- Malignant tumors such as cancer of the antrum, pylorus and duodenum. In addition, compression of the outlet section by a tumor of the head of the pancreas or bile ducts, as well as enlarged lymph nodes, for example, with lymphoma, is possible.
- Peptic ulcer of the stomach and duodenum, both in the acute stage (due to inflammation of the walls and severe swelling), and in the chronic stage with the formation of coarse scar tissue in place of previously existing ulcers of the pyloric canal or duodenum.
- More rare causes of gastric outlet stenosis may be Crohn's disease, burn stenosis after consuming aggressive liquids (acid or alkali), or chronic pancreatitis.
Clinical picture
The most characteristic signs of gastric outlet stenosis are:
- Quick feeling of fullness while eating;
- Loss of body weight;
- Nausea and vomiting after eating (without bile!);
- Belching of air with an acidic taste;
- Discomfort and pain in the epigastrium;
- Feeling of fullness in the stomach;
- “Splashing noise” is caused by jerky movements of the abdominal wall in the epigastric region with the tips of 2-3 fingers. “Splashing noise” appears when there is a significant amount of liquid and gas in the stomach (more clearly detected using a phonendoscope).
Symptoms of stenosis
At the compensation stage there are no pronounced signs. There is heartburn, heaviness in the stomach, belching. Vomiting is rare and provides relief.
At the stage of subcompensation, symptoms intensify. Rotten belching appears, heaviness in the abdomen becomes stronger, patients complain of frequent vomiting, colicky abdominal pain. Since vomiting improves the condition, patients often induce it themselves. In this regard, loss of body weight occurs.
Decompensation is the progression of the disease. Stomach dysfunction forms, the person’s general condition deteriorates greatly, he is tormented by constant vomiting, which does not improve his well-being as it was before. Emetics
- the masses have an unpleasant odor because the food masses ferment in the stomach for a long time. The heaviness in the abdomen becomes very strong, patients move little and suffer from exhaustion. At this stage also:
- mucous membranes and skin become dry;
- dehydration appears;
- mineral metabolism is disrupted;
- dizziness, weakness, and fainting occur;
- pulse quickens;
- blood pressure decreases;
- Paralysis of the diaphragm may develop, resulting in respiratory arrest and death.
Diagnostic methods
The gastroenterologist prescribes the following examinations:
- blood and urine tests;
- X-ray of the digestive system with contrast;
- FGDS.
Diagnostics
Diagnostic criteria for gastric outlet stenosis:
- Clinical – the presence of symptoms of impaired gastric emptying, weight loss, signs of water and electrolyte imbalance.
- Laboratory tests - increased hematocrit, signs of metabolic hypochloremic alkalosis, hypokalemia, hypochloremia, decreased concentration of ionized calcium, hypoproteinemia, signs of metabolic alkalosis, in severe cases - azotemia.
- Instrumental - probing the stomach - evacuation of a large amount of contents with a sour or “rotten egg” smell.
- Endoscopic - narrowing of the lumen of the pyloric part of the stomach and the initial part of the duodenum.
- X-ray – slowdown or lack of evacuation of contrast from the stomach, retention of contrast in the stomach.
Photo 1: X-ray of the esophagus and stomach with barium for stenosis of the gastric outlet. Photo 2: endoscopic picture of pyloric stenosis of ulcerative etiology.
How is stenosis detected?
If stenosis is suspected, the doctor may order the following tests:
- X-ray and fluoroscopy (including contrast-enhanced).
- Angiography is radiography with the introduction of a radiopaque solution into the vessels.
- Computed tomography (CT) and magnetic resonance imaging (MRI). These studies can also be performed with contrast enhancement.
- Ultrasound examination (ultrasound). Dopplerography is also performed - studying blood flow in vessels using ultrasound.
- Endoscopic studies, for example, fibroesophagogastroduodenoscopy (FEGDS) to detect stenosis of the esophagus, stomach, duodenum.
Classification
By etiology:
- due to benign diseases;
- due to malignant diseases.
By stage of development:
- compensated;
- subcompensated;
- decompensated.
Complications:
- hypovolemic shock;
- acute gastrointestinal bleeding (ulcerative or mucosal ruptures due to repeated vomiting);
- perforation of an ulcer or tumor;
- spontaneous rupture of the stomach.
What are the causes of stenosis?
There are many different causes of stenosis. The main ones:
- Congenital malformations (for example, congenital urethral valves, congenital intestinal obstruction due to intestinal underdevelopment).
- Proliferative inflammation of the organ wall is an inflammatory process in which tissue proliferation occurs.
- Scarring of the organ wall after damage, inflammation, or ulcers.
- Benign and malignant tumors.
- In vessels, the cause of stenosis is often blood clots and atherosclerotic plaques.
- Compression of a hollow organ from the outside, for example, by a tumor located in a neighboring organ.
- Hypertrophy of the organ wall - for example, this condition often causes narrowing of the pylorus of the stomach.
- Injuries and osteophytes (bone growths) can cause stenosis of bone canals, in particular the spinal canal.
Treatment
Treatment of gastric stenosis is surgical. The goal of surgical treatment of gastric outlet stenosis is to eliminate the stenosis and restore passage through the stomach and duodenum.
Patients with sub- and decompensated stenosis require comprehensive preoperative preparation, including correction of water-electrolyte metabolism, protein composition, volemic disorders, and activity of the cardiovascular system; as well as gastric lavage and decompression.
Patients without pronounced disorders of gastric motility (stages of developing and compensated stenosis) can be operated on after a relatively short (5-7 days) period of preoperative preparation (anti-ulcer therapy, gastric decompression).
The choice of surgical intervention is determined by the disease that led to the formation of obstruction of the gastric outlet tract.
- In case of malignant etiology of the disease, examination and treatment are carried out in accordance with oncological recommendations for gastric cancer. For tumor stenosis, subtotal proximal resection or gastrectomy in combination with lymphadenectomy is performed.
- For cicatricial stenoses of benign origin, it is necessary to perform either organ-preserving drainage operations (pyloroplasty in various modifications, gastrojejunostomy bypass) or distal gastrectomy. In case of ulcerative stenosis, a standard resection of 2/3 of the stomach is performed with an anastomosis according to Billroth 1 or Billroth 2 in various modifications, depending on the conditions for the anastomosis and the formation of the duodenal stump. All surgical treatment options are possible using minimally invasive technologies in the absence of contraindications.
Pyloroplasty according to Heineke-Mikulicz
Treatment of stenosis of the stomach and duodenum
Treatment is always surgical. Before the operation, the metabolism is adjusted. To do this, the patient is injected with solutions of dextran, albumin, glucose, saline solution, and electrolyte solution. In addition, it is necessary to constantly remove the contents of the stomach through a tube to reduce pressure on its walls. To replenish energy losses, patients are prescribed parenteral nutrition. About a week after such preparation, the operation is performed. This may be gastric resection, expansion of the duodenum, vagotomy, etc.
The prognosis depends on the stage of the disease. With late diagnosis, complications that are incompatible with life develop.
Treatment in the department of thoracoabdominal surgery and oncology
Treatment in the department is carried out under the programs of compulsory medical insurance, voluntary medical insurance, VMP, as well as on a commercial basis. Read how to get treatment at the Department of Thoracoabdominal Surgery and Oncology of the Russian Scientific Center for Surgery.
To schedule a consultation, call:
+7 (499) 248 13 91 +7 (903) 728 24 52 +7 (499) 248 15 55
Submit a request for a consultation by filling out the form on our website and attaching the necessary documents.
Causes of development of pyloric stenosis
One of the reasons for the development of gastric stenosis is a scar, consisting of connective tissue and formed during the healing process of a peptic ulcer. It tightens the wall of the stomach, making it inactive.
Another reason for the development of stenosis may be intramural cancer. The neoplasm grows into the tissue, as a result of which the lumen of the gastrointestinal tract narrows. Food moving through the digestive tract cannot reach the intestines in full. It stagnates. To evacuate the contents from the stomach, the muscular layer begins to grow. This compensates for the stenosis to some extent.
However, over time, the hypertrophied muscular layer of the stomach cannot cope with the load, and an increase in the volume of stomach contents leads to its stretching. As a result of stagnation, food under the influence of microbes begins to decompose and ferment.
The disease has the following stages:
- First stage
– compensated pyloric stenosis. The hole is narrowed slightly. The patient complains of belching with a sour taste and a feeling of a full stomach after eating. Occasionally, vomiting occurs, which brings a feeling of relief for a short time. The patient's condition is generally satisfactory.
- Second stage
– stage of subcompensation. The patient already has a constant feeling of a full stomach, which is combined with belching and pain. Vomiting occurs after a while or immediately after eating and brings relief. Over time, a person loses weight. When palpating and examining the abdomen, a splashing noise is heard in the navel area.
- Third stage
– stage of decompensation. Over time, the disease progresses, the stomach is distended. The condition worsens significantly, exhaustion and dehydration develop. Vomiting occurs frequently and does not bring relief. The vomit is in large quantities, foul-smelling, and contains large quantities of the remains of many days' food.
Congenital pyloric stenosis
In children, congenital pyloric stenosis can be found. Often the disease is hereditary. With stenosis, there is a proliferation of connective tissue in the area of the excretory section of the stomach. It is the most common cause of gastric obstruction in infants, with boys being affected four times more often than girls.
The disease appears in the second to fourth week of life. The main symptom is frequent and severe “fountain” vomiting some time after feeding. Treatment is only surgical. The prognosis after surgery is favorable provided that treatment is started in a timely manner.
Stages or degrees of laryngeal stenosis
Regardless of the form of laryngeal stenosis, acute or chronic, doctors distinguish stages or degrees of the disease. The stage of development of stenosis determines the danger posed by the disease:
1. First stage. Stenosis always develops from the first stage. There is a narrowing of the respiratory lumen, but breathing disturbances are still barely noticeable. Shortness of breath may occur during exercise. When diagnosing first degree laryngeal stenosis, as a rule, treatment always gives a positive result.
2. Second stage. In the second stage, the glottis noticeably decreases, and typical symptoms of laryngeal stenosis begin to appear - shortness of breath at rest, noise during breathing, skin changes color, children become restless.
3. Third stage. The diameter of the gap is minimal, shortness of breath no longer goes away. It becomes difficult to breathe, and lying down is almost impossible; there is a significant lack of air. The voice may disappear completely, there is severe sweating, and a high pulse.
4. Fourth stage. The glottis is likely to close completely, leading to complete cessation of breathing. If a person is able to breathe, then breathing is rare and very heavy. Convulsions occur and loss of consciousness is possible. Immediate help and surgical intervention are required.
How does the gastrointestinal tract function after gastric resection?
The stomach takes part in hematopoiesis; the cells of the gastric mucosa produce intrinsic Castle factor, an enzyme that converts vitamin B12 from food into an absorbable form. Without intrinsic factor, vitamin B12 is not absorbed and does not enter the bloodstream, but is excreted in the feces. The source of vitamin B12 is animal food; there are no plant sources of B12. For more information about B12 deficiency anemia, read the article in the healthy lifestyle “Red vitamin and anemia (if blood is on a fast ration)” or on the website.
The first blow from food intake is the intestines, primarily the small intestine - this is the most extensive organ of the human digestive system. In it, under the influence of pancreatic enzymes and bile of intestinal juice, the main processes of digestion occur, transforming food into simple components that can be absorbed by the body, determine the state of metabolic processes and, ultimately, human health.
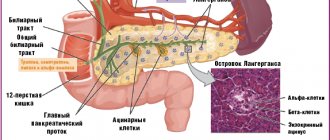
Pancreas. It produces 1.5-2.0 liters of pancreatic juice, which has a pH of 7.5. The main part of pancreatic juice is pancreatic enzymes (trypsin, chymotrypsin, elastase, carboxypeptidases, pancreatic lipase, phospholipases, etc.) Pancreatic juice contains a huge range of enzymes that digest almost all components (macronutrients) of food consumed by humans. These enzymes are produced only in the pancreas. In practice, the pancreas takes over the functions of the stomach in digesting protein foods.
Large intestine - carries out residual final digestion of food, secretion and absorption of water, electrolytes, gases, formation and evacuation of feces.
An important role is played by intestinal microflora, the enzymes of which utilize digestive enzymes secreted by the digestive organs. The breakdown products of enzymes and bile acids are absorbed into the blood and returned to the digestive organs for the re-synthesis of digestive enzymes and acids.
Therapeutic nutrition for problems with the stomach and intestines
Therapeutic nutrition for stomach problems has a positive effect.
This article has already mentioned such a principle of healthy eating as mechanical sparing. As a rule, it is used in cases where the disease of the gastrointestinal tract is in the acute stage, and the patient’s digestive process is difficult.
One of the most common tools for performing mechanical sparing is rubbing any food prepared for the patient.
Of course, if we are talking about a chronic illness, not only the form of serving the dish plays a role, but also the composition of the products included in it. Below is one of the options for a gentle diet suitable for patients suffering from serious stomach or intestinal problems:
- First breakfast: viscous rice porridge cooked in milk; soft-boiled egg; tea with milk.
- Second breakfast: baked apple (possibly with added sugar).
- Lunch: oatmeal soup cooked with milk; carrot puree; lean meat meatballs cooked in a double boiler; fresh fruit mousse.
- Afternoon snack: wheat flour crackers; rosehip decoction.
- Dinner: mashed potatoes; fish (boiled or baked with milk sauce); tea with milk.
- Before bed: a glass of something dairy (cream, non-acidic yogurt, acidophilus, etc.).
There is a version of the described diet that does not involve rubbing the food. It is suitable for those patients whose disease is sluggish, without causing significant discomfort. Sample menu:
Features of treatment of stenosis. Prevention and diet therapy
This disease inherently represents a number of pathological changes and conditions. All of them are characterized by different symptoms and pathogenesis. All that unites them is only a narrowing or complete closure of the lumen of the vascular units of the body, as well as cavities and organ systems.
The mechanism of stenosis and its features
There are such types of stenosis as:
- Hereditary. Usually manifests itself as a result of congenital distortion of anatomical features.
- Acquired disorders. As a rule, their causes are metabolic disorders. However, infectious and inflammatory reactions, as well as possible neoplasms, should not be ruled out.
- Combined stenosis. This type is represented by a combination of the first and second factors. In this case, many organs are affected by narrowing (larynx, bronchi, arteries, trachea, etc.)
Types of stenosis:
- Spinal stenosis. It is a narrowing of the annals of the spinal cord, which leads to an impressive number of complications; problems with the spine
. It is both a congenital feature and an acquired disease. According to anatomy, it is divided into central and lateral. - Vascular stenosis. The cause of this type is damage to the arteries by cholesterol plaques.
- Stenosis of the trachea and larynx. It is characterized by a narrowing of the lumen in the respiratory tract, causing respiratory dysfunction.
- Pyloric stenosis. Or its other name is gastric stenosis. As a rule, the disease develops in the presence of an ulcer, causing spasms and narrowing of the spaces between the walls of the stomach.
Stenosis in centuries-old practice
Nowadays, the classical understanding of stenosis is considered to be pathological processes associated with an anomaly of narrowing of the great vessels. The ethology of the phenomenon is based on atherosclerotic processes, which are a consequence of the formation and sedimentation of cholesterol plaques on the walls of blood vessels. A deficiency of nutrients and oxygen elements in the blood has a detrimental effect on organs and leads to serious health problems.
From this we can conclude that even a person who has little knowledge of medicine can imagine how dangerous this pathology is. It is worth knowing that forms of stenosis diagnosed in time can be successfully treated surgically. Age-old practice shows that an integrated approach to the treatment of stenosis produces results immediately. In addition to surgical intervention and drug therapy, it is worth considering traditional methods that have been used for many generations. Therapeutic complexes of home therapy can be safely included in the basis of methods for the successful treatment of various types of stenosis.
Traditional medicine as one of the methods of treatment
Cleaning vessels of accumulated waste and toxins can be successfully carried out by using natural components and materials. There are a huge variety of plants that have the ability to dissolve cholesterol plaques and deposits. The ability to eliminate pathologies of arterial loops and level out anatomical disorders is the main advantage for resorting to traditional medicine at home.
In addition to drug therapy, infusions and decoctions will have an excellent effect on the body as a whole, because plant materials can replenish the required amount of nutrients and strengthen the vascular system, while normalizing the body's metabolic processes. Herbal recipes will improve the absorption of micro- and macroelements, increasing the level of vitamins. Another advantage of using traditional medicine is the convenience and ease of preparing the necessary recipes.
Prevention using traditional methods. Diet therapy
Traditional methods cannot completely cure such a serious disease as stenosis. However, it is possible to improve the patient’s general condition by getting rid of problems such as back pain
, breathing problems and reduce the number of cramps in the stomach.
- Coltsfoot tincture will improve the functioning of the digestive glands. To prepare it you will need 1 teaspoon of a mixture of flowers and leaves, poured with 200 grams of boiling water. To ensure complete readiness, leave the resulting solution for 30-40 minutes and strain. Take this recipe before meals, 100 ml.
- A decoction of golden mustache will help in the treatment of atherosclerotic conditions. All that is required is to mix golden mustache juice with plantain juice in a ratio of 1:20, bring to a boil in a steam bath and store in a dark place. Taken exclusively in the first half of the day after meals.
- Tincture of white onions with honey perfectly prevents blockage of blood vessels with blood clots. White onion juice is mixed with honey in equal parts and infused for 20 days in a cool, dark room. Take 1 tablespoon three times a day before meals. The course of therapy is 6 weeks.
- In certain cases, gruel from grated raw potatoes has a beneficial effect in an integrated approach to the treatment of stenosis. It is necessary to consume 20-30 minutes before meals, without peeling the peel, but rinsing it thoroughly.
In addition to folk recipes, the main component of successful treatment is diet.
Proper nutrition will have the best effect on the body, reducing the effects of fatty plaques on the arteries and blood vessels. First of all, it is necessary to dilute the diet with vegetables and fruits, and also reduce the consumption of spicy and fatty foods. Eliminating salt and giving up bad habits is another important factor in the treatment of stenosis. All these simple rules will help create optimal diet therapy and improve immunity, which in the future will be a huge plus not only for improving well-being, but also for the body as a whole. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
A gentle diet for reduced gastric secretion
With reduced gastric secretion - a gentle diet.
Speaking about gentle diets, one cannot fail to mention their special type. We are talking about a diet in which there is a targeted stimulation of the secretion of gastric juice.
It is important to understand that such a diet can only be prescribed by a doctor and only after the patient has been given a specific diagnosis.
So, what are the basic principles of this diet? Firstly, this is the selection of certain foods that stimulate the patient’s digestion.
Secondly, creating the “right” surroundings when eating (scientists have proven that pleasant smells, a calm atmosphere and beautiful table setting can increase the production of gastric juice).
What foods are allowed to be consumed by patients on this type of gentle diet? For such patients, doctors recommend including in their diet soups with low-fat broths (fish, meat, vegetable or even mushroom), borscht, cabbage soup and beetroot soup, jellies, low-fat ham and mild cheese, soaked herring and fresh caviar (sturgeon or chum salmon), tomatoes and herbs and spices.
The latter, of course, in moderation. But flour (especially puff pastry and pastry products) and dairy, fatty, smoked and overly salted, hard-boiled eggs and, in addition, some fruits, berries and vegetables (for example, grapes, gooseberries, radishes, radishes, peas and beans) cannot be consumed within the described diet.
The patient is also advised to exclude any carbonated drinks from his diet. Usually, doctors themselves help patients navigate the list of restrictions, giving them an approximate menu for the day. Below is one of the possible options for eating on a schedule:
- Breakfast: oatmeal cooked with milk; soft-boiled egg; cheese; tea.
- Lunch: meat broth seasoned with noodles; fried meat cutlets without breading; carrot puree; jelly.
- Afternoon snack: cookies; rosehip decoction.
- Dinner: jellied fish; rice pudding with fruit gravy; tea.
- Before bed: a glass of kefir or other fermented milk drink.