A state of shock occurs when there is a sudden disruption of the usual blood circulation. This is a severe stress reaction of the body, which has failed to manage vital systems. Hemorrhagic shock is caused by sudden blood loss. Since blood is the main fluid that supports metabolism in cells, this type of pathology refers to hypovolemic conditions (dehydration). In ICD-10 it is regarded as “Hypovolemic shock” and is coded R57.1.
In the origin of hemorrhagic shock, it is important to exclude the slow loss of blood, even of a significant volume. It has been established that hemodynamic disturbances with a gradual loss of up to 1.5 liters do not lead to serious consequences. This is due to the inclusion of compensation mechanisms.
In conditions of sudden bleeding, an unreplaced volume of 0.5 liters is accompanied by acute tissue oxygen deficiency (hypoxia).
Most often, blood loss is observed during injuries, surgical interventions, and in obstetric practice during labor in women.
What mechanisms determine the severity of shock?
In the development of pathogenesis, compensation for blood loss is important:
- state of nervous regulation of vascular tone;
- the ability of the heart to work under hypoxic conditions;
- blood clotting;
- environmental conditions for additional oxygen supply;
- level of immunity.
It is clear that a person with chronic diseases has a much lower chance of suffering massive blood loss than a previously healthy person. The work of military doctors during the Afghan war showed how severe moderate blood loss is for healthy soldiers in high altitude conditions, where air oxygen saturation is reduced.
Rapid transportation of the wounded using armored personnel carriers and helicopters saved many soldiers
On average, a person constantly circulates about 5 liters of blood through arterial and venous vessels. In this case, 75% is in the venous system. Therefore, the subsequent reaction depends on the speed of adaptation of the veins.
A sudden loss of 1/10 of the circulating mass does not make it possible to quickly “replenish” reserves from the depot. Venous pressure drops, which leads to maximum centralization of blood circulation to support the work of the heart, lungs and brain. Tissues such as muscles, skin, and intestines are recognized by the body as “superfluous” and are turned off from the blood supply.
During systolic contraction, the ejected volume of blood is insufficient for tissues and internal organs; it only supplies the coronary arteries. In response, endocrine protection is activated in the form of increased secretion of adrenocorticotropic and antidiuretic hormones, aldosterone, and renin. This allows you to retain fluid in the body and stop the urinary function of the kidneys.
At the same time, the concentration of sodium and chlorides increases, but potassium is lost.
Increased synthesis of catecholamines is accompanied by vascular spasm in the periphery, and vascular resistance increases.
Due to circulatory hypoxia of tissues, “acidification” of the blood occurs with accumulated toxins—metabolic acidosis. It promotes an increase in the concentration of kinins, which destroy vascular walls. The liquid part of the blood enters the interstitial space, and cellular elements accumulate in the vessels, creating all the conditions for increased thrombus formation. There is a risk of irreversible disseminated intravascular coagulation (DIC syndrome).
The heart tries to compensate for the necessary output by increasing contractions (tachycardia), but there are not enough of them. Potassium loss reduces myocardial contractility and heart failure develops. Blood pressure drops sharply.
Replenishing the volume of circulating blood can prevent general microcirculation disorders. The patient’s life depends on the speed and completeness of emergency measures.
Causes
The cause of hemorrhagic shock is acute bleeding.
Traumatic pain shock is not always accompanied by significant blood loss. It is more characterized by a widespread lesion surface (extensive burns, combined fractures, tissue crushing). But the combination with uncontrolled bleeding aggravates the effect of damaging factors and aggravates the clinical course.
In pregnant women, urgent diagnosis of the cause of shock is important
Hemorrhagic shock in obstetrics occurs during difficult labor, during pregnancy, and in the postpartum period. Massive blood loss is caused by:
- ruptures of the uterus and birth canal;
- placenta previa;
- with the normal position of the placenta, its premature detachment is possible;
- abortion;
- uterine hypotension after childbirth.
In such cases, bleeding is often combined with another pathology (trauma during labor, gestosis, concomitant chronic diseases of the woman).
List of sources
- Bratus V.D., Sherman D.M. Hemorrhagic shock, pathophysiology and clinical aspects. Kyiv: Nauk. Dumka. 1989.
- Gakaev D. A. Pathophysiological changes in the body during acute blood loss [Text] // Medicine and healthcare: materials of the IV International. scientific conf. (Kazan, May 2016). - Kazan: Buk, 2016. - pp. 37-40.
- Vorobyov A.I., Gorodetsky V.M., Shulutko E.M., Vasiliev S.A. Acute massive blood loss. M.: GEOTAR-MED, 2001.
- Bryusov P.G. Emergency infusion-transfusion therapy for massive blood loss / P.G. Bryusov // Hematology and transfusiology. –1991. – No. 2. – P. 8-13.
- Stukanov M.M. Comparative assessment of infusion therapy options in patients with hemorrhagic shock / M.M. Stukanov et al. //Anesthesiology and resuscitation. – 2011. – No. 2. – P. 27-30.
Clinical manifestations
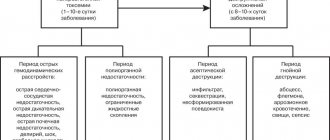
The clinical picture of hemorrhagic shock is determined by the degree of impaired microcirculation and the severity of cardiac and vascular insufficiency. Depending on the stage of development of pathological changes, it is customary to distinguish the stages of hemorrhagic shock:
- Compensation or the first stage - blood loss is no more than 15–25% of the total volume, the patient is fully conscious, he answers questions adequately, upon examination, attention is drawn to pallor and coldness of the skin of the extremities, a weak pulse, blood pressure at the lower limits of normal , heart rate increased to 90–110 per minute.
- The second stage, or decompensation, - in accordance with the name, symptoms of oxygen deficiency in the brain and weak cardiac output appear. Typically, acute blood loss ranges from 25 to 40% of the total circulating blood volume. The failure of adaptive mechanisms is accompanied by a disturbance in the patient’s consciousness. In neurology it is regarded as soporous, there is inhibition of thinking. There is pronounced cyanosis on the face and limbs, the hands and feet are cold, the body is covered with sticky sweat. Blood pressure (BP) drops sharply. The pulse is weakly filled, characterized as “thread-like”, frequency up to 140 per minute. Breathing is frequent and shallow. Urinary excretion is sharply limited (up to 20 ml per hour). Such a reduction in the filtration function of the kidneys is called oliguria.
- The third stage is irreversible - the patient’s condition is regarded as extremely serious, requiring resuscitation measures. There is no consciousness, the skin is pale, with a marbled tint, blood pressure is not determined or only the upper level can be measured within 40–60 mm Hg. Art. The pulse on the ulnar artery cannot be felt, but with sufficiently good skills it can be felt on the carotid arteries, heart sounds are muffled, tachycardia reaches 140–160 per minute.
Tests and diagnostics
The diagnosis of hemorrhagic shock is established based on examination of the patient (presence of fractures, external bleeding) and clinical symptoms reflecting the adequacy of hemodynamics (color and temperature of the skin, changes in pulse and blood pressure, calculation of the shock index, determination of hourly diuresis) and laboratory test data, including: determination CVP, hematocrit , blood CBS (indicators of acid-base status).
Establishing the fact of blood loss due to external bleeding does not present any difficulties. But in its absence and suspicion of internal bleeding, it is necessary to take into account a number of indirect signs: in case of pulmonary hemorrhage - hemoptysis; for stomach and duodenal ulcers or intestinal pathology - vomiting “coffee grounds” and/or melena; in case of damage to parenchymal organs - tension of the abdominal wall and dullness of percussion sound in the sloping parts of the abdomen, etc. If necessary, instrumental studies are prescribed: ultrasound, radiography, MRI, laparoscopy, consultations with various specialists are prescribed.
It should be borne in mind that the assessment of the volume of blood loss is approximate and subjective, and if it is assessed inadequately, you can miss the permissible waiting interval and find yourself faced with the fact that a picture of shock has already developed.
How is the degree of blood loss determined?
In diagnosis, it is most convenient for the doctor to use objective signs of shock. The following indicators are suitable for this:
- circulating blood volume (CBV) - determined in the laboratory;
- shock index.
It has been proven that the body can completely restore the loss of ¼ of the blood volume on its own. And with the rapid disappearance of half the volume, compensatory reactions fail. Recovery is only possible with the help of treatment.
Death occurs with a sharp decrease in blood volume by 60% or more.
To state the severity of the patient, there is a classification associated with minimal capabilities in determining hypovolemia based on laboratory and clinical signs.
| Degree of shock (hypovolemia) | % loss of bcc | Blood loss in ml | Decrease in systolic blood pressure |
| light | from 15 to 25 | 700–1300 | by 10% of the operating level |
| medium-heavy | from 25 to 35 | 1300–1800 | up to 90–100 mm Hg. |
| heavy | up to 50% | 2000–2500 | 60 mmHg Art. |
The given indicators are not suitable for assessing the severity of shock in children. If a newborn baby’s total blood volume barely reaches 400 ml, then for him a loss of 50 ml is quite similar to 1 liter in an adult. In addition, children suffer from hypovolemia much more severely, since their compensation mechanisms are poorly expressed.
Any medical professional can determine the shock index. This is the ratio of the calculated heart rate to the systolic pressure. Depending on the obtained coefficient, the degree of shock is roughly judged:
- 1.0 - light;
- 1.5 - medium-heavy;
- 2.0 - heavy.
Laboratory values in diagnosis should indicate the severity of anemia. For this purpose the following are determined:
- hemoglobin,
- number of red blood cells,
- hematocrit
For timely choice of treatment tactics and recognition of a severe complication in the form of disseminated intravascular coagulation syndrome, the patient is determined by coagulogram parameters.
Monitoring diuresis is necessary in the diagnosis of kidney damage and filtration disorders.
What is infusion therapy?
Infusion therapy does not mean replacing lost blood with donor blood. The slogan “a drop for a drop”, which provided for complete replacement, and sometimes even with interest, has long gone into oblivion. Donor blood transfusion is a serious operation that involves the transplantation of foreign tissue, which the patient’s body may not accept. Transfusion reactions and complications are even more difficult to deal with than acute blood loss, which is why whole blood is not transfused. In modern transfusiology, the issue of infusion therapy is solved differently: blood components are transfused, mainly fresh frozen plasma and its preparations (albumin)
. The rest of the treatment is supplemented by the addition of colloidal plasma expanders and crystalloids.
The goal of infusion therapy for acute blood loss:
- Restoring normal circulating blood volume;
- Replenishing the number of red blood cells, as they carry oxygen;
- Maintaining the level of coagulation factors, since the hemostatic system has already responded to acute blood loss.
It makes no sense for us to dwell on what a doctor’s tactics should be, since this requires certain knowledge and qualifications. However, in conclusion, I would also like to note that infusion therapy provides various ways of its implementation. Puncture catheterization requires special care for the patient, so you need to be very attentive to the slightest complaints of the patient, since complications may also occur here.
How to provide assistance at the prehospital stage?
First aid actions against the background of detected acute bleeding should be aimed at:
- measures to stop bleeding;
- prevention of hypovolemia (dehydration).
Applying a belt to a maximally bent arm helps stop bleeding from the vessels of the shoulder and forearm
Help for hemorrhagic shock cannot be done without:
- application of hemostatic dressings, tourniquets, immobilization of the limb for injuries of large vessels;
- placing the victim in a lying position; with a mild degree of shock, the victim may be in a euphoric state and inadequately assess his well-being and try to get up;
- if possible, replenish fluid loss by drinking plenty of fluids;
- warming up with warm blankets and heating pads.
An ambulance must be called to the scene of the incident. The patient’s life depends on the speed of action.
Treatment of hemorrhagic shock begins in an ambulance
The doctor’s algorithm of action is determined by the severity of the injury and the patient’s condition:
- checking the effectiveness of a pressure bandage, tourniquet, applying clamps to blood vessels for open wounds;
- installation of systems for transfusion into 2 veins, if possible, puncture of the subclavian vein and its catheterization;
- establishing a fluid transfusion to quickly restore the volume of blood volume; in the absence of Reopoliglyukin or Poliglyukin, a normal saline solution will do for the duration of transportation;
- ensuring free breathing by fixing the tongue, installing an air duct, if necessary, intubation and transfer to mechanical breathing or using a hand-held Ambu bag;
- carrying out pain relief using injections of narcotic analgesics, Baralgin and antihistamines, Ketamine;
- administration of corticosteroids to support blood pressure.
The ambulance must ensure the fastest possible (with a sound signal) delivery of the patient to the hospital, inform by radio or telephone about the arrival of the victim so that the reception staff is ready.
Video about the principles of first aid for acute blood loss:
Acute blood loss. What to do?
{banner_banstat9}
As a rule, first aid in case of bleeding caused by injuries is provided by people who are nearby at that moment. Sometimes they are just passers-by. And sometimes a person has to do this himself if trouble strikes him far from home: while fishing or hunting, for example. The very first thing to do is to try to stop the bleeding using the available means or by pressing the vessel with your fingers.
However, when using a tourniquet, you should remember that it should not be applied for more than 2 hours, so a note is placed under it indicating the time of application.
In addition to stopping the bleeding, pre-medical care also consists of carrying out transport immobilization if fractures occur, and ensuring that the patient falls into the hands of professionals as soon as possible, that is, it is necessary to call a medical team and wait for its arrival.
Emergency care is provided by medical professionals and consists of:
- Stop the bleeding;
- Assess the degree of hemorrhagic shock, if it occurs;
- Replace the volume of circulating blood by infusing blood substitutes and colloidal solutions;
- Carry out resuscitation measures in case of cardiac and respiratory arrest;
- Transport the patient to the hospital.
The sooner a patient gets to the hospital, the better his chances of life, although even in a hospital setting it is difficult to treat acute blood loss, since it never leaves time for reflection, but requires quick and clear action. And, unfortunately, he never warns of his arrival.
Basics of therapy for hemorrhagic shock
In a hospital setting, shock therapy is provided by a set of measures aimed at counteracting the damaging mechanisms of pathogenesis. It is based on:
- maintaining continuity of care with the prehospital stage;
- continuation of replacement transfusion with solutions;
- measures to completely stop bleeding;
- adequate use of medications depending on the severity of the injury;
- antioxidant therapy - inhalation of a humidified oxygen-air mixture;
- warming the patient.
Reopolyglucin normalizes platelet aggregation and serves as a prevention of DIC syndrome
When a patient is admitted to the intensive care unit:
- catheterization of the subclavian vein is carried out, a jet injection of Polyglyukin is added to the drip infusion of saline solution;
- Blood pressure is constantly measured, the heart rate is noted on the cardiac monitor, and the amount of urine excreted through the catheter from the bladder is recorded;
- during vein catheterization, blood is taken for urgent analysis to determine the degree of loss of blood volume, anemia, blood type and Rh factor;
- after the tests and diagnosis of the moderate stage of shock are ready, donor blood is ordered, tests are performed for individual sensitivity and Rh compatibility;
- if the biological test is good, blood transfusion is started; in the early stages, transfusion of plasma, albumin or protein (protein solutions) is indicated;
- In order to eliminate metabolic acidosis, an infusion of sodium bicarbonate is necessary.
If surgical intervention is necessary, the issue of its urgency is decided collectively by surgeons, and the possibility of anesthesia is also determined
Diagnostic measures
Diagnostic measures for hemorrhagic shock are aimed at determining the amount of blood lost. The patient's appearance cannot provide objective data. Therefore, to clarify the stage of shock, 2 methods are used:
- Indirect methods. Determination of blood loss is carried out using a visual examination of the patient and assessment of the functioning of the main organs and systems: the presence of pulsation, blood pressure, skin color and breathing patterns.
- Direct methods. The essence of the methods is to determine the weight of the patient himself or the materials used to stop the bleeding.
Indirect techniques for assessing the patient's condition can help calculate the shock index. To do this, you need to determine the victim’s vital signs and compare them with approximate indicators of the degree of blood loss. The shock index is usually determined at the stage before hospitalization. In a hospital setting, diagnostic data are clarified using laboratory tests.
How much blood should be transfused?
During blood transfusion, doctors use the following rules:
- for blood loss of 25% of the bcc, compensation is possible only with blood substitutes, and not with blood;
- for newborns and small children, the total volume is half combined with the erythrocyte mass;
- if the BCC is reduced by 35%, it is necessary to use both red blood cells and blood substitutes (1:1);
- the total volume of transfused fluids should be 15–20% higher than the specified blood loss;
- if severe shock is detected with a loss of 50% of blood, then the total volume should be twice as large, and the ratio between red blood cells and blood substitutes should be maintained as 2:1.
Indications for stopping the continuous infusion of blood and blood substitutes are:
- no new signs of bleeding within three to four hours of observation;
- restoration of stable blood pressure numbers;
- presence of constant diuresis;
- compensation of cardiac activity.
If there are wounds, antibiotics are prescribed to prevent infection.
Cardiac glycosides and osmotic diuretics such as Mannitol are used very carefully when blood pressure is stabilized and there are no contraindications based on ECG results.
Urgent measures
Emergency care for hemorrhagic shock is based on 2 main tasks:
- Stop blood loss;
- Prevent dehydration.
Considering that in case of extensive bleeding, its immediate stop is required, the algorithm for urgent actions will be as follows:
- Use a tourniquet or special constriction bandages to stop bleeding;
- Keep the injured part of the body immobile;
- Lay the victim down, since in the presence of the first stage of shock the patient is in a state of euphoria and may attempt to move independently;
- Let the person drink as much pure water without gases as possible;
- Warm him up using any available means: blankets, clothes, heating pads.
Remember!
Regardless of the patient's condition, if hemorrhagic shock is suspected, medical professionals should be called immediately. His life depends on how quickly professionals begin to provide emergency assistance to the victim.
Actions of professionals
To prevent the onset of a serious complication, medical care begins to be provided on the way to the medical facility. When stopping bleeding, therapeutic measures are carried out in parallel, which consist of performing three actions:
- To restore the necessary balance in the blood system and stabilize cell membranes, catheters are installed in peripheral veins;
- To maintain gas exchange and the required patency in the respiratory organs, a special probe is installed. In case of emergency, use a device for artificial ventilation of the lungs;
- Catheters are installed in the bladder area.
After the victim is taken to a medical facility, diagnostic measures are carried out to determine the severity of the shock, and then intensive care is started. The actions of medical personnel are carried out according to the emergency algorithm:
- The necessary laboratory tests are carried out;
- Preventive measures are started urgently to prevent the development of hypoglycemia and Wernicke encephalopathy;
- In case of emergency, narrow-profile antidotes are used;
- Eliminate swelling of the meninges and reduce intracranial pressure;
- Use symptomatic therapy aimed at eliminating convulsions and vomiting;
- During the period of stabilization of the patient's condition, it is mandatory to monitor blood pressure, pulse, cardiac activity, and the amount of urine excreted.
It should be noted that the therapy itself is carried out only after the patient’s condition has stabilized. The standard set of drugs that improve blood flow replenishment is as follows:
- Vitamin C and medicines containing it;
- Ganglion blockers to relieve the effects of venous spasms;
- In order to improve cardiac metabolism, riboxin, carvetin and cytochrome are used;
- Developing heart failure may require the addition of prednisone and hydrocortisone to improve cardiac contractility;
- Contrical is used to normalize blood clotting.
Emergency therapy for hemorrhagic shock has been tested for many years and is considered successful with strict adherence to medical prescriptions and dosage of medications. To consolidate therapeutic effects, rehabilitation after treatment is important, which includes gentle exercise therapy.
Replenishment of the bloodstream
In case of significant blood loss, the victim is given an emergency blood transfusion to prevent irreversible consequences. The procedure is performed according to certain rules:
- Blood loss within 25% is replaced with blood substitutes;
- For children under three years of age, the missing volume is compensated with blood with the addition of red blood cells in proportions of 1 to 1;
- For blood loss up to 35% of the bcc, the compensated solution should consist of blood, its substitutes and red blood cells;
- The volume of fluids artificially introduced into the body must exceed blood loss by 20%;
- If the volume of bcc is reduced by half, fluids are administered 2 times more, while the number of red blood cells should also exceed blood substitutes by 2 times.
Emergency measures are stopped when the patient’s condition is stabilized, which manifests itself in the normalization of blood pressure, cardiac activity and diuresis.
What complications are possible with hemorrhagic shock?
The state of hemorrhagic shock is very transient, dangerous due to massive blood loss and death due to cardiac arrest.
- The most severe complication is the development of disseminated intravascular coagulation syndrome. It disrupts the balance of formed elements, vascular permeability, and impairs microcirculation.
- Tissue hypoxia most affects the lungs, brain, and heart. This is manifested by respiratory and heart failure, mental disorders. In the lungs, the formation of a “shock lung” with hemorrhagic areas and necrosis is possible.
- Liver and kidney tissues react with manifestations of organ failure, impaired synthesis of coagulation factors.
- In case of obstetric massive bleeding, long-term consequences are considered to be a violation of a woman’s reproductive capabilities and the appearance of endocrine pathology.
To combat hemorrhagic shock, it is necessary to maintain constant readiness of medical personnel and have a supply of drugs and blood substitutes. The public has to be reminded of the importance of donation and community participation in providing assistance.
Pathogenesis
The main factors in the development of hemorrhagic shock include:
- Severe deficit of blood volume with the development of hypovolemia , which leads to a decrease in cardiac output.
- Decreased oxygen capacity of the blood (oxygen delivery to cells and reverse transport of carbon dioxide decreases. The process of delivery of nutrients and removal of metabolic products also suffers).
- Hemocoagulation disorders that cause disorders in the microvasculature - a sharp deterioration in the rheological properties of blood - increased viscosity (thickening), activation of the blood coagulation system, agglutination of blood cells, etc.
hypoxia occurs , often of a mixed type, capillarotrophic insufficiency, causing dysfunction of organs/tissues and disruption of the body's vital functions. Against the background of disruption of systemic hemodynamics and a decrease in the intensity of biological oxidation in cells, adaptation mechanisms are turned on (activated) aimed at maintaining the vital functions of the body.
Adaptation mechanisms primarily include vasoconstriction (vasoconstriction), which occurs due to activation of the sympathetic part of neuroregulation (release of adrenaline , norepinephrine ) and the action of humoral hormonal factors (glucocorticoids, antidiuretic hormone, ACTT, etc.).
Vasospasm helps to reduce the capacity of the vascular bloodstream and centralize the circulatory process, which is manifested by a decrease in the volumetric velocity of blood flow in the liver, kidneys, intestines and vessels of the lower/upper extremities and creates preconditions for further disruption of the function of these systems and organs. At the same time, the blood supply to the brain, heart, lungs and muscles involved in the act of breathing continues to remain at a sufficient level and is the last thing to be disrupted.
This mechanism, without pronounced activation of other compensation mechanisms in a healthy person, is capable of independently neutralizing the loss of about 10–15% of the bcc.
The development of severe ischemia of a large tissue mass contributes to the accumulation of under-oxidized products in the body, disturbances in the energy supply system and the development of anaerobic metabolism. adaptive response to progressive metabolic acidosis , since they contribute to more complete utilization of oxygen by various tissues.
Relatively slowly developing adaptive reactions include fluid redistribution (its movement into the vascular sectors from the interstitial space). However, this mechanism is realized only in cases of slowly occurring minor bleeding. Less effective adaptive responses include increased heart rate (HR) and tachypnea .
Developing cardiac/respiratory failure is leading in the pathogenesis of acute blood loss. Volumetric bleeding leads to decentralization of the systemic circulation, an extreme decrease in the oxygen capacity of the blood and cardiac output, irreversible metabolic disorders, “shock” organ damage with the development of multiple organ failure and death.
In the pathogenesis of hypovolemic shock, it is necessary to take into account the role of the developing imbalance of electrolytes, in particular, the concentration of sodium ions in the vascular bed and extracellular space. In accordance with their concentration in the blood plasma, isotonic type of dehydration (at normal concentration), hypertonic (increased concentration) and hypotonic (decreased concentration) type of dehydration are distinguished. Moreover, each of these types of dehydration is accompanied by specific shifts in plasma osmolarity, as well as extracellular fluid, which has a significant impact on the nature of hemocirculation, the state of vascular tone and cell functioning. And this is important to consider when choosing treatment regimens.