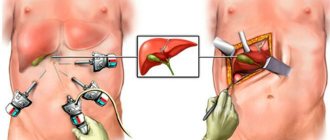
Today, laparoscopy is very popular due to its low degree of penetration (invasiveness). Unlike the traditional abdominal one, where the length of the incision reaches 15-17 cm. With laparoscopy, the length of the main incision does not exceed 3-5 cm; the length of 2-3 incisions for inserting a video camera and manipulators is 1-2 cm.
Despite the shorter rehabilitation period, as after abdominal surgery, after laparoscopy it is necessary to go through the same stages of recovery of the body: diet, taking medications, dosed physical activity.
Since less tissue is damaged, the full recovery cycle occurs 2-3 times faster. Exceptions include complications during surgery and postoperative complications.
Is physical activity allowed after laparoscopy?
In the first 2 weeks, any physical activity is strictly prohibited.
In the first 2 weeks, any physical activity is strictly prohibited. Lifting weights more than 3 kg from 3 weeks. Until the sutures heal, you must not: sharp bends; massage: fast walking; exercises associated with muscle load, regardless of muscle group.
Before a walk, do not drink tonic drinks. Sex - after the discomfort in the abdominal muscles disappears.
If there is redness of the healing sutures, do light breathing exercises, no more than 2 deep inhalations and exhalations. If after removing the stitches on days 3-5 there is a burning sensation or twitching in the muscles - a light walk indoors. Absorbable sutures - 3-5 breaths in a supine position.
If there is a need to lift any object from the floor, lightly kneel down or squat down, stand up slowly, preferably hold on to a support.
For the first 3 weeks, avoid sitting in a bent position. Do not wear high platform shoes or heels.
For the first 1.5 years, do not wear tight belts or clothes.
Lifestyle after gallbladder removal
Be sure to stick to the diet
Be sure to stick to your diet. The first 7 days - puree soups, mashed potatoes, cereals, yogurts, low-fat cottage cheese.
When ventilating the room, do not stay in the room. Overheating and hypothermia - inflammation of the seams is strictly prohibited. Walk slowly for the first month, slowly going up the stairs.
Throughout life.
- Eliminate fried, smoked, alcohol, vinegar as a sauce from the diet; dishes cooked over a fire.
- Minimize onions, garlic, mustard, horseradish, preserves with cloves, red pepper and plenty of vinegar; Replace vinegar with lemon juice.
- Do not lift more than 10 kg, if this happens - bed rest for 24 hours.
- Do not swim in an ice hole in winter.
- Immediately stop any physical activity if shortness of breath occurs.
- Instead of sugar, give preference to honey.
- Do not combine acidic and fatty foods.
- Do not take choleretic drugs without a doctor's prescription.
Watch a video about life without a gallbladder:
After gallbladder removal
Those who have undergone surgery for calculous cholecystitis have many questions. Many people are interested in how to behave after being discharged from the hospital, what the diet should be, and what to do so that the absence of a gallbladder does not negatively affect digestion.
Important changes
In a healthy person, bile enters the gallbladder from the liver, where it accumulates and reaches a certain concentration. As food arrives, concentrated bile from the bladder is secreted into the duodenum and is involved in the digestion and absorption of fats: butter and vegetable oil, fat from meat, fish, sour cream, milk and other products.
After removal of the gallbladder (cholecystectomy), a series of biochemical changes occur, the system of regulation of bile flow is disrupted; the motility of the muscles of the duodenum is impaired. And bile becomes more liquid and worse protects against the invasion of microbes. They do not die, but multiply, upsetting the balance of microflora. Bile acids turn into chemically strong aggressors - irritants of the mucous membrane. The result of these metamorphoses may be
- inflammation of the duodenum (duodenitis) and disruption of its motor activity,
- throwing food masses back into the stomach and esophagus, and as a result - esophagitis, gastritis, enteritis, colitis.
The troubles are complemented by disturbances in the secondary absorption and use of bile due to the absence of a bladder. Bile acids usually make the liver-intestinal-liver turnover 5-6 times a day, and are now excreted and lost by the body. Without them, interruptions in digestion get worse. At this stage, a gastroenterologist or general practitioner will help you choose the right course of drug treatment.
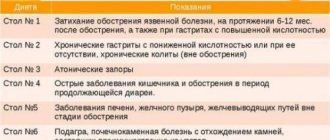
Diet
Less concentrated bile can now act as digestive juice only for small portions of food . If a person does not follow the correct diet, bile stagnation occurs in the liver. There is a danger of developing an inflammatory process in the intrahepatic ducts (cholangitis) and even, although rarely, the formation of stones in them . That is why after the operation the patient is supposed to eat little, but often (6-7 times a day). After all, every meal is a kind of push that promotes the active release of bile into the duodenum.
In the first three to four months after surgery, the body gradually adapts to the new digestive conditions.
- During this period, a gentle diet : only boiled and pureed dishes.
- Then the diet is gradually expanded to include unprocessed meat and fish, raw fruits and vegetables.
- You need to chew longer - the slow flow of food into the stomach allows you to wake up the enzymes, giving the liver time to start working.
Nutrition should be complete:
- Sufficient amount of proteins : meat, fish, cheese, cottage cheese.
- Carbohydrates : white bread, cereals, fruits and vegetables.
- Vitamins and mineral salts are needed , which mostly come from food, but sometimes the doctor prescribes pharmaceutical preparations of vitamins to the patient.
- Foods that contain large amounts of cholesterol are not recommended: it promotes the formation of stones.
- Limit fats , completely exclude indigestible ones - pork, beef, lamb. At first, no more than 20 grams of butter per day is allowed, and no more than 40 grams of vegetable oil. Then, when the doctor allows you to expand the diet, the amount of fat can be increased to the norm of 80-100 grams. We should not forget that fats are found in many foods. It must be borne in mind that refractory fats, and even easily digestible ones, consumed in excess, suppress liver function.
- Pickles, smoked meats, marinades, and alcoholic beverages are also excluded.
- It is better to replace sweets with berries, honey and dried fruits.
- But the fermented milk assortment with live bifidobacteria (bifidok, bifidokefir) helps improve intestinal microflora and neutralize cholesterol. You will also need prebiotics - preparations with dietary fiber - food for beneficial microflora.
Water
Frequent drinking of water is necessary . Before meals, every 2.5-3 hours you should drink about a glass (200-250 ml) of water, based on the dosage: 1 sip (30 ml) per 1 kg of body weight. This is a necessary condition for protecting the mucous membrane of the gastrointestinal tract (GIT) and duodenum from the aggression of bile acids.
You should not consume more than 1.7-2 liters of liquid, including soups, compotes, and jelly. Check to see if all the liquid you drink during the day is released. To do this, you need to know how much you drank and how much urine was released.
It happens that due to a change in the motility of the duodenum, bile is thrown back into the stomach and further into the esophagus. In addition to the unpleasant feeling of bitterness in the mouth, the “counterflow” of bile damages the mucous membrane of the esophagus. Therefore, drinking water to neutralize the harmful effects of bile and normalize the functioning of the gastrointestinal tract is especially important. For any dyspeptic disorders (rumbling, bloating, diarrhea, constipation), do not rush to swallow the pill, but drink a glass of clean water .
It is useful to drink those drinks that have a choleretic effect : rosehip decoction, barberry decoction, fruit and vegetable, especially tomato, juices, compotes from dried apples, prunes, dried apricots.
Mineral waters help to liquefy bile and prevent its stagnation : Essentuki No. 4, 20, Slavyanovskaya, Smirnovskaya, Naftusya and others. However, gallstone disease is often accompanied by gastritis and pancreatitis. Therefore, your doctor will tell you what kind of mineral water, when and how much to drink.
Mineral water is usually prescribed, half a glass warm, 30-40 minutes before meals, but no more than three times a day. Pour water into an enamel mug and place it in a pan of boiling water for 3-5 minutes, removed from the heat. Drink heated water slowly, in small sips. Mineral waters are usually used in courses. After a month of daily use, it is recommended to take a break for two to three months, and then repeat the course of treatment again within a month.
Exercise stress
To avoid stagnation of bile, movement is necessary. One to two months after the operation (depending on the patient’s well-being), swimming will be useful as a means of gentle massage of the abdominal cavity. In addition, daily walks for 30-40 minutes in the fresh air are a muscle load that helps fight bile stagnation and improve oxygen saturation of body tissues. And if there is no oxygen deficiency, it means that metabolism will be intense, and liver activity will be normalized, in particular the process of bile secretion.
A few days after the start of daily walks, you should begin morning hygienic exercises. Physical exercise activates the function of the abdominal organs, including the liver, thereby facilitating the discharge of bile.
Skiing at a leisurely pace is not only allowed, but recommended. Your doctor will tell you when to start these walks. Of course, there is no question of any sports competitions or participation in cross-country races, since overload is dangerous. Dosed physical activity is necessary.
For 6-12 months after surgery, heavy physical activity , especially those associated with tension in the abdominal muscles, is not allowed. This can cause the formation of an incisional hernia. For obese people whose abdominal muscles are weakened, doctors recommend wearing a special bandage . It is put on in the morning without getting out of bed and removed at night. The duration of wearing the bandage is largely determined by the person’s well-being and the course of the postoperative period.
A set of exercises after cholecystectomy
These exercises are not burdensome and bring undoubted benefits. You can expand this complex and do exercises in which the abdominal muscles intensively contract (bending over, lifting your legs and body from a lying position) no earlier than six months after the operation, if your health is quite satisfactory.
It is recommended to start classes with calm walking for one and a half to two minutes; breathing is voluntary. Then perform exercises in a standing and lying position.
- Standing, feet shoulder-width apart. Turn the body to the right and left while simultaneously raising your arms to the sides - inhale. Lower your hands - exhale. Repeat 4-6 times.
- Standing, feet shoulder-width apart, hands on your belt. Pull your elbows back - inhale, return to the starting position - exhale. Repeat 6-8 times.
- Lying on your back, legs extended, arms along the body. Bend your leg, bringing it as close as possible to your stomach - exhale, straighten your leg - inhale. Do the same with the other leg. Repeat 4-6 times.
- Lying on your back, legs bent, right hand on your stomach, left along your torso. While inhaling, stick your stomach out, and while exhaling, pull it in strongly. Repeat 4-6 times.
- Lying on your back, legs straight, hands on your belt. Raise and move your straight leg to the side - exhale, lower - inhale. Same with the other leg. Repeat 4-6 times.
- Lying on your back, legs bent, arms along your body. Sliding your heels along the floor, stretch your legs - inhale, bend them just as slowly - exhale. Repeat 4-6 times.
- Lying on your side, legs straight. One hand is on the belt, the other is behind the head. Bend the leg lying on top - exhale, straighten - inhale. Do the same with the other leg, turning to the other side. Repeat 4-6 times.
- Lying on your side, legs bent. While inhaling, stick your stomach out, and while exhaling, pull it in strongly. Repeat 6-8 times.
- Standing, feet shoulder-width apart, hands to shoulders. Circular movements with your elbows 8-10 times forward and back. Breathing is voluntary.
Spa treatment
Spa treatment is necessary mainly for those who have had complicated calculous cholecystitis, as well as in the presence of concomitant diseases of the digestive system. Drinking resorts are recommended, which one will be advised by the attending physician. Usually you are allowed to travel no earlier than six months after the operation.
Sea bathing is not contraindicated: swimming is even beneficial, as the water has a kind of massaging effect. You can go to the sea and swim six months to a year after surgery.
We are about health
Stages of rehabilitation
The rehabilitation process begins immediately after the end of general anesthesia - 30-75 minutes after completion of the operation (cessation of infusion), regardless of the type.
The first stage is quenching strong thirst. Do not give anything to drink until 3 hours after waking up! Moisten lips with a cotton or gauze swab soaked in boiled water. No more than 5 ml should enter the mouth.
Give drinks on demand, preferably once every 10-15 minutes. After 3 hours, no more than 50 ml every half hour. Regular drinking regimen after 12 hours, if there is no nausea.
The second stage is a post-operative diet of puree soups, liquid porridges for up to 3 days.
Get up slowly for up to 7 days.
Mineral water is not carbonated. Leave the carbonated one for 24 hours for the gas to escape.
During the week, drain the first broths.
The first 3 days, for prophylactic purposes, an antibiotic 2 times a day. Optimal 1 of the cephalosporins; for contraindications - synthetic penicillin; if not, natural. Painkillers administered intramuscularly only when necessary - slow down healing, high load on the liver.
Relieve nausea with cerucal, metoclopramide; mint dries out the mucous membranes.
Important! These stages, in addition to quenching thirst, are performed as needed, and not one by one.
Physical exercise
Baths and saunas no earlier than six months after surgery
There are no clearly defined periods for playing sports or performing heavy physical exercises.
Playing sports no earlier than 3 months, and swimming - 1.5 months. Weightlifting no earlier than 5 months. Light – 4-5 months. Sprint 9-12 months.
Contrast showers, baths and saunas no earlier than six months. This also applies to immediate air temperature changes of more than 15 degrees.
After the stitches have completely healed, you can go to the swimming pool. The rabbit is no earlier than six months old. Butterfly after 9 months. Start from a distance of 25 m with a surface breaststroke. A week after healing until mild tingling occurs.
Further, water procedures depend on the condition of the body. If one or another procedure (swimming) results in heartburn, bitter belching for more than 24 hours, or discomfort in the right hypochondrium, resume after a 2-week break after consulting a doctor.
Operation duration
The duration of laparoscopic cholecystectomy surgery depends on the complexity of the operation and the experience of the surgeon. Laparoscopic cholecystectomy lasts on average from 40 to 1.5 minutes, but in complex cases up to 3 to 5 hours.
Indications for laparoscopic gallbladder removal
Laparoscopic removal of the gallbladder is performed if the following indications exist:
- chronic calculous cholecystitis;
- gallbladder polyps;
- asymptomatic cholecystolithiasis (presence of gallstones that do not bother the patient) if they are less than one centimeter;
- acute cholecystitis (no later than two or three days from the onset of the disease).
Physiotherapy
Exercise therapy exercises only after the permission of the attending physician. The complex is prescribed individually.
The most common:
| Squats | Start with 3-5 – increase to 10-15 repetitions; add 1 per day; do once a day in the morning. |
| Bends forward, backward, sideways | Start with 1-3 - increase to 10-15, do it once, and after 2 weeks, 2 times a day. |
| Circular rotation of the shoulders in different directions, in a sitting position | Start with 10, then until you feel discomfort in the muscles, right hypochondrium. |
| Lifting the pelvis while lying down | Start with a slight lifting from the surface by 1-2 cm with a delay in the upper position for 3-5 seconds, 3-5 repetitions; bring to a tear of 3-5 cm with a 15-second delay; do 2-3 times a day. |
| Bend forward, reaching your toes with your fingertips | Start with 5-10 – increase to 20-30 repetitions; do it once a day. |
| "Bike" | Starting position, lying on your back, make circular rotations with your legs, imitating riding a bicycle; start with 3-5 – increase to 15-20 repetitions; start performing 3-5 days after the stitches have healed. |
Important! The starting position for all exercises performed standing is with your feet shoulder-width apart. Movements should be smooth. If you feel slightly tired, stop. Do not do gymnastics on an empty stomach or empty stomach. Do the exercises no earlier than 1.5-2 hours after waking up.
Therapeutic exercises after laparoscopy
Breathing exercises
Start performing on the 5th day:
- Position lying on your back; slow breath; hold your breath for 1-3 seconds; exhale very slowly – 1-3 repetitions.
- Short inhalations and exhalations: start from day 5-7 for 30-60 seconds – increase to 2-3 minutes.
- Position, standing; when inhaling, rise on your toes, raise your arms up, stretch your whole body up; exhale – starting position; inhale – 15-30 – exhale 10-15 seconds; start on the 10th day after surgery.
Attention! Stop breathing exercises at the slightest dizziness.
Physical therapy after gall bladder surgery: development of diaphragmatic breathing
One of the most serious problems 1-2 days after gall bladder surgery is the risk of developing congestion in the lungs. This is due both to the volume of surgery and to the presence and location of drains in the abdominal cavity. Concomitant pathology – obesity – is also important. Under such conditions, there is a sharp restriction in the mobility of the diaphragm, tidal volume decreases, and breathing mechanics are disrupted.
Physical therapy after gall bladder surgery solves this problem through special exercises aimed at preventing congestion in the lungs.
Hiking
The first walks should not last more than 30 minutes. Thirst will arise. Bring still or boiled mineral water with you. Boil water for at least 30 minutes. Drain the top third.
Wear linen T-shirts under warm clothes. Move slowly. If you have a bandage, sit down after 10 minutes. There should be no burden. The step is measured.
Dizziness, burning sensation in the operated area - reduce walks to 15-20 minutes. Don't go far from home. Once a month, go to the coniferous forest. Walk on flat ground. Avoid excessive sweating in the operated area.
Spa treatment
To speed up recovery, therapy with mineral waters is prescribed in sanatoriums
To accelerate the restructuring of the digestive secretion organs to new conditions, mineral water therapy is prescribed. Recommended: Borjomi, Essentuki 17, Naftusya. Medicinal mineral waters retain their healing properties for no longer than 6 hours after they are received from the source.
Naftusya – up to 15 minutes. For this therapy to be highly effective, it is necessary to undergo treatment in sanatoriums focused on the treatment of liver and gallbladder diseases. In these centers, the diet is based on diet No. 5 or No. 5a: Kislovodsk, Essentuki, Morshin, Truskavets.
Advantages of laparoscopic surgery over laparotomy (incision in the abdominal wall)
Without a doubt, the laparoscopic method of gallbladder removal has a number of advantages over laparotomy:
- for the operation, not an incision is used, but four punctures, anterior abdominal;
- pain after surgery subsides within one day;
- at the end of the operation, the patient can walk independently and perform simple actions;
- length of hospital stay is reduced (from 1 to 4 days);
- rehabilitation and restoration of working capacity occur quickly;
- the risk of postoperative hernia formation is reduced to a minimum;
- The scars are either barely noticeable or cannot be seen at all with the naked eye.
Possible consequences
Bloating and flatulence may be symptoms of complications after surgery
The main complication is postcholecystectomy syndrome - digestive disorders due to uneven redistribution of the load between the organs that secrete secretions in the gastrointestinal tract - the stomach, pancreas, liver, as well as the microflora of the large intestine.
The syndrome may appear 4-7 years after surgery. The type of surgery does not matter. With the development of the syndrome: constant heartburn, flatulence, dysbacteriosis, dyspepsia.
Other complications.
- Suppuration in the operated area with possible blood sepsis.
- Immune diseases.
- Autoimmune manifestations - allergies, inflammatory diseases throughout the body.
What do experts recommend?
- After removal of the gallbladder, permanently exclude beer and pork fat from the diet, regardless of heat treatment; meat, fish, eggs that have undergone improper heat treatment; give preference to plant foods - carrots and beets daily.
- Avoid hunger – satisfy hunger even at night; meals are fractional.
- Gradually accustom the body to physical activity - this also applies to athletes.
- Any medications only as prescribed by a doctor; folk remedies - only pharmacy preparations or a prescription drawn up by the attending physician.
- Take general and biochemical blood tests, and do an ultrasound of the abdominal cavity 2 times a year.
- Do not sunbathe for more than 2 hours a day; Avoid midday sunlight.
Long Range Exercises
At this time, gymnastics is aimed at:
- restoration of full functionality;
- adaptation of the cardiovascular and respiratory systems to normal levels of physical activity.
Such physical education is also recommended after discharge from the hospital. The essence of the exercises is the same. Like in the late period. Only the frequency of repetitions and the weight of the weights used increase. Sports games and skiing are also useful at this rehabilitation stage.
Long range exercise – skiing