The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
Unfortunately, pregnancy can be accompanied by abdominal pain, which is associated not only with enlargement and hypertonicity of the uterus. Sometimes its course is complicated by various diseases of the abdominal organs. One of the most insidious among them is acute appendicitis.
In pregnant women, appendicitis occurs a little differently, masquerading as any other condition and an enlarged uterus. And the risk of severe complications doubles, because we are talking about mother and child. Therefore, it is so important to correctly and carefully evaluate all the data that speaks in favor of acute appendicitis during pregnancy.
Causes
It is noted that such a combination as appendicitis and pregnancy occurs somewhat more often than the same disease in non-pregnant women. What is this connected with? It is difficult to say, since the causes of the development of the disease have not yet been precisely established. The most common theory states that inflammation of the appendix is associated with blockage of the passage between the appendix and the cecum.
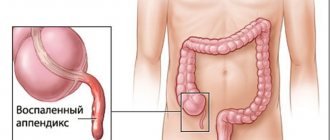
For example, blockage can occur due to the formation of coprolites - small fecal stones. As a result, blood circulation in the appendix worsens and inflammation begins. Accordingly, during pregnancy, another risk factor is added: the enlarging uterus displaces and puts pressure on almost all abdominal organs, including the appendix. The result may be a disruption of the blood supply and conditions for impaired evacuation of the contents of the appendix.
What to do?
If a pregnant woman has a stomach ache, she must see a doctor in any case. She must be examined by two specialized specialists: an obstetrician-gynecologist and a surgeon. In all doubtful cases, hospitalization in a surgical or obstetrician-gynecological hospital is indicated. Pregnant women with suspected appendicitis are monitored for 12 hours. During this time, the necessary diagnostic studies are carried out and the issue of further tactics is decided. Under no circumstances should you administer or take painkillers yourself. They can further confuse the clinical picture. It is only advisable to use antispasmodics (no-spa, papaverine, riabal), both for the purpose of pain relief and for differential diagnosis with various colic and uterine hypertonicity.
Stages of the disease
The main danger of this disease is its rapid development. It takes only 2 days for the development from a mild stage to complete destruction of the appendix. There are four stages of the disease:
- catarrhal, when only the mucous membrane of the organ is affected;
- phlegmonous, when the lesion reaches the internal mucous layers and also partially affects the muscle layers;
- gangrenous, when we are talking about the death (necrosis) of all layers of the organ;
- In case of a long absence of medical care, perforation of the organ (destruction of the wall of the appendix) may occur, due to which the contents of the appendix enter the abdominal cavity.
Signs of the disease
Every woman should know the signs of appendicitis during pregnancy, and if they are detected, consult a doctor as soon as possible. The situation is complicated by the fact that against the background of an “interesting” situation, the signs may not be expressed clearly enough.
In addition, the woman’s sensations will directly depend on the duration of pregnancy, the degree of damage to the organ and its location in the abdominal cavity. The growing uterus inevitably displaces the appendix from its usual place - the right iliac region. As a rule, in the initial stage, appendicitis during pregnancy has the following manifestations: pain in the upper abdomen with a gradual shift to the right iliac region. Nausea and vomiting are also characteristic of this condition. Most likely, the pain will intensify when lying on the right side.
Let's say you suspect you have appendicitis during pregnancy, what should you do? You should call an ambulance immediately!
Appendicitis during pregnancy
Appendicitis
is an inflammation of the appendix of the cecum. In pregnant women, this disease occurs with a frequency of 1 case in 800-2000 pregnant women. With increasing gestational age, the frequency and severity of complications from appendicitis increases, which is due to diagnostic difficulties, inadequate patient management and delayed surgical treatment.
Most often, in 63% of cases, catarrhal appendicitis occurs during pregnancy, which is a simple form of this pathology. More complicated, destructive forms, such as phlegmonous, gangrenous, perforated appendicitis, occur during pregnancy with a frequency of up to 37% of cases. In most cases, acute appendicitis occurs in the first half of pregnancy, and about 25% of cases occur in the second half. Complicated destructive forms mainly occur in the third trimester of pregnancy and after childbirth. These forms of the disease are often accompanied by perforation of the appendix with the development of diffuse peritonitis.
The main prerequisite for the development of appendicitis during pregnancy is the displacement of the cecum along with the appendix upward and outward due to the enlargement of the pregnant uterus. In this case, the vermiform appendix is bent, stretched, blood supply deteriorates, and emptying is impaired. The tendency to constipation, which often occurs during pregnancy, contributes to stagnation of intestinal contents and increased activity of intestinal microflora. Adhesions form with the uterus, which leads to increased contractile activity, and in some cases, in 2.7-3.2% of women, to termination of pregnancy. With destructive appendicitis, fetal death can also occur.
Childbirth with appendicitis can be complicated by abnormal contractile activity of the uterus, fetal hypoxia, bleeding in the afterbirth and early postpartum period. Child losses due to acute appendicitis in the second half of pregnancy occur 5 times more often than in the presence of this disease in the first half of pregnancy. The incidence of fetal death due to perforation of the appendix reaches 28%, and in the case of peritonitis it reaches up to 90%.
Clinical course and diagnosis of acute appendicitis during pregnancy
During pregnancy, the body's defenses are weakened in a certain way. In this regard, the clinical picture of acute appendicitis may be blurred, and typical symptoms of the disease may appear only with a widespread process. It should be noted that often the clinical picture of acute appendicitis in the first half of pregnancy is practically no different from that in non-pregnant women. In the second half of pregnancy, the nature of the course of the disease largely depends on the changes that have occurred in the appendix and its location.
Abdominal pain with appendicitis may not be as severe as in non-pregnant women. In this regard, the presence and severity of the disease should be judged by such signs as an increase in pulse rate, rise in body temperature, vomiting, bloating, shortness of breath, and difficulty breathing. The presence of abdominal pain during childbirth can be masked by contractions, and after childbirth - by pain associated with inflammatory diseases of the uterus and its appendages.
The further prognosis for the mother and fetus depends on the quality and timeliness of diagnosis of acute appendicitis in pregnant women. Women more often associate the presence of abdominal pain with the threat of miscarriage and often engage in unsuccessful self-medication for the complication they suspect. This leads to late consultation with a doctor, delayed hospitalization, aggravation and complicated course of acute appendicitis and late surgery. Most pregnant women with acute appendicitis are admitted to the maternity hospital with a false diagnosis of threatened miscarriage. The correct diagnosis before hospitalization is made in no more than 1/3 of observations.
With a typical picture of acute appendicitis in the first half of pregnancy, difficulties in diagnosing this disease, as a rule, do not arise. Exceptions may be cases of atypical location of the appendix. In the second half of pregnancy, symptoms of peritoneal irritation are poorly expressed or absent due to stretching of the anterior abdominal wall and the lack of direct contact of the appendix with the peritoneum, as this is prevented by the enlarged pregnant uterus. Starting from the second half of pregnancy after 20 weeks, the enlarged uterus displaces the cecum with the vermiform appendix upward and posteriorly. Toward the end of pregnancy, the appendage may be located closer to the right kidney and gallbladder, which changes the typical location of pain. As a result, pain can be detected not in the lower abdomen on the right, but higher in the right hypochondrium.
Comparison of the number of leukocytes and pulse rate acquires important diagnostic significance in pregnant women. Thus, with a pulse rate of more than 100 beats/min in combination with an increase in leukocytes of more than 12-14 X 109/l, even at normal body temperature, the presence of a destructive process can be assumed with a high degree of probability. During childbirth, the tension of the muscles of the anterior abdominal wall is weak due to its stretching. Therefore, for diagnosis, it is important to pay attention to the local nature of abdominal pain, the appearance of signs of intoxication, as well as the results of a clinical blood test. An increase in temperature may indicate that a destructive process has already begun. To diagnose the disease, laparoscopy can be used, which makes it possible to correctly diagnose 93% of pregnant women with appendicitis, which in turn helps reduce the incidence of complications and prevent unnecessary surgical interventions in 84% of patients. Ultrasound examination is not very informative from the point of view of diagnosing acute appendicitis in pregnant women.
Depending on the location of the appendix, the resulting inflammatory process leads to damage to other adjacent organs of the abdominal cavity, which is manifested by the clinical picture of pyelonephritis, spontaneous abortion, premature birth, premature abruption of a normally located placenta, intestinal obstruction, etc. It is also important to distinguish acute appendicitis from other possible complications of pregnancy, which may have similar symptoms and a similar clinical picture. Such complications and diseases include: early toxicosis, renal colic, pyelonephritis, cholecystitis, pancreatitis, ectopic pregnancy, pneumonia and torsion of the ovarian cyst.
In the second half of pregnancy, when the appendix is located high, appendicitis can be difficult to distinguish from right-sided pyelonephritis or cholecystitis. In this case, attention should be paid to the onset of diseases. Thus, acute appendicitis always begins with pain, then the temperature rises and vomiting appears. Pyelonephritis, on the contrary, more often begins with chills, vomiting, fever, and only later does pain appear in the lumbar region. In addition, leukocytes and red blood cells appear in the urine in significant quantities.
Differential diagnosis with acute cholecystitis is very difficult, and often a correct diagnosis is only possible with laparoscopy. In postpartum women, a positive Shchetkin-Blumberg symptom may be associated with inflammation of the uterus and its appendages.
In the process of differential diagnosis, the sensations of tapping in the lumbar region are assessed - Pasternatsky's symptom, which should be negative in case of appendicitis. Urine is also examined, which should not contain pathological elements. Before 12-13 weeks of pregnancy, a vaginal examination should be performed. For differential diagnosis with renal colic, it is advisable to perform chromocystoscopy. Moreover, in the case of renal colic, the injected dye is not released from the ureter with impaired patency. To exclude torsion of the ovarian cyst stalk, an ultrasound examination is performed. In particularly difficult cases, laparoscopy is performed to clarify the diagnosis.
It is also necessary to remember that a combination of acute appendicitis with other complications and diseases is possible.
Treatment of acute appendicitis
Acute appendicitis, regardless of the duration of pregnancy, can only be treated surgically, since against the backdrop of a weakening of the body's defenses, the likelihood of a destructive process with all its negative consequences increases significantly. It is advisable to transfer a pregnant woman to the surgical department for appendectomy and postoperative management.
In the first half of pregnancy, the surgical technique does not differ from that outside pregnancy. The wound is sutured tightly. In the second half of pregnancy, the anterior abdominal wall is dissected higher than usual. If access to the appendix is difficult due to an enlarged uterus, the patient should be turned on the left side. The method of choice is lower-median laparotomy. In the first half of pregnancy, with uncomplicated appendicitis, appendectomy can be performed using laparoscopy.
In case of complications (peritonitis, infiltrate, abscess), drainage of the abdominal cavity is performed with the administration of antibiotics. The subsequent volume of treatment depends on the extent of the process.
Appendiceal infiltrate
treated conservatively until it resolves or abscesses. If the infiltrate resolves, appendectomy is performed after 6 months. If it develops an abscess, surgery is also necessary. If an abscess ruptures, the operation is performed as an emergency. In the postoperative period, the administration of drugs that increase uterine contractility should be avoided. In this regard, prozerin, hypertonic sodium chloride solution and hypertonic enemas are not used. Spontaneous miscarriage after surgical treatment of appendicitis occurs in 0.9-3.8% of women. To prevent this complication in women after surgery performed in the first trimester, magnesium preparations and vitamin E are prescribed. In later stages of pregnancy, the development of premature birth soon after surgical treatment of appendicitis is extremely undesirable, since contractions of the uterus and changes in its size and configuration after childbirth disrupt healing process and contribute to the spread of peritonitis. To prevent premature development of labor, ginipral or partusisten is prescribed after surgery in the second and third trimesters of pregnancy. To prevent postoperative inflammatory complications, patients are prescribed antibiotics. As part of the management and treatment of a pregnant woman with appendicitis, the tactics of maximizing pregnancy preservation are followed, regardless of the form of appendicitis.
With diffuse purulent peritonitis
due to phlegmonous or gangrenous appendicitis, a cesarean section is performed. After this, the appendix is removed, the abdominal cavity is drained, and all measures aimed at treating peritonitis are carried out. With a short period of pregnancy, it is possible to treat peritonitis while prolonging pregnancy. At the request of the woman, an artificial abortion is also performed. At the same time, it is performed 2-3 weeks after surgery if the postoperative period is uncomplicated. If the pregnancy is full-term or almost full-term, then a cesarean section is first performed, and after suturing the incision on the uterus, an appendectomy is performed, followed by treatment of peritonitis.
In the presence of catarrhal or phlegmonous appendicitis
against the background of the normal course of labor, it should be completed as quickly as possible through the vaginal canal, and then an appendectomy should be performed. During childbirth, complete pain relief and prevention of fetal hypoxia are carried out.
In the case of a normal course of labor and the occurrence of a clinical picture of gangrenous or perforated appendicitis, it is necessary to simultaneously perform a cesarean section and subsequent appendectomy.
If the patient has chronic appendicitis
, then the greatest likelihood of its exacerbation occurs in the third trimester of pregnancy. The appendix is removed as planned. When a chronic process becomes acute, emergency surgery is necessary.
Make an appointment with specialists by calling a single call center:
+7(495)636-29-46 (metro stations “Schukinskaya” and “Street 1905 Goda”). You can also make an appointment with a doctor on our website, we will call you back!
Diagnostic issues
Diagnosing appendicitis during pregnancy is quite difficult. There are not many reliable research methods. The examination always begins with palpation, which allows the localization of pain to be established.
Then a blood test is done for leukocytes and ESR. The presence of an inflammatory process is always expressed by an increase in leukocytes. However, this is how absolutely any inflammation is expressed, so this analysis does not give a clear answer. The same applies to urine tests. The fact is that the result of this analysis may be affected by pathological changes in the kidneys or bladder.
An ultrasound can give more or less accurate results, provided that the appendix can be seen. However, more than half of women fail to do this. There is only one method left - laparoscopy. In this case, a puncture is made in the abdominal wall and a laparoscope is inserted into the abdominal cavity - a thin, 3 to 5 mm in diameter, instrument with an optical system that is connected to a video camera. It allows you to examine any organ in detail; if necessary, instruments are inserted into the abdominal cavity through the same punctures to perform the operation.
Dangerous consequences of refusing surgery
The stages of development of the inflammatory process take their course and it is not yet possible to stop this mechanism even with strong antibiotics. And if a woman is determined to continue her pregnancy and give birth to a healthy baby, most medications are undesirable.
The clinical course of the disease has a period of subsiding of symptoms and imaginary improvement of the condition. The reduction in pain is caused not by recovery, but by necrosis of the nerve endings of the process. Next, gangrene and the breakthrough of pus into the abdominal cavity quickly progresses.
Dangerous consequences for the child and mother include the development of complications:
- peritonitis;
- multiple abscesses;
- purulent inflammation of the portal vein (pylephlebitis).
In fact, harmful bacteria appear in the blood of the mother’s body, which leads to infection of the fetus. Fetal mortality statistics indicate a connection with a form of inflammation of the appendix in the mother.
| Forms of appendicitis in a pregnant woman | Percentage of fetal death |
| uncomplicated appendicitis | 2–16 |
| perforated appendicitis | 20–50 |
| peritonitis | up to 90 |
The overall incidence of death of an unborn child is 5–7%. The progression of the severity of the inflammatory process increases the risk of death of the child. In the second half of the term it is 5 times higher than in the first.
It has been established that pregnant women tend to deceive themselves and do not immediately seek help. In 25% of cases, they are admitted to surgery two days after the onset of the disease. This period is almost 2.5 times higher than in non-pregnant patients. Therefore, the gangrenous form of appendicitis in late pregnant women is detected 6 times more often than in other women, and the perforated form is detected 5 times more often.
Treatment
Surgical removal of the inflamed organ during pregnancy is the only possible treatment method. This is done either through an incision or, which is much better, by laparoscopy. The advantages of this operation are less pain, less recovery time, and from a cosmetic point of view, three small punctures create much smaller scars than a large incision.
Qualified removal of appendicitis during pregnancy is one of the. Experienced specialists will advise on any questions.