Intercostal neuralgia is a pain syndrome in the intercostal spaces caused by a pathological condition of the peripheral nerves. Due to the location and nature of the pain, it can be confused with a heart attack, and therefore often leads patients into a state of panic. Intercostal neuralgia occurs in approximately 10% of the adult population.
MedEx offers to make an appointment with a neurologist. If necessary, the clinic can carry out all necessary diagnostic procedures and laboratory tests.
Causes
The causes of intercostal neuralgia may be associated with inflammation of the peripheral nerves. As a rule, it develops as a result of hypothermia or an infectious process of another localization. For example, intercostal neuralgia often occurs as a result of herpetic infection or herpes zoster.
Intercostal neuralgia develops as a result of degenerative changes in the thoracic spine. Diseases that lead to the destruction and reduction of the height of the intervertebral discs provoke compression of the nerves. Bone growths form on the vertebrae, which also irritate the nerves.
Other possible reasons include:
- Physical overexertion. Staying in an uncomfortable position for a long time, sleeping on a hard or too soft mattress, intense exercise, as well as chronic vertebrogenic syndrome can lead to compression of the nerves.
- Injuries. Nerve damage can be caused by broken ribs, bruises, and injuries to the chest and spine.
- Cardiovascular diseases. A number of pathologies lead to hypoxia of the nerve trunks - atherosclerosis, arterial hypertension, rheumatism and anemia.
- Endocrine disorders. Intercostal neuralgia is often diagnosed in women during menopause, patients with thyrotoxicosis, diseases of the adrenal glands, and also after long-term use of hormonal drugs.
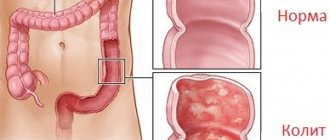
This is not a complete list of diseases and pathological conditions that are accompanied by intercostal neuralgia. The risks of developing the syndrome increase with gastric and duodenal ulcers, diabetes mellitus, tumor diseases, gastritis and colitis.
What is intercostal neuralgia?
Let's start with the fact that intercostal neuralgia is not a disease.
This is the name for pain that occurs when the intercostal nerves are exposed to various pathological factors, for example, herpetic infection, tumors, injuries, disc herniation, protrusion, osteochondrosis, etc. In other words, thoracic intercostal neuralgia can be called not all chest pain, but only that where intercostal nerves are involved. And this needs to be clearly understood so that the confusion that you often encounter at the everyday level does not arise when you hear people using the term intercostal neuralgia, but at the same time they mean a completely different pathology. By the way, even some doctors sometimes make the diagnosis of intercostal neuralgia erroneously, while in reality it most often turns out to be myofascial syndrome. Intercostal neuralgia, myalgia, myositis, myofascial syndrome, osteochondrosis, disc herniation, protrusion and many other terms are not synonymous. These are the names of specific pathologies that have their own characteristics and differences. And, since they are different, it means that the approach to them must also be different, otherwise there will be no sense in the treatment.
In general, the term intercostal neuralgia should not be used haphazardly, and it is not worth calling all pain in this area that way.
Symptoms
The main symptom of intercostal neuralgia is acute unilateral piercing pain localized in the chest. It is gradually growing. Pain with intercostal neuralgia spreads from the spine to the midline of the abdomen or sternum, becoming encircling in nature.
The pain will increase if:
- cough;
- laugh;
- sneeze;
- take a deep breath;
- start moving quickly.
If certain muscle groups are overstrained, the pain may intensify if you lean forward.
Palpation of the affected area with intercostal neuralgia in adults is painful, since the sensitivity of the nerve fibers is increased. There may be a burning sensation or numbness along the nerves.
Acute intercostal neuralgia is manifested by redness or blanching of the skin, hyperhidrosis due to damage to the sympathetic fibers of the peripheral nerves. Depending on which area is affected, the pain can spread to the right or left, affecting the area under the shoulder blades on the back.
Diagnosis of intercostal neuralgia
Diagnosis of intercostal neuralgia is quite difficult, since it must be differentiated from a number of diseases that have similar symptoms. A cardiologist or pulmonologist may be involved in the diagnostic process. Specialists at the CELT Pain Clinic conduct an examination and collect anamnesis, and also determine the presence or absence of the disease in the following ways:
- chest x-ray;
- CT scan;
- myelography;
- Magnetic resonance imaging;
- spondylography;
- electro- and echocardiography;
- examination of the gastrointestinal tract.
If diagnostic studies do not reveal diseases of the lungs, gastrointestinal tract and cardiovascular system, the patient is referred to a neurologist who develops a treatment plan.
Expert opinion of a doctor
Intercostal neuralgia on the left side of the heart is often mistaken by patients for a heart attack. It can be distinguished by its characteristic features. If you take a stationary position during intercostal neuralgia, the symptoms will become less pronounced. For cardiovascular diseases - no.
Pain with intercostal neuralgia intensifies due to coughing, laughter, deep breaths, and forced movements. However, it does not change during cardio exercise. With cardiovascular diseases, it's exactly the opposite.
With neuralgia, heart rate and blood pressure do not change, the pain is girdling in nature and intensifies with palpation of the ribs. In cardiovascular diseases, blood pressure and heart rate change, palpation is painless, and the pain syndrome is localized in the projection of the heart or behind the sternum.
Diagnostics
Diagnosis of intercostal neuralgia begins with an initial examination. First of all, the doctor pays attention to the position of the patient’s body. As a rule, it is tilted to the opposite side - so as not to provoke a second attack. If several nerve branches are affected, sensitivity in a certain area may be impaired.
To clarify the diagnosis, additional studies and procedures may be required:
- ECG;
- X-rays of light;
- MRI of the spine;
- Ultrasound of the abdominal organs;
- electroneurography.
Additional research is needed to differentiate intercostal neuralgia from cardiovascular diseases, infections, diseases of the musculoskeletal system and digestive tract. In this regard, you may need additional consultation with a specialized specialist - a cardiologist, gastroenterologist, chiropractor.
Research is also carried out to clarify the nature and location of the disease. Thus, electroneurography helps determine the structure and functionality of nerve fibers and determine the causes of their irritation.
Important! The information is posted on the website for informational purposes. Don't self-diagnose - consult a specialist!
Intercostal neuralgia: symptoms, diagnosis and treatment
Chest pain is always alarming. As a rule, the first thing a person thinks about is the heart. Statistics, widely revealed thanks to the media, also echo such fears: deaths from cardiovascular diseases confidently remain at the top of the sad list.
However, it is not only the heart that can hurt in the chest. Natalya Vladimirovna Umerenkova, a neurologist and leading specialist in the neurology department at the Expert Clinic Kursk, told us about intercostal neuralgia, one of the symptoms of which is chest pain.
— Unexpected chest pain is always alarming. What can hurt your chest?
Such pain is a signal for both the doctor and the patient. Many anatomical structures can hurt in this area. This is the heart in case of ischemic disease (angina pectoris, heart attack), large vessels (in case of dissecting aortic aneurysm). Pain occurs with tracheitis, pneumonia, accumulation of air in the pleural cavity (pneumothorax) and its inflammation, tumors of the lungs and mediastinal organs, pulmonary embolism, mediastinitis, pathology of the esophagus (inflammation, peptic ulcer).
You can read about the symptoms, diagnosis and treatment of pneumonia here
Pain can also be “reflected” into the chest when the pancreas, gall bladder, or stomach pathology are affected (peptic ulcer).
Sometimes pain can be of a psychogenic nature - for example, with an imbalance of the autonomic nervous system (also known as vegetative-vascular dystonia).
Vegetative-vascular dystonia - diagnosis or fiction? Read here
Accompanied by chest pain and diseases of the osteochondral structures of the chest and nerve trunks - including intercostal neuralgia.
— How do you understand that chest pain is threatening and an ambulance should be called immediately?
Here it is important not to miss, in particular, such pathologies as unstable angina, myocardial infarction, pulmonary embolism, and thoracic aortic aneurysm.
For this group of diseases there are common manifestations - “alarm signals” that you should definitely pay attention to. This is most often a fairly severe, acute pain, which differs from the pain noted earlier (if it was noted), and does not go away while taking nitrates. The pain may be accompanied by nausea, vomiting, sweating, and pale or bluish skin. Rapid heartbeat often develops, shortness of breath, suffocation, hemoptysis, drop in blood pressure, pre-syncope or fainting are possible. These signs are a reason to immediately call an ambulance.
— What is intercostal neuralgia?
Intercostal neuralgia is a complex of manifestations that develops when the intercostal nerve or nerves are irritated or compressed. There are doctors who regard it as an independent disease with a clearly defined picture, while others consider it a syndrome that can be caused by a variety of disorders. In any case, intercostal neuralgia is coded in ICD 10 (code G58.0).
— What kind of pain occurs with intercostal neuralgia? By what signs can it be distinguished from other pain?
Intercostal neuralgia is often characterized by a unilateral location of pain (right or left), which is semi-encircling in nature. The patient can describe it quite clearly, i.e. indicate its location, the course of distribution (usually along the intercostal space).
The pain is quite acute, can be constant (with periods of worsening) or paroxysmal. Longer than that with stable angina (with the latter, the pain usually goes away after 3-5 minutes at rest).
Pain with intercostal neuralgia has periods of worsening/improving, is quite clearly associated with physical activity, changes in body position, and can be provoked by coughing, sneezing, or deep breathing. In addition to pain, symptoms such as numbness, burning, pulsation, and involuntary muscle contraction are often encountered in the intercostal space.
The difference between pain in intercostal neuralgia and cardiac pain (in particular angina) also lies in the absence of irradiation to the left arm and lower jaw; no fluctuations in blood pressure; The duration of the pain syndrome also differs (with neuralgia, pain can be bothersome for a long time), there is no effect from taking nitrates, there are no symptoms signaling a serious pathology of the heart and blood vessels. The provoking factors in the occurrence of pain also differ (awkward movement and a deep breath can trigger an attack of pain with intercostal neuralgia); Adopting a pain-relieving position minimizes it in case of intercostal neuralgia, but does not affect the intensity of “heart” pain.
How to avoid running to a hospital bed? What do you need to know about health before buying a gym membership? Read more
— Can there be an increased body temperature with intercostal neuralgia?
No. If such a manifestation occurs, you need to look for another cause of pain in the chest.
— Why does intercostal neuralgia occur?
The mechanisms leading to intercostal neuralgia may be irritation or compression of the intercostal nerve. This may be due to osteochondrosis of the spine, curvature of the spinal axis, spondylosis, damage to the transverse costal joints; after injury to the ribs and chest, excessive muscle tension (in particular intercostal muscles); with excessive mobility of parts of the ribs on the lateral and anterior surface of the chest; Infringement of the 7th-12th nerves in the connective tissue sheaths of the rectus abdominis muscle is less common.
Does osteochondrosis exist? Find out here
Sometimes the cause of intercostal neuralgia can be the herpes zoster virus. In this case, it is coded in a different section of ICD-10, but the manifestations will be generally the same.
In some cases, intercostal neuralgia can occur after suffering from influenza and a number of infectious diseases.
Additional risk factors for the occurrence of intercostal neuralgia may include diabetes mellitus, alcoholism, and impaired absorption of B vitamins.
“Triggering” moments can be a combination of factors: hypothermia, sudden and/or awkward movement, interventions on the thoracic spine (not entirely correct manual therapy, surgery, etc.).
— Can intercostal neuralgia go away on its own or does it need to be treated?
Sometimes it can go away on its own. However, in the absence of treatment, it is likely that the duration of the disease and the treatment time will increase (with therapy, the period of temporary disability is usually 7-14 days), and the process may become chronic, when the pain can last for weeks, and in the case of the herpetic nature of the disease - for months and years.
The question is also that during self-diagnosis, i.e. when the patient decided that he had intercostal neuralgia and did not go to the doctor to prescribe treatment, you can “miss” some other, often serious, diagnosis that resembles neuralgia in its manifestations. At the same time, the consequences without treatment may not be so harmless, and, in addition, time will be lost.
— What is the risk of intercostal neuralgia if it is not treated? How dangerous is this diagnosis?
If left untreated, recovery time may increase or the pain may become chronic.
— Which doctor should you contact for symptoms of neuralgia?
Since intercostal neuralgia can be confused with much more serious, life-threatening diseases, you should first immediately consult a physician or general practitioner. And only after excluding these pathologies, see a neurologist.
You can make an appointment with a therapist here
Please note: consultations are not available in all cities
Occasionally, when there is a need for therapeutic blockades, the help of a neurosurgeon or traumatologist may be needed.
— How is intercostal neuralgia diagnosed?
An ECG and chest x-ray are required, and body temperature is measured.
Are x-rays dangerous? Yulia Aleksandrovna Rutskaya, head of the radiation diagnostics department, tells
"Clinics Expert Kursk"
According to indications - radiography or MRI with myelography of the thoracic spine. Sometimes tests are prescribed to confirm/exclude an acute inflammatory process.
— What should you never do if you have intercostal neuralgia? For example, is it possible to warm the area of pain with a heating pad? Exercise? Go to the bathhouse?
None of the above.
— What is the prognosis for this disease? Is intercostal neuralgia successfully treated?
With correct diagnosis and timely treatment, the prognosis is favorable. This pathology is highly treatable.
— What needs to be done to prevent the development of intercostal neuralgia?
For prevention, it is necessary to avoid hypothermia, sudden and awkward movements (especially if they are unfamiliar, insufficient training or “warming up” before training; within the framework of the work performed); optimize body position in the workplace; engage in physical therapy; undergo regular medical examinations; do not hesitate to consult a doctor if any health symptoms appear.
For reference:
Umerenkova Natalya Vladimirovna
In 2004 she graduated from Kursk State Medical University.
In 2004-2005, she completed an internship in neurology at the above-mentioned university.
Since 2015, he has been working at Clinic Expert Kursk LLC, and is a leading specialist in the neurology department. Receives at the address: st. Karl Liebknechta, 7
Treatment
Treatment is selected taking into account the root cause of the pathological process, as well as the current condition of the patient.
To relieve acute pain during an attack of intercostal neuralgia, painkillers are used. If the pain is very severe, they give injections - injections with solutions of lidocaine and novocaine.
In the acute stage of the pathological process, the patient is prescribed bed rest and rest. Drugs and methods are selected aimed at normalizing the functioning of the nervous and muscular systems:
- B vitamins;
- analgesics;
- muscle relaxants;
- sedatives;
- NSAIDs.
If there is severe swelling of the tissues, diuretics are prescribed to the patient.
If the pathological process is caused by a herpes infection, antiviral and antihistamines are prescribed. If it is not possible to check for infection, they are prescribed for preventive purposes.
The rehabilitation period can last several weeks or even months. How long it lasts depends on the patient's condition. The doctor selects a set of measures aimed at restoring the nervous system:
- exercise therapy;
- massotherapy;
- osteopathy;
- drug therapy.
In the period between exacerbations, mud therapy, as well as radon, sodium chloride, and sulfide baths can be used. Manual therapy, kinesiotaping and acupuncture are used to relax the fascia of the chest and back, improve the functioning of nerve fibers and overall well-being.
How exactly to treat intercostal neuralgia is determined by a neurologist. Self-medication for this disease is unacceptable.
Treatment of intercostal neuralgia
Treatment for intercostal neuralgia depends on what causes it. Statistics say that the vast majority of pain in this area is caused by mechanical causes - pathology of the spine and muscles - osteochondrosis, disc herniation, protrusion, myalgia and myofascial syndrome. Therefore, the answer to the question of how to treat intercostal neuralgia is obvious. Since most of the reasons are mechanical, then they should be eliminated mechanically. This means that the best way to treat thoracic intercostal neuralgia is manual therapy. Moreover, not ordinary, but soft manual therapy, which is not only softer, but also much more effective than simple realignment of the vertebrae. Gentle manual therapy works extremely gently and delicately. Its main advantage is the safe elimination of muscle tension that “pinches” the nerve and stiffens the spine. This is why a chiropractor is the primary physician for intercostal neuralgia. In cases where the problem is advanced, manual therapy can be supplemented with medications and physical therapy.
Treatment of intercostal neuralgia with herpetic lesions requires parallel treatment by a dermatologist. Rare and severe forms caused by fractures and tumors require high-tech and expensive medical care, which is carried out under government programs in specialized clinics.
How to relieve pain from intercostal neuralgia if a person finds himself far from full-fledged medicine and only a pharmacy nearby? Pain in acute intercostal neuralgia is best relieved with the combined use of non-steroidal and steroidal anti-inflammatory drugs. But, we draw your attention - see a specialist as soon as possible. This must be done even if the pain stops completely. It is in your best interests to be sure that nothing more serious lies behind the pain and intercostal neuralgia.
Prevention
Prevention is a simple and affordable way to reduce the risk of intercostal neuralgia in adulthood. It includes moderate physical activity, selected in accordance with the general well-being of the patients. Loads should be dosed and regular, preferably daily.
It is important to monitor your posture. If you are predisposed to disorders, perform a set of exercises aimed at strengthening the muscle corset. To maintain immunity, you should avoid excessive stress and stress, eat well, and avoid hypothermia.

![Rice. 2. Clinical stigmas of chronic atrophic gastritis [4] 2. Clinical stigmas of chronic atrophic gastritis [4]](https://zakam.ru/wp-content/uploads/ris-2-klinicheskie-stigmy-hronicheskogo-atroficheskogo-gastrita-4-fig-2-330x140.jpg)







