Chemotherapy drugs for the treatment of stomach cancer are liquid solutions that are injected slowly into a vein and tablets that are taken by mouth. Both have the same effect on cancer cells, but liquid solutions quickly spread throughout the body through the bloodstream, and tablets are first absorbed in the intestines before entering the bloodstream. This treatment, which affects the entire body, is called systemic chemotherapy.
To treat stomach cancer, either one drug (monochemotherapy) or several (polychemotherapy) can be prescribed, since the drugs act differently and together enhance the antitumor effect.
Chemotherapy treatment is given in cycles of several days followed by rest days. This allows the body to recover before the next cycle. The length of the cycles varies depending on what drugs were used.
In what cases is chemotherapy used in the treatment of stomach cancer?
Chemotherapy is used for locoregional gastric cancer and metastatic gastric cancer. Below, treatment tactics are presented in more detail depending on the spread of the tumor and the general condition of the patient.
Chemotherapy for locoregional gastric cancer
If stomach cancer spreads beyond the first layer of the stomach wall (the lining), it is called locoregional cancer. Such cancer can spread to nearby lymph nodes, but not to those distant from the stomach (this is already metastatic cancer).
Surgery may be an option for treating locoregional tumors. When the tumor has spread to the second layer of the gastric wall (submucosa), surgery is the main treatment option (stage T1b).
If the tumor has grown beyond the second layer of the stomach wall (T2, T3 or T4 tumors), there are several treatment options, but in most cases (T3 and T4 tumors) chemotherapy is prescribed. Chemotherapy can be given either after surgery or in combination before and after surgery (perioperative chemotherapy).
Chemotherapy regimens recommended before and after surgery (perioperative chemotherapy)
| Preferred Modes | Fluoropyrimidines and oxaliplatin |
| Fluorouracil, leucovorin, oxaliplatin and docetaxel (FLOT) | |
| Other modes used | Fluorouracil and cisplatin |
A combination of chemotherapy and radiation therapy (chemoradiotherapy) followed by surgery is also possible. This is called preoperative chemoradiotherapy.
Chemotherapy regimens recommended for preoperative chemoradiotherapy
| Preferred Modes | Fluorouracil and oxaliplatin |
| Fluorouracil and cisplatin | |
| Fluoropyrimidines (fluorouracil or capecitabine) and paclitaxel | |
| Other modes used | Paclitaxel and carboplatin |
When perioperative chemotherapy or preoperative radiation therapy is given, the doctor will order CT scans of the chest, abdomen, and pelvis to make sure the cancer has shrunk enough to be removed by surgery. In this case, a special contrast is injected into a vein or given as a liquid to drink.
If the required tumor reduction is achieved and there are no contraindications for surgical treatment, surgery is performed.
Postoperative adjuvant chemotherapy
This chemotherapy for stomach cancer is prescribed at stages T2-4 N1-3 M0 after surgery, taking into account the situation when the tumor is removed along with the organ. The priority medications are: fluoropyrimidine, oxaliplatin, capicistabine.
For stomach cancer, chemotherapy procedures begin at least 4-6 weeks after surgery so that the body has time to recover, as evidenced by normalized laboratory parameters. Also, the condition for starting chemotherapy is the absence of any complications after surgery. The duration of taking the drugs is at least 6 months.
Having studied this scheme for combating stomach cancer, experts pointed to an increase in three-year disease-free survival from 59% to 74% at any of the previously described stages of disease development. It is worth noting that this method of influencing abdominal tumors is supported by oncologists in Asian countries.
A separate form of treatment, which is recognized as the most effective in the United States, is chemoradiotherapy. In this case, chemotherapy is combined with irradiation of the malignant tumor, significantly increasing the survival rate.
What to do if the tumor cannot be removed surgically?
If you are healthy enough to have major surgery, but the tumor is so widespread that surgery will not be successful, you have other treatment options.
- Chemoradiation therapy as an attempt to cure cancer. It is also called radical chemoradiotherapy.
Chemotherapy regimens recommended for radical chemoradiotherapy
| Preferred Modes | Fluorouracil and oxaliplatin |
| Fluorouracil and cisplatin | |
| Fluoropyrimidines (fluorouracil or capecitabine) and paclitaxel |
- Systemic chemotherapy (see “Metastatic gastric cancer”).
Is chemotherapy necessary if surgical treatment was performed at the first stage?
If treatment began with surgery, the results of surgery are used to decide whether further treatment is necessary.
The surgeon cannot always remove all the tumor he sees. Preoperative examination has certain errors, and the true spread of the tumor is visible only during surgery. If during the operation it becomes clear that the tumor has spread to structures that cannot be removed, the main component of the tumor is removed (if possible), but part of the tumor remains. This operation does not cure, but it reduces the symptoms of the disease and increases the likelihood of a positive response to chemotherapy and radiation therapy, because The smaller the tumor volume, the higher the likelihood of response to treatment.
Palliative care
In essence, this is not treatment, but the creation of the most comfortable living conditions, including pain relief and drug inhibition of tumor growth. This is the main direction of providing care to patients with stage 4 cancer. Such therapy must be carried out to eliminate the symptoms that bring suffering to the patient and his loved ones - severe pain, nausea and vomiting, dizziness, bleeding.
An inoperable (unremovable) stomach tumor also requires therapeutic measures.
- In this case, you can perform a gastrostomy - an artificial insertion of the alimentary canal into the stomach through the abdominal wall, which will allow you to receive nutrition for life.
- Build a bypass junction between the intestinal loops and the stomach - that is, assemble a “labyrinth” through which food can pass unhindered.
- Use the method of endoluminal laser therapy, that is, cut the tumor using a laser that is introduced through the mouth. This is necessary in cases where the entrance to the stomach is blocked by a tumor.
What are the side effects of chemotherapy for stomach cancer?
The side effects of chemotherapy can vary from patient to patient and depend on the type of drug, the amount of drug taken (dose), and the length of treatment. Common side effects are: lack of appetite, nausea, vomiting, diarrhea, hair loss, inflammation and ulcers of the oral mucosa. Brittleness and discoloration of the nails may also occur.
Some chemotherapy drugs harm sensory nerves. This is called sensory neuropathy. Symptoms include numbness, tingling and pain in the fingers and toes. You may also experience increased sensitivity to cold and pain when touched lightly.
At a consultation with an oncologist at the Rassvet Clinic, you can learn how to prevent or reduce side effects. If you are concerned about a side effect, there may be ways to help you feel better.
Intra-arterial course of polychemotherapy
After catheterization of the main vessel of the stomach, an intra-arterial course of polychemotherapy is carried out against the background of artificial hyperglycemia according to the scheme described below. For polychemotherapy, the drugs 5-fluorouracil and adriablastin are used. A single dose of 5-fluorouracil is 1.5 g, adriablastin is 30 mg.
To dilute 1.5 g of fluorouracil, use 400 ml of a 20% glucose solution, the same amount of this solution is required to dilute 30 mg of adriablastin. Using drip systems used for blood transfusions, the drugs are injected into the artery over 90-120 minutes. After completing the administration of the drugs, the catheter must be closed and left in the artery. The following administrations are performed every day for 3-4 days.
The total course dose of chemotherapy drugs is equal to: adriablastine - 90 mg, 5-fluorouracil - 4.5 g. Before each time the drug is administered, the position of the catheter in the gastric vessels is checked by angiography. After completion of drug perfusion, the catheter is removed from the vessel, and a pressure bandage is applied to the site where the femoral artery was punctured for 24 hours.
What to do if the cancer comes back?
A recurrence that occurs close to where the stomach was located (if you had a complete stomach removal) is called a locoregional recurrence . If the cancer comes back and spreads to areas distant from the stomach, it is metastatic disease .
Treatment of locoregional relapse largely depends on two factors:
- whether your health condition allows surgical treatment,
- whether the spread of the tumor allows for a successful operation.
If surgery is not possible, supportive care may be an alternative (see below “Metastatic gastric cancer”).
Causes and risk factors
Today, scientists know that the formation of stomach cancer is caused by the interaction of three components: Helicobacter pylori, the negative influence of external factors and genetic predisposition.
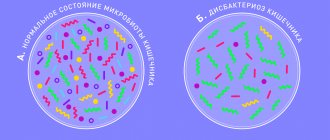
H. pylori is a bacterium that colonizes the mucous membrane of the human stomach and duodenum. In more than 90% of cases this does not manifest itself in any way, in the rest it leads to the development of gastritis and peptic ulcers. In 1994, H. pylori was recognized as a first order carcinogen. It was found that carriers of the bacterium develop stomach cancer 2-6 times more often.
Environmental factors are associated with approximately 80% of gastric malignancies. The appearance of cancer is promoted by poor nutrition, lack of antioxidants, and smoking, which increases this risk by 2-3 times. At the same time, it has been established that an increase in the proportion of dairy products and fruits in the diet is reliably accompanied by a decrease in mortality from stomach cancer.
Most scientists note a connection between gastric carcinomas and underlying diseases that precede the development of a tumor, but do not always lead to them. These include: condition after gastrectomy, chronic hyperplastic gastritis, polyps and some pathological processes.
Metastatic stomach cancer
Treatment options for metastatic tumors are based on the patient's general condition, which is determined by their daily activities and ability to perform daily tasks and activities. The doctor assesses your general condition using one of the two systems described below.
ECOG scale (Eastern Cooperative Oncology Group):
- 0 points—the patient is fully active;
- 1 point - the patient can fully cope with self-care, but it is difficult for him to perform heavy physical work;
- 2 points - the patient is capable of self-care and spends most of his waking time out of bed, but cannot perform any work;
- 3 points - the patient is not able to fully cope with self-care, cannot perform any work and spends most of his waking time in bed;
- 4 points - the patient is completely dependent on outside help.
Karnofsky Performance Status KPS:
- index from 0% to 49% - the patient is not able to care for himself;
- index from 50% to 79% - the patient cannot perform active work and partially needs help;
- index from 80% to 100% - the patient maintains normal activity.
Poor general condition:
If a patient has an ECOG score of 3 or 4, or a KPS of 0 to 59, they are considered to have poor general condition. This means that chemotherapy will likely be too dangerous. In this case, supportive care may be the best treatment option.
Good general condition:
If the ECOG score is 0, 1 or 2, or the KPS is between 60 and 100 points, the patient is considered to be in good general condition. This means he has several options for treating cancer.
Where to start treating metastatic stomach cancer?
Testing should be done to identify tumor markers. These can be used to determine what systemic therapy you may receive:
- HER2;
- PD-L1;
- microsatellite instability (MSI) or abnormalities in the MMR-dMMR system.
For patients with good general status, the following treatments may be used:
- chemoradiotherapy;
- systemic therapy;
- palliative care.
Chemoradiation therapy
A combination of chemotherapy and radiation therapy. This option is suitable for patients who are not candidates for surgery and have not yet received chemotherapy.
Chemotherapy regimens recommended for use in radiotherapy:
- fluorouracil and oxaliplatin;
- fluorouracil and cisplatin;
- fluoropyrimidines (fluorouracil or capecitabine) and paclitaxel.
Systemic therapy
The term "systemic therapy" is used when talking about treating cancer throughout the body. There are first-line treatment drugs that are recommended to start treatment with, since their use has the best results.
First-line systemic therapy
| Preferred Modes | Fluoropyrimidines (fluorouracil or capecitabine) and oxaliplatin |
| Fluoropyrimidines (fluorouracil or capecitabine) and cisplatin | |
| Other recommended modes | Paclitaxel with cisplatin or carboplatin |
| Docetaxel with cisplatin | |
| Fluoropyrimidines (fluorouracil or capecitabine) | |
| Docetaxel | |
| Paclitaxel | |
| Fluorouracil and irinotecan | |
| Docetaxel, cisplatin and fluorouracil | |
| Docetaxel, oxaliplatin and fluorouracil | |
| Docetaxel, carboplatin and fluorouracil | |
| ECF (epirubicin, cisplatin and fluorouracil) | |
| Epirubicin, oxaliplatin and fluorouracil | |
| Epirubicin, cisplatin and capecitabine | |
| Epirubicin, oxaliplatin and capecitabine | |
| If the tumor is HER2-positive, the targeted Trastuzumab is added to the first-line treatment regimen in addition to chemotherapy. Trastuzumab is not prescribed if epirubicin is included in the treatment regimen. | |
Targeted therapy is a new type of systemic therapy. Trastuzumab is a targeted drug used to treat advanced gastric cancer.
More details
Targeted therapy for stomach cancer
During the consultation, the oncologist at the Rassvet Clinic will prescribe a systemic therapy regimen based on data about the patient’s general health and information about the side effects of his treatment.
Two-drug regimens have fewer side effects than three-drug regimens. If you are prescribed fluorouracil (5-FU), leucovorin may be added to your regimen to reduce the side effects of chemotherapy. Regardless of your prescribed medication regimen, you should be examined and tested regularly to evaluate and check for side effects.
If the tumor does not respond to first-line regimens, the subsequent treatment regimen is adjusted depending on the previous treatment regimen and the general health of the patient.
Below are the regimens that have proven to be the most effective in clinical trials as second and subsequent lines of therapy.
Treatment if first-line drugs are ineffective
| Preferred Modes | Ramucirumab and paclitaxel |
| Docetaxel | |
| Paclitaxel | |
| Irinotecan | |
| Trifluridine or tipiracil (third and subsequent line therapy) | |
| Fluorouracil and irinotecan | |
| Pemprolizumab (third and subsequent line therapy, for MSI-H or dMMR tumors) | |
| Other recommended modes | Ramucirumab |
| Irinotecan and cisplatin | |
| Pemprolizumab (third and subsequent line therapy, for patients with PD-L1 marker) | |
| Docetaxel and irinotecan |
Palliative care
Palliative care is specialized medical care aimed at relieving pain and other symptoms of a serious illness. Palliative care specialists work with the patient, the patient's family, and other health care providers to provide a level of support that complements ongoing treatment and care. Palliative care may be used during aggressive procedures such as surgery, chemotherapy, or radiation therapy.
When palliative care is used in conjunction with all other appropriate treatments, cancer patients feel better and tolerate treatment better.
At the Rassvet Clinic, palliative care is provided by a team of doctors, nurses and other specialists. Palliative care teams strive to improve the quality of life for people with cancer and their families. This form of care is offered with most types of treatment a patient may receive.
Good to know
Why is chemotherapy at the Rassvet clinic a good solution?
Diagnosis of the disease
Gastric cancer is a pathology, the effective treatment of which depends on a timely and correct diagnosis, taking into account the stages and morphological type of the malignant process. To conduct a high-quality diagnostic examination, clinics in Russia use only ultra-modern equipment and perform:
- Esophagogastroduodenoscopy (EGD, gastroscopy) with biopsy
is the main method for diagnosing gastric cancer at any stage; During the procedure, a visual assessment of the internal walls and cavity of the esophagus, stomach and duodenum is carried out, which makes it possible to determine the location of the tumor, its shape and size, the degree of narrowing of the stomach, and also to collect material from the pathological area for further histological analysis and diagnosis. - Computed tomography ()
is a method that reflects the prevalence of the oncological process, assessing the condition of the chest, abdominal and pelvic organs; When carried out, it is possible to exclude the presence of distant metastases in other organs and tumor growth into neighboring structures. - Laboratory tests of blood (
including tumor markers)
and urine
. - Diagnostic laparoscopy
is performed, as a rule, before a planned surgical intervention with a confirmed diagnosis of stomach cancer, in order to finally determine the stage of the tumor process and exclude metastases in the peritoneum and liver. - Positron emission tomography (
PET-CT
)
is an additional method that is used to identify lesions suspicious for metastases on CT; This method also allows you to dynamically monitor the effectiveness of treatment of the disease.