Sigmoiditis implies an inflammatory process that occurs in the sigmoid colon. Simply put, a lesion occurs in the final sections of the intestine located in the large intestine.
The sigmoid colon is most vulnerable to inflammatory processes, since it is physiologically designed in such a way that long-term stagnation of the masses located in the intestine is formed in this area, awaiting the formation of fecal waste from them.
Sigmoiditis quite often occurs accompanied by colitis or proctitis. Moreover, this disease has practically no symptoms that separately characterize the presence of sigmoiditis. It is noteworthy that sigmoiditis can occur even in acute and chronic forms.
General characteristics of the disease
Proctitis is a disease of the sigmoid colon.
To draw correct conclusions about the condition of the sigmoid colon, it is necessary to conduct an examination of the processes that occur inside it. It is necessary to study the physiological and anatomical components of the sigmoid colon.
As everyone knows, the intestine has a thick section and a thin section. Each of them is responsible for performing a specific function.
The thin section is responsible for digesting food and absorbing nutrients, while the thick section supplies the blood with water, glucose, vitamins and amino acids. Fecal matter also forms in the large intestine.
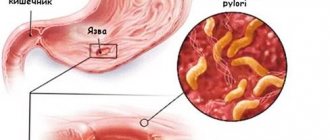
To study sigmoiditis, we need the large intestine. This is where the rectum and colon are located. The terminal portion of the colon is shaped like the letter S, hence the name sigmoid.
Taking as a basis the physiological, anatomical characteristics and the presence of the nearby rectum, we can conclude that sigmoiditis in isolation is quite rare. If it occurs, it is most often in the final section of the gastrointestinal tract.
Treatment methods
The method of combating diverticulosis depends on what stage the disease is at and whether there are complications. The patient’s age, individual characteristics of the body and diet also play an important role.
Drug treatment
Despite the fact that today pharmacies sell many medications to combat this pathology, you cannot prescribe medications for yourself. The dosage and duration of treatment must be selected strictly by the attending physician, otherwise the condition may only worsen.
Typically, patients are prescribed drugs from the following pharmaceutical groups:
- Broad-spectrum antibiotics.
- Anabolic steroids and antispasmodics (No-shpa, Drotaverine).
- Drugs that activate intestinal motility.
- Laxatives.
- Enzymes that have a beneficial effect on digestion.
- Medicines that eliminate diarrhea, bloating and heaviness.
During exacerbation of diverticulosis, taking anabolic steroids is of utmost importance.
Doctors warn patients that the pain can be so severe that a person cannot even stand up. That is why drugs of this pharmaceutical category must certainly be available in your home medicine cabinet.
Physiotherapy
If the patient's condition does not improve, additional measures may be prescribed:
- gastric lavage;
- siphon enemas, which help cleanse the intestines and relieve it as much as possible;
- therapy using crystalloid solutions;
- use of fresh frozen plasma.
Diet
The right foods and diet also help to significantly alleviate the condition and reduce symptoms. Most experts advise their patients to switch to vegetables and fruits, and to include as many grains and cereals in their diet as possible.
It is advisable that dishes from the menu be steamed or boiled; frying food in a frying pan is strictly not recommended. To relieve the load on the intestines and normalize its functioning, you need to eat small portions 5 times a day.
Small meals promote better absorption of food and normalize intestinal activity.
What can you eat if you have diverticulosis? They have proven themselves very well:
- fermented milk products of medium fat content;
- dried apricots and prunes;
- vegetable salads with garlic and olive oil;
- bran, nuts, seeds;
- oatmeal;
- low-fat broths;
- asparagus, spinach and other greens.
To avoid complications and not slow down recovery, it is recommended to completely eliminate the following products:
- sweets (gingerbreads, candies, buns);
- chips, crackers, salted nuts;
- fast food;
- soda;
- strong tea or coffee;
- alcoholic products.
Exercise therapy
Special therapeutic exercises will also help normalize the activity of the digestive system and intestines. To achieve maximum results and not injure organs, gymnastics should be performed in a specialized center under the supervision of a doctor.
The most effective are sets of exercises designed for the abs and pelvic muscles, but they need to be done without zeal, the load should increase gradually.
Surgical intervention
If complex treatment does not bring improvement, surgical removal is prescribed. The following complications are also indications for surgery:
- severe bleeding;
- peritonitis;
- the appearance of fistulas;
- constant exacerbations of the disease.
Such operations are not considered complex; during them, the surgeon simply removes the affected area of the intestine.
Symptoms of sigmoiditis
Abnormal bowel movements are a symptom of sigmoiditis.
The manifestation of symptoms of a disease such as sigmoiditis is influenced by a number of factors. Factors characterizing this disease:
- Certain type of sigmoiditis (acute or chronic stage)
- General nature of the inflammatory process (catarrhal/erosive or ulcerative sigmoiditis)
- Motility disorders (spastic or paralytic sigmoiditis)
- Presence of scale of complications (local or distant)
Although rare, the following symptoms of sigmoiditis may appear:
- Painful sensations
- Abnormal stool
- General disorder of the human condition
In typical cases, the location of the pain can be determined. Usually it is concentrated during the inflammatory process in the lower abdomen on the left. The pain is quite intense and can radiate to the lower back or left leg.
Sometimes pain in the sigmoid colon can be confused with pain during acute inflammation of appendicitis. However, this is easy to check; every doctor can do it.
The scale of manifestation of symptoms of sigmoiditis directly depends on the anatomical features of the sigmoid colon. The anatomical features of the sigmoid colon are that the length of the sigmoid colon can reach from 16 to 63 cm.
Moreover, on such a long section there is a mesentery, which affects the mobility of the department. In this regard, it is quite possible for the sigmoid colon to shift to the right side of the abdomen. In this case, to determine the localization of the inflammatory process, it will be necessary to carry out differential diagnosis.
As practice shows, increased pain with sigmoiditis is observed in the following cases:
Drugs
Treatment with antibiotics and anti-inflammatory substances is justified for diverticulitis. Conservative therapy, in addition to antibacterial agents, for inflammation, looks like this:
- substances to improve intestinal motility;
- antispasmodics;
- laxatives;
- vitamin complexes;
- medications for hemoglobin growth.
In case of complications in the hospital, medications are administered intravenously, which increases the effectiveness of treatment. Nutrition is administered parenterally, which makes it possible to “rest” the gastrointestinal tract.
Early stage sigmoid diverticulosis can be treated with medication. The main medications on the list are:
| Alpha Normix | An antibiotic belonging to the broad-range group. Presented in the treatment of infectious diseases of the gastrointestinal tract, diverticulosis of the sigmoid colon. Recommendations for use prescribe a dosage of 200 mg for adults and children over the age of twelve years. Reception is carried out every 8 hours. The duration of therapy does not exceed 7 days. The medicine can be taken in a repeated course, but only after a break of a month. Price from 650 rubles. |
| Amoxiclav | Belongs to the group of penicillins. Prescribed for inflammation of the urinary tract, problems with the gastrointestinal mucosa. The dosage is 1 pill. The break between doses is also 8 hours. The dosage is prescribed for adults and children over twelve years of age. Cost from 200 rubles. |
| No-Shpa | Shows a calming effect on spasms of the smooth muscles of the digestive organs. The dosage for an adult is from 120 to 240 mg throughout the day. The drug can be divided into 3 doses. Cost from 50 rubles. |
| Buscopan | Prescribed to relieve spasm of the muscles of internal organs, reduces the secretion of the digestive glands. The instructions for use indicate a dosage of 1-2 pills after meals. Take up to 5 times within 24 hours. Cost from 330 rubles. |
| Duphalac | The drug belongs to the laxative group and is sold in syrup form. Helps with long-term constipation. According to the instructions, you can take from 15 to 45 ml. The medicine does not need to be diluted. Cost from 290 rubles. |
| Domperidone | An antiemetic drug that eliminates the feeling of nausea. The drug alleviates dyspeptic symptoms associated with decreased gastric emptying. Adults and children over five years of age are prescribed 10 mg three times within 24 hours, thirty minutes before meals. |
| Linex | A complex remedy that belongs to the group of drugs that normalize intestinal microflora. Prescribed when the composition of the normal intestinal flora changes. A child over twelve years old and an adult are prescribed two capsules per day. Cost from 250 rubles. |
What are the symptoms of acute and chronic sigmoiditis?
With sigmoiditis, nausea and vomiting may occur.
As previously noted, sigmoiditis can occur in acute and chronic forms. Each form has certain features.
Acute form of sigmoiditis. The development of acute sigmoiditis occurs spontaneously, unexpectedly. There are often situations when the pain syndrome is so severe that there is a need for differential diagnosis.
This diagnosis will be carried out in comparison with the presumptive diagnosis of acute appendicitis, renal colic, and gynecological diseases. In addition to acute pain in the left side of the abdomen, the following symptoms may be observed:
- Frequent loose stools
- Discharge of blood and pus in the stool
- Nausea
- Vomiting (without feeling of relief)
- Fever
- Tenesmus
Chronic form of sigmoiditis. This form of the disease proceeds according to the principle of remission, i.e. periodic manifestations of pain and then inflammation subsides. Exacerbation of sigmoiditis can be provoked by:
- Diet violation
- Stress
- Hypothermia
- Injuries
- acute respiratory infections, flu
Regarding the symptoms of chronic sigmoiditis, it should be noted that it completely depends on the symptoms of the disease that provoked the formation of chronic sigmoiditis.
Therapy
Treatment of diverticulosis and diverticulitis of the colon depends on the severity of the clinical picture.
Treatment of diverticular disease
Most cases of diverticulosis can be treated at home. You need to understand that it is impossible to eliminate pouch-like protrusions of the intestinal wall using conservative methods.
To relieve the symptoms of the disease, the patient is recommended to take painkillers, for example, Paracetamol. Non-steroidal anti-inflammatory drugs (Aspirin, Ibuprofen) should not be taken, as they increase the risk of bleeding.
To relieve symptoms of the disease, doctors recommend following a diet rich in fiber. It should be remembered that the effect of such nutrition may take several weeks.
If you have constipation, you can use laxatives that increase the volume of stool.
Symptoms of catarrhal and erosive forms of sigmoiditis
Sigmoiditis can be caused by an intestinal infection.
In addition to acute and chronic forms of sigmoiditis, depending on the degree of damage to the sigmoid colon, the following forms also differ:
- Catarrhal. This is the mildest form of sigmoiditis. In the catarrhal form of this disease, the surface of the epithelial layers is damaged, but without gross violations of their integrity.
- Erosive. With erosive sigmoiditis, damage to epithelial cells in the superficial layers is possible.
- Ulcerative. The development of ulcerative sigmoiditis is provoked by the progression and deepening of erosion to layers located deeper in the intestinal mucosa.
- Perisigmoiditis. This is a particularly neglected option. The inflammatory process spreads along all layers of the walls of the sigmoid colon, extending beyond its limits, affecting the visceral peritoneum. As a result, the sigmoid colon loses its mobility and fuses with nearby tissues and organs.
- Hemorrhagic sigmoiditis. Its characteristic feature is an inflammatory process with the formation of pinpoint bleeding.
- Purulent-hemorrhagic. A feature of purulent-hemorrhagic sigmoiditis is the continuation of a more advanced form of hemorrhagic sigmoiditis. In addition to pinpoint bleeding, purulent discharge is also added.
Learn more about diseases and treatment of the sigmoid colon in the thematic video:
Authorized Products
The diet for proctosigmoiditis occurring with diarrhea should include:
- Soups on low-fat broth with pureed vegetables and cereals (buckwheat, semolina, rice) without spices or frying. You can add pureed (scrolled in a meat grinder) boiled meat, egg dressing or meatballs to soups.
- Low-fat boiled or steamed fish. Depending on the period of the disease and the condition of the patient, fish can be served in pieces or pureed (mashed potatoes, soufflés, steamed cutlets, meatballs with rice). Cutlets and meatballs can be cooked in a small amount of water (stewed or poached).
- Any slimy dishes (mashed porridge, jelly, jelly, mashed potatoes).
- Wheat stale bread (no more than 200 g per day).
- Lean meat and poultry. Soufflés, quenelles, cutlets or meatballs are prepared from them. If necessary, to further spare the mucous membrane, the meat is passed through a meat grinder several times.
- Puree porridges cooked in water. You can eat rice, oatmeal or buckwheat porridge.
- Eggs in the form of an omelet, soft-boiled and in soups in the form of an egg-milk mixture. You can consume up to two of them per day.
- Boiled pureed vegetables in the form of puree (zucchini, pumpkin, potato, cauliflower). The consumption of vegetables is excluded in case of diarrhea or poor tolerance to the patient.
- Baked apple puree and mashed raw apples in remission.
- Non-acidic pureed cottage cheese - it can be consumed in its natural form and in dishes.
- Butter in dishes.
- Green tea, cocoa prepared with water, diluted fruit juices, weak black tea, rosehip infusions, jelly made from astringent berries (blueberries, bird cherry, currants, quince, dogwood, pears).
If you have constipation:
- Fruits that stimulate intestinal function: figs, apricots, melons, plums, prunes, peaches, soaked dried fruits.
- Fiber-rich foods: sauerkraut (if tolerated), other vegetables, wholemeal bread (bran or grain). If tolerated well (no bloating), rye bread is allowed. All bread products should be consumed stale or dried.
- Vegetable snacks (fresh or boiled). If well tolerated, the amount of vegetable dishes should be increased. These can be carrot and pumpkin purees, vegetable stews and casseroles. All vegetable dishes need to add various vegetable oils.
- Soups with weak broth. Preference is given to vegetable first courses. If tolerated well, you can eat cabbage soup, borscht, and beetroot soup.
- Chicken, beef, turkey, fish, cooked by boiling or baking.
- Loose porridges, puddings and casseroles. Dishes can be prepared from buckwheat and, if tolerated, millet and wheat porridge are allowed. Eliminate or consume very limited rice and semolina porridge.
- Vegetable oil for ready-made dishes and salads. You can use olive, corn, rapeseed, sunflower oils.
- Milk, sour cream (in dishes), kefir, low-fat yogurt. It should be borne in mind that cottage cheese and cheeses consumed in large quantities can cause constipation.
- Weak tea and coffee with milk, fruit and vegetable juices.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| potato | 2,0 | 0,4 | 18,1 | 80 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| parsley | 3,7 | 0,4 | 7,6 | 47 |
| beet | 1,5 | 0,1 | 8,8 | 40 |
| dill | 2,5 | 0,5 | 6,3 | 38 |
| green beans | 2,8 | 0,4 | 8,4 | 47 |
Fruits | ||||
| pears | 0,4 | 0,3 | 10,9 | 42 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Nuts and dried fruits | ||||
| dried pears | 2,3 | 0,6 | 62,6 | 249 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| oat groats | 12,3 | 6,1 | 59,5 | 342 |
| cereals | 11,9 | 7,2 | 69,3 | 366 |
| white rice | 6,7 | 0,7 | 78,9 | 344 |
Flour and pasta | ||||
| noodles | 12,0 | 3,7 | 60,1 | 322 |
Bakery products | ||||
| white bread crackers | 11,2 | 1,4 | 72,2 | 331 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jam | 0,3 | 0,1 | 56,0 | 238 |
| marshmallows | 0,8 | 0,0 | 78,5 | 304 |
| fruit and berry marmalade | 0,4 | 0,0 | 76,6 | 293 |
| meringues | 2,6 | 20,8 | 60,5 | 440 |
| paste | 0,5 | 0,0 | 80,8 | 310 |
| Maria cookies | 8,7 | 8,8 | 70,9 | 400 |
Dairy | ||||
| skim milk | 2,0 | 0,1 | 4,8 | 31 |
| kefir | 3,4 | 2,0 | 4,7 | 51 |
| sour cream | 2,8 | 20,0 | 3,2 | 206 |
| acidophilus | 2,8 | 3,2 | 3,8 | 57 |
Cheeses and cottage cheese | ||||
| cheese | 24,1 | 29,5 | 0,3 | 363 |
| cottage cheese 0.6% (low fat) | 18,0 | 0,6 | 1,8 | 88 |
Meat products | ||||
| boiled beef | 25,8 | 16,8 | 0,0 | 254 |
| boiled veal | 30,7 | 0,9 | 0,0 | 131 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken | 25,2 | 7,4 | 0,0 | 170 |
| turkey | 19,2 | 0,7 | 0,0 | 84 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
| green tea | 0,0 | 0,0 | 0,0 | — |
| black tea | 20,0 | 5,1 | 6,9 | 152 |
Juices and compotes | ||||
| Orange juice | 0,9 | 0,2 | 8,1 | 36 |
| Cherry juice | 0,7 | 0,0 | 10,2 | 47 |
| Strawberry juice | 0,6 | 0,4 | 7,0 | 31 |
| tangerine juice | 0,8 | 0,3 | 8,1 | 36 |
| carrot juice | 1,1 | 0,1 | 6,4 | 28 |
| tomato juice | 1,1 | 0,2 | 3,8 | 21 |
| pumpkin juice | 0,0 | 0,0 | 9,0 | 38 |
| Apple juice | 0,4 | 0,4 | 9,8 | 42 |
| * data is per 100 g of product | ||||
Causes of the disease
The reasons that provoke the occurrence of sigmoiditis are very diverse. In general, they are conditionally grouped as follows:
- Acute and chronic form of sigmoiditis caused by intestinal infections. These include: dysentery and similar intestinal infections.
- Non-ulcer chronic sigmoiditis. Intestinal dysbiosis contributed to its occurrence. Sigmoiditis caused by inflammatory bowel disease. Such diseases include: Crohn's disease, ulcerative colitis.
- Sigmoiditis, which was caused by circulatory failure in the intestines. Radiation sigmoiditis. It occurs primarily during the treatment of cancer by performing radiation therapy in the area of the lymph nodes or pelvis.
Don’t be lazy to get examined at least once a year. This will help you prevent the development of diseases, and, importantly, will cost you less material costs than when treating an advanced form of the disease.
Causes of proctosigmoiditis in adults
Various aggressive factors affect the mucous membrane, which serves as a barrier between the intestines and the external environment.
Often it is infections and parasites that cause proctosigmoiditis. Pathogenic flora and helminths affect the intestinal mucosa with their toxins and also damage it mechanically.
The toxic effect of medications is also possible: heavy antibiotics, constant use of laxatives, alcohol, and other substances. They support chronic inflammation.
Sometimes the body’s own immunity attacks: autoimmune intestinal pathology, as well as allergies. Constantly eating food that the body cannot tolerate leads to damage to the intestinal mucosa and increased permeability of the intestinal lining.
Poor blood supply affects the condition of the mucous membrane. Older people often experience atherosclerosis of the vessels of the mesentery, the organ that attaches the intestines to the walls of the abdominal cavity. Elderly people often suffer from constipation. Excess feces stretches the intestines and damages the mucous membrane. Intoxication with food breakdown products also occurs.
Disturbances in the functioning of other digestive organs affect the condition of the underlying sections. For example, with pancreatitis or cirrhosis of the liver, a lack of enzymes leads to poor digestion of food even at the stage of the small intestine. Thus, unprocessed substances pass lower into the large intestine, and inflammation develops.
Oncology, as well as the treatment of this disease, can also provoke proctosigmoiditis. Tumor cells release toxins into the intestines, causing a pathological immune response. And radiation therapy also injures the intestine itself, and not just the tumor.
Diagnosis of sigmoiditis
X-ray examination will help identify sigmoiditis.
Sigmoiditis can be diagnosed only after a detailed examination.
And then, based on the data obtained, you can safely make a diagnosis and prescribe treatment. The patient will need to undergo a number of studies, namely:
- Palpation. This is necessary to determine compaction and pain in the area of the sigmoid colon.
- Macroscopic examination. The test will be performed on the patient's stool. The stool will be examined for mucus, pus, and blood.
- Microscopic studies. This study will determine the presence of red blood cells, white blood cells and epithelial cells.
- Biochemical research. Using a biochemical study of stool, the content of enzymes and protein will be revealed.
- X-ray examination. Using this type of study, pathology in the folds of the intestinal mucosa, a general decrease in the number of folds, rigidity of the intestinal walls, and other defects will be identified.
DIVERTICULOSIS: fiber plays the main role in its treatment
Claire Cheek, Fellow of the Royal College of Physicians Simon Radley, MD, Fellow of the Royal College of Physicians Queen Elizabeth Hospital, Birmingham, UK
How does diverticular disease manifest? What complications may develop? Which patients need to be hospitalized?
Colon diverticulosis is an acquired disease. It is believed that it is based on impaired peristalsis, which leads to the appearance of areas with high intraluminal pressure, pushing the mucous membrane through the submucosal and muscular layers. This occurs in relatively weak areas where blood vessels extend into the circular muscle.
Impaired peristalsis may occur due to the frequent passage of small volumes of stool with a low content of undigested food debris. Both circular and longitudinal muscle bundles usually hypertrophy, which leads to thickening and shortening of the colon. Diverticula and muscle hypertrophy are most often observed in the sigmoid colon, but the colon can also be affected in any part or completely.
The term “diverticulosis” simply reflects the presence of diverticula, not necessarily the clinical manifestation of the disease. Diverticulitis is a clinical and morphological concept that refers to inflammation of diverticula. Diverticular disease is a broader term that applies to diverticulosis and its complications.
Diverticulosis is very rare in people under 30 years of age, but its incidence increases with age, and by age 50, up to 30% of the population has colonic diverticula. The frequency of this pathology in men and women is the same.
Only 20% of people with diverticulosis eventually develop symptoms of the disease.
This disease is characteristic of Western countries, its pathogenesis is largely associated with insufficient fiber intake. It is observed less frequently in vegetarians and rural Africans.
Thus, environmental factors are believed to play an important role in the development of this pathology. Nevertheless, genetic factors seem to have a certain significance: in cases where diverticula appear at a young age or when they predominantly affect the right parts of the colon.
Clinical picture. Most patients with diverticulosis do not have any complaints. With uncomplicated diverticular disease, bowel dysfunction may occur, often accompanied by pain such as colic, flatulence and a feeling of fullness in the abdomen. These symptoms can sometimes be difficult to distinguish from irritable bowel syndrome.
Acute diverticulitis is characterized by pain in the left iliac fossa. Typically, there are signs of acute inflammation, namely: tachycardia, fever, local peritoneal phenomena and leukocytosis.
Perforation of an inflamed diverticulum can lead to abscess formation. Such patients often have a fluctuating fever and a painful mass in the affected area.
Diverticular abscesses often resolve spontaneously. However, large or nonabsorbing abscesses may require percutaneous drainage under ultrasound or CT guidance. Perforation of a diverticular abscess into the abdominal cavity causes purulent peritonitis, with local tenderness becoming diffuse.
The local inflammatory process associated with the diverticulum can lead to perforation of the wall of another organ lined with epithelium, resulting in the formation of a fistula. The most common cause of diverticular disease is colovesical fistulas, which occur when a diverticulum perforates into the bladder. When first seeing a doctor, patients with colovesical fistulas sometimes have no complaints of bowel dysfunction, but instead experience frequent urinary tract infections and/or pneumaturia.
Fistulas can also open into other organs - the vagina or loops of the small intestine, and occasionally enterocutaneous fistulas occur.
Diffuse peritonitis associated with diverticular disease is caused by the presence of free pus and/or feces in the abdominal cavity. Fecal peritonitis develops as a result of necrosis of the intestinal wall, leading to leakage of feces. The patient's condition can be very severe, with severe symptoms of peritonitis and septic shock.
Sometimes bleeding occurs from the vessels passing through the neck of the diverticulum, and more often it is profuse. Typically, such bleeding develops from a single diverticulum, located, as a rule, in the right parts of the colon.
Diverticular disease cannot be considered as a cause of occult bleeding from the lower gastrointestinal tract leading to iron deficiency anemia, for which other causes should be sought, such as neoplasms or angiodysplasia.
Inflammatory changes in combination with smooth muscle hypertrophy and scarring from previous attacks of acute diverticulitis may be sufficient to cause complete closure of the colonic lumen and acute obstruction. Incomplete obstruction due to scarring is manifested by unstable stools and abdominal pain such as colic. Using imaging techniques, it can be very difficult to distinguish strictures resulting from diverticular disease from malignancy.
Diagnostic methods. Diverticulosis is easily detected by irigoscopy and computed tomography (CT) with contrast.
| Figure 1. Irigoscopy: uncomplicated diverticulosis of the sigmoid colon | Figure 2. Irigoscopy: diverticular disease of the sigmoid colon. Fistula (arrow) connects the intestine to the bladder (B) |
Double-contrast irigoscopy identifies diverticula (see Fig. 1), any strictures, and can also help detect fistulas (see Fig. 2).
If in areas with severe diverticulosis it is sometimes not possible to reliably exclude small polyps or carcinomas, then it is necessary to perform a colonoscopy or flexible sigmoidoscopy.
Irigoscopy with double contrast can be performed only four to six weeks after relief of acute diverticulitis.
In acute pathological processes, other diagnostic techniques play a major role, such as CT and/or sonography.
Colonoscopy. Colonoscopy is usually performed on an outpatient basis. It allows you to clearly visualize diverticula and any pathology of the mucosa. This is the diagnostic method of choice in cases where the patient is admitted with rectal bleeding or during irigoscopy it was not possible to thoroughly examine the colon.
However, colonoscopy is sometimes difficult to perform because of the spasm observed with extensive diverticular disease, as well as because of rigidity or because of the diverticula themselves.
| Figure 3. Computed tomography with contrast: diverticular disease of the sigmoid colon (S) complicated by the formation of an abscess (A) containing a large amount of gas (arrow) |
Computed tomography and sonography. Contrast-enhanced CT is the study of choice in patients with acute diverticulitis.
Often during this procedure, a characteristic thickening of the walls of the colon with inflammation of the surrounding fatty tissue is detected. In complicated cases, CT scan reveals abscesses (see Fig. 3), gas and/or contrast material outside the bowel loops. Many departments practice drainage of abscesses in the abdominal cavity under CT control, which helps avoid surgical interventions in the acute phase of the disease. Sonography is slightly less sensitive but can detect wall thickening and large abscesses.
Other research methods. Occasionally, cystoscopy may be necessary to detect a colovesical fistula. Angiography and scanning with technetium-labeled red blood cells can help locate the source of blood loss from the colon.
Referral to hospital. Patients with abnormal stools, blood on rectal examination, or recurrent abdominal pain should be examined on an outpatient basis to determine the causes of these symptoms. Rigid sigmoidoscopy and irigoscopy or complete colonoscopy are the main methods used in this case. Asymptomatic diverticula occur in at least one in three people over 65 years of age. Therefore, diverticulitis can be reliably diagnosed only when there is an appropriate clinical picture and when no other diseases, especially malignant tumors, are detected.
A patient with acute diverticulitis without dysfunction of other body systems does not necessarily need to be treated in a hospital. In such cases, home treatment consisting of oral antibiotics (amoxicillin with clavulanic acid and metronidazole for five days) and drinking plenty of fluids is often sufficient. Analgesics and bed rest are also prescribed. If within a few days the pain does not stop or intensifies or becomes more widespread, and also if the patient develops systemic symptoms (for example, tachycardia or fever), then it is necessary to immediately refer him to the hospital.
| Figure 4. Complicated diverticular disease. The probe is inserted into the perforated diverticulum. The mucous membrane looks quite normal |
Patients with diffuse abdominal pain and/or signs of peritonitis should be urgently hospitalized.
Drug and surgical treatment. In uncomplicated cases, special nutrition may be sufficient for treatment. The patient is advised to eat a high-fiber diet and/or take medications that increase stool bulk, such as ispaghula husk. Patients should drink plenty of fluids.
Pain caused by smooth muscle spasms should be relieved with antispasmodics such as mebeverine. The role of surgical resection in uncomplicated cases remains controversial and should be reserved for exceptional cases.
Laporotomy and myotomy (dissection) of hypertrophied smooth muscle of the sigmoid colon have rightly been criticized and are currently only of historical interest.
Elective surgery. In case of complications, such as fistulas or strictures, surgical intervention is required with resection of the segment of the colon affected by diverticula and a primary anastomosis. For patients with recurrent diverticulitis, resection is offered in cases where their physical condition allows such an intervention - if other pathology is excluded.
One third of patients who are hospitalized for an attack of diverticulitis have to be hospitalized again in the next five years with the same pathology.
Elective surgery is associated with much lower complication rates and mortality; Resection and primary anastomosis can usually be achieved, although a stoma may sometimes be required.
Emergency surgery. For patients with generalized peritonitis, effective resuscitation measures with intravenous fluid and antibiotics are required before surgery.
Perforation of the colon is a serious situation, and almost half of patients with fecal peritonitis die. Purulent peritonitis, which develops as a result of rupture of a diverticular abscess, has a lower, but still significant mortality rate.
Patients with acute diverticulitis that does not respond to conservative treatment may also require surgery. In such cases, the inflamed segment with diverticula or phlegmon is resected, and it is usually possible to perform a primary anastomosis.
In case of extensive fecal or purulent contamination of the abdominal cavity, resection of the affected segment is necessary, but primary anastomosis is not always appropriate. In such cases, the rectal stump is sutured and the proximal colon is exposed to the skin as a final colostomy. This intervention is called Hartmann's operation.
After Hartmann's operation, in most cases it is possible to close the colostomy without any risk, and, according to numerous data, in 80% of cases the normal passage of intestinal contents is restored.
If complications develop, then exclusion of the affected segment from the intestinal function is carried out by applying a bypass anastomosis and establishing drainage of the abdominal cavity. But in such situations, this segment is not resected, which leads to a significant increase in mortality compared with primary resection. Therefore, the vast majority of surgeons refused such an operation.
In case of complications of diverticular disease, severe concomitant diseases and old age negatively affect the outcome of emergency surgery.
Literature
- Pemberton JH, Armsrong DN, Dietzen CD Diverticulitis. In: Textbook of Gastroenterology, 2nd edition (Ed. Yamada T). Lippincott. Philadelphia. 1995.
- Keighley MRB Diverticular disease. In: Surgery of the Anus, Rectum and Colon, 1st edition (Eds. Keighley MRB, Williams NS). W. B. Saunders, London. 1993.
Editor's comment
- In accordance with the “Standards for the diagnosis and treatment of diseases of the digestive system,” which are approved by order of the Ministry of Health of the Russian Federation No. 125 dated April 17, 1998, lactulose (Duphalac) is the first choice for diverticular disease with a tendency to constipation.
- In the Russian Federation, mebeverine is registered under the trade name Duspatalin
Note !
- Acute diverticulitis is characterized by pain in the left iliac fossa and is usually accompanied by signs of acute inflammation, namely tachycardia, fever, local peritoneal findings and leukocytosis
- Perforation of an inflamed diverticulum can lead to abscess formation. Such patients sometimes have a fluctuating fever and a painful mass in the affected area.
- Sometimes bleeding occurs from the vessels passing through the neck of the diverticulum, quite often profuse. Diverticular disease cannot be considered a cause of occult bleeding from the lower gastrointestinal tract leading to iron deficiency anemia
- Patients with changes in stool, blood on rectal examination, or recurring abdominal pain should be evaluated in an outpatient setting to determine the cause of these symptoms. Rigid sigmoidoscopy and irigoscopy or complete colonoscopy are the main methods used in this case. In uncomplicated cases, special nutrition may be sufficient for treatment. Patients are advised to eat a high-fiber diet and/or medications that increase stool volume, such as ispaghula husk.
- Pain caused by smooth muscle spasms should be relieved with antispasmodics. The role of surgical resection in uncomplicated cases remains controversial and should be used with great caution
What to tell the patient?
In uncomplicated cases
- The examination did not reveal any severe disease of the colon, including a malignant tumor.
- It is very important to pay attention to nutrition
- It is necessary to eat foods rich in fiber and take medications that increase the volume of stool
- You should drink more fluid
- Increasing the fiber content of your diet may initially increase pain and bloating. Stick to your diet anyway as these symptoms usually go away
- Surgery is risky and may not improve the condition.
For complications
- After the first attack, 30% of patients develop an exacerbation of the disease within five years, requiring hospitalization
- Economical surgery can be recommended for young patients
- When considering the possibility of economical resection for patients in the older age group, one should carefully weigh, on the one hand, the possibility of preventing relapses and relieving symptoms, on the other hand, the significant risk of postoperative complications
- Surgery is indicated for patients with fistulas
- If there are no contraindications, economical resection is recommended for patients with abscesses.