Proctitis
In this variant of UC, the affected area is limited to the rectum.
The basis of treatment is topical therapy, which begins with drugs of 5 aminosalicylic acid (5 ASA) in the form of suppositories (500 mg of mesalamine 2 times a day) or microenemas (2-4 grams of mesalamine in 30-60 ml at night). The percentage of achieving remission depends on the duration of use of the drug. On average, a response can be expected after 2-3 weeks of treatment, the average duration of treatment is 3-6 weeks (or until clinical and endoscopic remission is achieved). If there is no effect after 6 weeks of treatment, further use as monotherapy is most likely useless. Topical therapy with 5 ASA drugs is more effective than their oral administration in the treatment of this form of UC [5]. If there is no effect or intolerance to 5 ASA drugs, the question of using steroids arises. It must be remembered that aminosalicylic acid preparations are clinically and economically more effective than steroids in the treatment of proctitis [11], however, when treatment with them is not effective, the use of steroids is justified. Hydrocortisone is used at a dose of 100 mg at night. After administration, the patient should lie on his left side for at least 30 minutes (as in the case of using 5 ASA drugs in enemas). It is advisable that the patient hold the enema for at least an hour, and ideally overnight. In severe cases, you can use enemas with hydrocortisone 2 times a day, followed by a reduction to 1 time. Clinical response can be observed as early as 3-5 days. Treatment should be continued until remission is achieved. If therapy is completely ineffective within 2-3 weeks, further treatment with hydrocortisone is pointless. After a course of treatment longer than 21 days, drug withdrawal should be carried out gradually by prescribing the drug every other day for 2-3 weeks. Patients tolerate hydrocortisone better in the form of foam containing 90 mg of the drug in the form of a 10% aerosol foam suspension. Hydrocortisone is also available in the form of rectal suppositories containing 25 mg or 50 mg of the drug. They are used in a dose of 75-100 mg per day in 2-3 doses. The combination of 5 ASA drugs and steroids is more effective than each of them separately.
Budesonide (a steroid with less systemic activity than hydrocortisone) with similar efficacy results in less impact on plasma cortisol levels. A similar effect is ensured by rapid biotransformation in the liver. Microenemas containing this drug are produced by Astra Zeneca, under the name Entocort. The use of Budesonide or mesalamine (4 g per day) as topical therapy for UC after four weeks of treatment led to improvement in 67% and 71% of cases, respectively, and plasma cortisol levels were similar in both groups [16]. Bianchi Porro G. et al. demonstrated equal effectiveness of Entocort and hydrocortisone in patients with active distal colitis [3]. In another study, Entocort was as effective and well tolerated as mesalamine in the treatment of distal colitis and proctitis [8]. Topical steroids also include tixocortol and beclomethasone diproprionate. A meta-analysis of steroid use in UC demonstrated that Budesonide has similar efficacy to other steroid drugs but causes less reduction in endogenous plasma cortisol levels and less severe side effects. However, it is inferior to 5 ASA drugs in terms of clinical and economic effectiveness [11].
The use of 5 ASA drugs in combination with steroids (for example, every other day) leads to better clinical results than either drug alone [12].
If there is no result from topical therapy (or if it is desired to achieve an effect in a shorter time), there is a need for systemic use of aminosalicylates or steroids, which we will discuss in the next section.
"Zeposia": mechanism of action of ozanimod
Ozanimod (RPC1063) is an oral, small-molecule, selective agonist of sphingosine-1-phosphate receptors 1 and 5 (S1PR1 and S1PR5). The immunomodulatory mechanism of action of ozanimod is due to the internalization of S1P receptors with their subsequent degradation (functional antagonism) in the ubiquitin-proteasome metabolic pathway. This leads to inhibition of the migration of a certain subtype of activated lymphocytes (T-helper CD4+ CCR7+ and T-killer CD8+ CCR7+) from lymphoid tissue to sites of inflammation. At the same time, the integrity of immunological surveillance of infections and tumors is maintained, since S1P signaling does not affect the subset of lymphocytes that do not migrate through lymphoid tissue.
Distal and left-sided colitis
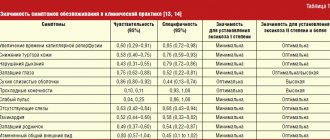
With distal colitis, 30-40 cm of the colon is involved in the inflammatory process; if it reaches the splenic angle, they speak of left-sided colitis. For mild forms of distal colitis, treatment is similar to that for proctitis. In moderate and severe forms, as in left-sided colitis, not only topical but also systemic therapy is most often required. Thus, the combination of systemic and local use of 5 ASA drugs, according to one study, led to faster and more complete control of symptoms than each type separately [17]. Among the drugs in this group, sulfasalazine, mesalamine and balsalazide are used. A meta-analysis comparing placebo sulfasalazine and other 5-ASA drugs showed that both sulfasalazine and the new 5-ASA drugs were superior to placebo in all parameters studied. New 5 ASA drugs had a slightly better therapeutic effect than sulfasalazine and were better tolerated [19]. Mesalamine is usually prescribed in a dose of 2-4 g. per day, which can be increased to 6 grams if necessary. Balsalazide is used in a daily dose of 6.75 g. for 3 doses over 8-12 weeks. There are studies indicating that this drug in a standard dose leads to a higher percentage of achieving remission and a faster (12-14 days) onset compared to mesalamine (2.4 g per day), and is also easier to tolerate by patients [6, 15].
Prednisolone (40-60 mg) is used in patients with severe forms of colitis or when the above-mentioned therapy is ineffective. An analysis of steroid therapy for UC showed that their use leads to complete remission in 54% of cases, partial remission in 30% of cases, and in 16% of patients they are not effective. After a year, 22% of patients experience steroid dependence, and 29% require surgical treatment [4].
Possibility of complete recovery
Since the disease is autoimmune in nature, the exact cause of its development has not been determined, and it is not possible to accurately predict the possibility of a complete cure. No doctor, not even the most experienced gastroenterologist, surgeon, or proctologist, can answer this question. The difficulty of the answer is formed from the following characteristics of the pathology:
- chronic course of the process with periodic exacerbation under the influence of damaging factors;
- cyclicity of symptomatic manifestations with periodic development of remission or relapse;
- deterioration of health with an unstable psycho-emotional state, frequent stress;
- the need for constant use of a diet, rational nutrition.
When patients learn the diagnosis, they often panic. There are many optimal treatment methods that can help you maintain normal health and reduce the number of relapses and exacerbations. A strict diet is not always used; it is used only when the inflammatory process intensifies. The rest of the time, it is enough to follow the doctor’s recommendations to maintain normal health.
Severe/fulminant UC
According to the current definition, UC with more than 6 bowel movements per day, fever, tachycardia and anemia is considered severe. The use of 5 ASA drugs may lead to worsening of colitis and is therefore not recommended. In this case, the mainstay of therapy is intravenous steroids (prednisolone). The optimal dose is 48 mg per day (16 mg every 8 hours or 2 mg per hour infusion), although bolus administration is also possible. Total parenteral nutrition is also indicated. If there is no effect from 7-day therapy, the question arises of surgical treatment - colectomy. Alternatively, cytostatics such as cyclosporine at a dose of 4 mg/kg/day can be used. Within 7 days of treatment, the effect is achieved in 60-80% of patients [9, 10], after which the patient is transferred to oral administration of the drug (6-8 mg/kg/day) with a simultaneous gradual reduction in the dose of steroids.
UC with steroid refractoriness/dependence
In this case, the drugs of choice are Azathioprine (2.5 mg/kg/day) and 6-mercaptopurine (1.5 mg/kg/day). Their use makes it possible to achieve remission and stop using steroids in approximately 2/3 of patients [1,2]. However, the effect of their use occurs after 2-3 months of treatment (the process of reducing the dose of steroids should not begin earlier), and the risk of side effects is high. Therapy with this group of drugs is also indicated for patients with a relapse of UC when the dose of prednisolone is reduced below 15 mg per day, with a relapse within 6 weeks after stopping steroid treatment, and also for patients requiring two or more courses of steroid therapy per year.
Zeposia: safety of ozanimod in the treatment of ulcerative colitis
During the induction phase of treatment for ulcerative colitis, the most common adverse reactions in response to ozanimod were the following: anemia (4.2% of patients versus 5.6% in the placebo group), nasopharyngitis (3.5% versus 1.4%), headache (3.3% vs. 1.9%).
During the maintenance phase, the safety profile was as follows: increased alanine aminotransferase (ALT) levels [4.8% vs. 0.4%; no serious events], headache (3.5% vs. 0.4%).
The pooled analysis of the two stages revealed the following rates of adverse reactions: elevated liver enzymes (11% vs. 2%), headache (5% vs. <1%), upper respiratory tract infections (5% vs. 4%), pyrexia (3% vs. 2%), nausea (3% vs. 2%), arthralgia (3% vs. 1%).
Alternative Methods
There is evidence that smokers have an easier course of UC and require fewer hospitalizations and surgeries for this disease [13]. The use of a nicotine patch (15 mg per day) resulted in a higher rate of remission in patients with proctitis refractory to topical mesalamine therapy than the addition of oral mesalamine at a dose of 2 grams per day [7]. Moreover, the use of nicotine-containing enemas has been shown to be effective in the treatment of distal colitis [18].
The effectiveness of infliximab in patients with Crohn's disease led to attempts to use it in UC. However, there is not yet enough data to allow the use of this drug in UC.
The role of antibiotics in UC remains highly controversial, although there are isolated reports of their successful use in this disease.
Different forms of heparin have been compared with prednisolone in the treatment of severe UC in several studies. The results obtained are contradictory and not very encouraging. So the work, which included 25 patients with severe UC, randomized to heparin infusion or methylprednisolone at a dose of 0.75-1.0 mg per kilogram, gave the following results: on the 10th day of therapy, a positive response was observed in 69% of patients receiving steroids and 0% receiving heparin [14], in addition, in 3 of 12 patients receiving it, rectal bleeding increased. At the same time, the use of low molecular weight heparin in combination with steroid therapy improved the results of treatment of acute ulcerative colitis according to one small study [20].