ARVI is the most common infection on the globe. It is impossible to fully take into account the true incidence. Almost every person experiences ARVI several times (from 4-8 to 15 times or more) a year, mainly in the form of mild and subclinical forms. ARVI is especially common in young children. Children in the first months of life rarely get sick because they are in relative isolation and many of them retain passive immunity received from the mother transplacentally in the form of IgG for 6-10 months. However, children in the first months of life can also suffer from ARVI, especially if they are in close contact with sick people. The reasons for this may be weak transplacental immunity or its complete absence, prematurity, primary forms of immunodeficiency, etc.
ICD-10 code
J00-J06 Acute respiratory infections of the upper respiratory tract
Epidemiology of ARVI
According to statistics, a child can get sick from 1 to 8 times a year. This is due to the fact that the immunity developed in a child’s body against one virus is powerless against another infection. And there are hundreds of viruses that cause ARVI. These are influenza viruses, parainfluenza, adenoviruses, enteroviruses and other microorganisms. And since parents often have to deal with ARVI, they should know as much as possible about this disease, the mechanisms of its development and methods of combating viral infection in childhood.
The highest incidence occurs in children from 2 to 5 years of age, which is usually associated with their visits to child care institutions and a significant increase in the number of contacts. A child attending kindergarten can get ARVI up to 10-15 times during the 1st year, 5-7 times in the 2nd year, and 3-5 times a year in subsequent years. The decrease in incidence is explained by the acquisition of specific immunity as a result of acute respiratory viral infections.
Such a high incidence of ARVI in childhood makes this problem one of the most pressing in pediatrics. Repeated diseases significantly affect the development of the child. They lead to a weakening of the body's defenses, contribute to the formation of chronic foci of infection, cause allergization, interfere with preventive vaccinations, aggravate the premorbid background and delay the physical and psychomotor development of children. In many cases, frequent acute respiratory viral infections are pathogenetically associated with asthmatic bronchitis, bronchial asthma, chronic pyelonephritis, polyarthritis, chronic diseases of the nasopharynx and many other diseases.
Dr. Komarovsky: Children suffer from acute respiratory infections more often than adults - this is the norm, this is the law of life
In the specialized medical literature, the abbreviation BBD is often found. The standard decoding is children who are often ill. Sometimes the expression “frequently and for a long time ill children” is used.
Maturation of the immune system
In clinics, children who are often ill are kept under special dispensary care. But let's look at the situation objectively: is it worth worrying or are these statistics arbitrary? Adults lead a less healthy lifestyle than their children, but suffer from acute respiratory infections much less often. Although our mothers told each of us that in childhood we got sick 10 times a year, and then less and less. This is a law of life: children get sick with acute respiratory infections more often than adults - this is the norm.
A child is born with an immature immune system; it takes time to develop. Babies are surrounded by many people, each of whom is a carrier of a huge number of viruses and bacteria. The child will have to develop immunity to these microorganisms. But nature has done everything to ensure that frequent childhood illnesses are not dangerous. Children's bodies easily cope with acute respiratory infections. And every encounter with the virus is training, formation, and improvement of immunity. How will this all end? A frequently ill child will become an adult and healthy parent.
Tolerate or treat?
No matter how much I urge parents to treat childhood illnesses calmly, not everyone succeeds. Sometimes a mother literally cannot count how many times a year the child has had acute respiratory infections - they simply never end. But parents should know that congenital disorders of the immune system, so-called primary immunodeficiencies, are very rare. They manifest themselves not just as frequent ARVIs, but as severe ARVIs with dangerous bacterial complications that are difficult to treat. Congenital immunodeficiency is a fatal condition and has nothing to do with a two-month runny nose. On the other hand, frequent acute respiratory infections may be a consequence of secondary immunodeficiency - that is, the child was born healthy, but some external factors interfere with the normal development of his immunity.
The main conclusion: if a child who is normal from birth does not recover from illness, it means that he has a conflict with the environment. There are two options for help: try to reconcile the child with the environment with the help of medications, or try to change the environment so that the child is satisfied with it.
Environment
The formation and functioning of a child’s immune system is determined by his lifestyle. If a child often suffers from acute respiratory infections, no pills will solve this problem. Eliminate conflict with the environment, change your lifestyle.
Housing. Organize a child's room where there is no accumulation of dust, everything is subject to wet cleaning and regular ventilation. Night temperature – 18°C, humidity – 50–70%. Soft toys are accumulators of dust, allergens and microorganisms.
Nutrition. Never force a child to eat. It is ideal to feed when he begs for food. Stop snacking, don’t overuse foreign foods, and don’t diversify your diet too much. For sweets - dried fruits, not chocolates.
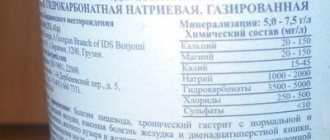
Drink. Optional: mineral water, compotes, fruit drinks, fruit tea. The temperature of the drinks is room temperature.
Cloth. A sufficient minimum, since sweating causes illness more often than hypothermia. The child should not be wearing more items of clothing than the parents.
Walks. Daily, active, preferably before bedtime.
Sport. Outdoor activities are ideal, rather than in confined spaces. Swimming in a pool is not appropriate for CBI.
In summer. The child should take a break from contact with people, from city air, chlorinated water and household chemicals. Holidays “at the seas” have nothing to do with improving your health, since most of the harmful factors remain, plus public catering and worse living conditions. An ideal vacation for a private person: a village, an inflatable pool with well water, a pile of sand nearby, in shorts and barefoot. A dirty naked child who jumps from water to sand, begs for food and breathes fresh air, restores immunity in 3-4 weeks.
Prevention of acute respiratory infections. Frequent illnesses are caused not by cold, but by viruses. We must avoid unnecessary contact with people, wash our hands, maintain local immunity, and vaccinate all family members against the flu.
Treatment of ARVI
Treating ARVI does not mean giving medications, but means creating conditions so that the child’s body can cope with the virus as quickly as possible and with minimal losses. It is necessary to ensure optimal temperature and humidity, dress warmly, do not overfeed, and actively water. Saline drops in the nose and antipyretic medicine if necessary are enough. Any active treatment prevents the formation of immunity. The drug should be used only when it is clearly impossible to do without it. This is especially true for antibacterial therapy.
Actions after recovery
It is important to remember: improvement in condition and normalization of temperature does not indicate that immunity has been restored. The next day after the child’s condition improves, he goes to a group where he encounters a new virus, and a new disease will begin in a weakened body. It will be more severe than the previous one and will require the use of medications.
When it gets better, you need to live a normal life for another week - walks, “working up” your appetite, healthy sleep, restoration of the mucous membranes. Antibodies to the virus are produced no earlier than the fifth day of illness. Therefore, you can resume visiting children’s groups no earlier than the sixth day after the onset of ARVI, regardless of its severity.
There are no non-kindergarten children
When the phrase “I wasn’t sick until I was three” is said, it means we have an absolutely normal child. We went to kindergarten, the environment changed - illnesses began. We must acknowledge the fact that it is impossible to start actively communicating with children and not get sick. Constant illness means either you are in a hurry to return to your children after illness, or something is fundamentally wrong in the kindergarten itself.
Even very frequent acute respiratory infections with proper treatment do not affect the child’s health.
But if every sneeze is a reason to prescribe a dozen syrups, tablets and antibiotics, a reason for a thorough examination and consultation of a dozen specialists, such acute respiratory infections are a clear and obvious evil. If a child suffers from acute respiratory infections often, even very often, but recovers not with the help of medications, but naturally, then let him be sick, let him go to kindergarten. Published: September 26, 2016
Causes of ARVI in children
Factors contributing to the development of ARVI follow the child everywhere. These reasons include:
- hypothermia, drafts, wet shoes;
- communication with other children with ARVI;
- sudden changes in weather, off-season (autumn-winter, winter-spring);
- decrease in the body's defenses;
- hypovitaminosis, anemia, weakened body;
- decreased physical activity of the child, physical inactivity;
- improper hardening of the body.
All these are factors that weaken the body and contribute to the unhindered spread of the virus.
The reasons for frequent ARVI in children are the high sensitivity of the child’s body at any age, including a newborn baby. A child's frequent acute respiratory viral infections begin from the moment he enters a nursery, kindergarten or school. Diseases can be repeated in succession. This happens because immune defense after a viral infection is developed from one type of virus. The penetration of a new virus into the body provokes a new disease, even if a short amount of time has passed since the previous one.
How long does ARVI last in a child?
How long can a baby be contagious and how long does ARVI last in a child?
As a rule, the more time has passed since the first symptoms appeared, the less likely it is that the child is contagious. The period of time when a sick person is able to infect others usually begins from the appearance of the first symptoms of the disease or simultaneously with them. In some cases, the baby may still look “healthy” outwardly, but the disease process may already have begun. This depends on many factors, including the strength of the child’s immunity.
The initial moment of the incubation period (when the virus has already penetrated the child’s body, but the disease has not yet manifested itself “in all its glory”) is considered to be the moment of communication with an already infectious patient. Such a moment could be contact with a sick child in kindergarten, or an accidentally caught “sneeze” on a trolleybus. The final stage of the incubation period ends with the appearance of the first signs of the disease (when complaints appear).
Laboratory tests can already indicate the presence of the virus in the body during the incubation period.
The incubation period of ARVI in children can last from several hours to 2 weeks. This applies to pathogens such as rhinovirus, influenza virus, parainfluenza, parapertussis, adenovirus, reovirus, and respiratory syncytial virus.
The period during which a child is contagious can begin 1-2 days before the first signs of the disease appear.
How long does ARVI last in a child? If you count from the moment the first symptoms appear, the period of illness can last up to 10 days (on average a week). Moreover, depending on the type of virus, the child may continue to remain infectious for another 3 weeks after recovery (disappearance of symptoms).
What to do if your child has a low temperature?
If parents record a short-term low temperature, then this is not a reason for great concern. But if it is observed for more than one or two days, then you need to pay attention to this and show the child to a pediatrician (pediatrician).
Pediatrician. Assess the child’s general condition and prescribe primary examinations (ECG, general and biochemical blood tests). If the cause of a child’s low body temperature is a decrease in immunity, fatigue, or the consequences of common diseases, then the doctor will adjust the diet and diet, general daily routine, and physical activity. But if the pediatrician suspects hidden diseases, he will refer you for examination to pediatric specialists.
Medical specialists. First of all, a pediatric neurologist, pediatric endocrinologist, functional diagnostics doctor, gastroenterologist, oncologist. Additional tests may be required, such as a blood test for hormones, and instrumental studies (ultrasound).
In case of prolonged low temperature in a child, only a comprehensive examination can establish the reasons for this and allow, based on the diagnosis, to prescribe correct and timely treatment.
Symptoms of ARVI in children
Whatever type of virus is caused by ARVI, the classic form of the disease presents some common symptoms:
- “general infectious” syndrome (the child is shivering, there may be pain in the muscles, in the head, there is weakness, the temperature rises, the submandibular lymph nodes are enlarged);
- damage to the respiratory system (nasal congestion, runny nose, sore throat, dry cough or with sputum production);
- damage to the mucous membranes (soreness and redness in the eye area, lacrimation, conjunctivitis).
The first signs of ARVI in a child are often characterized by a sudden onset with a clearly defined “general infectious” syndrome. With parainfluenza or adenovirus, the first signs are damage to the respiratory system (throat, nasopharynx), as well as redness and itching of the conjunctiva of the eye.
Of course, it would be easier for both parents and doctors if the course of ARVI in children was always classic. However, a child’s body is a very complex system, and its response to the penetration of a particular virus cannot be predicted one hundred percent. Each organism is individual, so the course of ARVI can be subtle, asymptomatic, atypical, or even extremely severe.
Since parents are unlikely to be able to guess and predict the course of the disease, it is necessary to know about conditions in which you will have to consult a doctor in the most urgent manner.
Symptoms of ARVI in children that require urgent medical attention:
- Temperature readings have exceeded 38°C and have little or no response to antipyretic medications.
- The child's consciousness is impaired, he is confused, indifferent, and may faint.
- The child complains of a severe headache, as well as the inability to turn his neck or bend forward.
- Spider veins and rashes appear on the skin.
- Chest pain appears, the child begins to choke, it is difficult for him to breathe.
- Multi-colored sputum appears (green, brown or pink).
- Swelling appears on the body.
- Convulsions appear.
You should not self-medicate, especially when it comes to your child. Also pay attention to the baby’s other organs and systems so as not to miss the onset of inflammation.
Temperature during ARVI in children
Children are quite sensitive to increases in body temperature: excessively high temperatures contribute to the appearance of seizures in a child. Because of this, the temperature should not be allowed to rise above 38-38.5°C.
There is no need to bring the temperature down to 38°C, since there is no need to interfere with the body doing its job - fighting the penetration of the virus. This may cause complications. What to do:
- do not panic;
- Monitor the child’s condition - usually after 3-4 days the temperature should stabilize.
Prolonged acute respiratory viral infection in a child with a persistent temperature may indicate the addition of a bacterial infection. It also happens that the temperature readings dropped after a viral infection, the baby seemed to be on the mend, but after a few days he became worse again and developed a fever. In such a situation, you should not hesitate to call a doctor.
In the classic course of ARVI, the temperature can last no more than 2-3 days, a maximum of five days. During this time, the body must overcome the virus by developing its own antibodies to it. Important: you should not deliberately lower the temperature to normal; you can only lower it so that the body continues to fight the infection.
Cough due to ARVI in children
Cough during ARVI in children is a fairly common symptom. It is usually present against a background of fever, runny nose and other signs of illness. With the onset of the disease, a dry cough (without sputum production) is observed. Doctors call this cough unproductive: it is difficult for the child to tolerate, can disturb the peace of his sleep, and negatively affect his appetite.
In the classic course of ARVI, after 3-4 days the cough enters the productive stage - sputum appears. But it should be borne in mind that not all children know how to cough it up. For this reason, the child needs help: regular chest massage, light exercises, and in case of a coughing attack, the baby should be placed in an upright position.
As a rule, cough during viral infections lasts up to 15-20 days, but if its duration exceeds three weeks, then a chronic cough can be suspected. In such cases, competent consultation with a pediatric pulmonologist and allergist, as well as the prescription of complex therapy, is simply necessary.
Vomiting in a child with ARVI
Vomiting in a child with ARVI can occur simultaneously with the appearance of high fever and cough. Sputum that is difficult to clear, dense and viscous, irritates the respiratory system and provokes bouts of painful coughing in the child. The gag reflex is triggered as a result of the transition of the excitatory signal from the cough centers to the vomiting centers. In some cases, vomiting may occur due to the accumulation of a large amount of mucous secretions in the nasopharynx, but in this case, vomiting occurs without coughing. Most often, vomiting due to coughing is not profuse and does not bring visible relief to the baby.
It is important to distinguish when vomiting is associated with the simultaneous excitation of the cough and gag reflex, and when vomiting may be a sign of poisoning or a disease of the gastrointestinal tract. Therefore, it is imperative to show the child to the doctor, otherwise this may provoke the appearance of unwanted and sometimes serious complications.
Rash due to ARVI in a child
If a rash appears due to ARVI in a child, this is a direct reason to consult a doctor. There are several possible reasons for the appearance of rashes during illness:
- intolerance to any of the medications taken by the baby;
- allergic reaction to foods that parents usually give to a sick child (raspberries, oranges, lemons, garlic, ginger, etc.);
- high temperature, which increases vascular permeability - in such cases, the rash resembles hemorrhages of various sizes on the skin.
There are also more serious causes of the rash. For example, this is the addition of a meningococcal infection: such a rash is usually accompanied by hyperthermia and vomiting. In any of the options, if a rash is detected on the child’s body, all measures should be taken to deliver the baby to the infectious diseases department as soon as possible. You can simply call an ambulance and describe the symptoms of the disease. In this case, you cannot hesitate.
Stomach pain due to ARVI in a child
Quite often, parents are faced with a situation where their child has a stomach ache due to ARVI. The pain is most often colicky and localized in the projection area of the large intestine. Doctors can explain this symptom as a combined reaction of the lymphatic system of the intestine and appendix. For the same reason, ARVI can be complicated by an attack of acute appendicitis. In such a situation, the most competent action of parents may be to call a doctor at home, and if the pain in the tummy area increases, then they will have to call the emergency room.
A large number of acute respiratory viral infections along with abdominal pain can also be accompanied by diarrhea. Diarrhea during ARVI in a child is caused by cramping spasms in the intestines - the child’s body’s reaction to the disease. However, most often diarrhea and abdominal pain are provoked by medications that the child is forced to take. For example, if a baby is prescribed antibiotics or antiviral drugs, this can gradually lead to disruption of the intestinal microflora, or may manifest itself as a hypersensitivity reaction of the digestive system to certain types of medications. In one case or another, consultation with a doctor is mandatory.
Conjunctivitis due to ARVI in a child
Unfortunately, conjunctivitis during ARVI in a child occurs in almost all cases of the disease, especially when attacked by an adenoviral infection. Signs of conjunctivitis become noticeable immediately. Initially, the viral infection that provokes ARVI affects one eye, but after 1-2 days the other eye is also affected. Both eyes of the child become red, itchy, and there is a feeling of “sand” in the eyes. The baby squints, rubs his eyelids, and cries constantly. The eyes may become crusty, and light discharge may collect in the corners.
This conjunctivitis gradually goes away on its own as the child recovers from ARVI. However, special children's medicines - antiviral eye ointment or drops, which can be easily purchased at pharmacies, can help alleviate the baby's condition and eliminate itching and discharge from the eyes more quickly.
True, in some cases, conjunctivitis can be the result of an allergic reaction in a child. In this condition, the baby not only develops watery eyes and redness of the eyes, but also the lower eyelids become swollen. It is typical that allergies affect both eyes at the same time. If this happens, urgent consultation with a doctor is necessary, identification and elimination of contact with a potential allergen, and prescription of antihistamine eye drops and medications.
Features of the course of ARVI in children
Children at different ages may react differently to the appearance of signs of ARVI.
- ARVI in an infant can manifest itself with symptoms such as restlessness of the baby, poor sleep, loss of appetite; defecation disorder, excessive tearfulness and moodiness. Such changes in the behavior of an infant should arouse suspicion in the mother, since the infant cannot explain his well-being in words.
- ARVI in a one-month-old baby can occur with difficulty in nasal breathing, since the baby does not yet know how to breathe through the mouth. How to suspect that a child has a stuffy nose? The baby becomes restless when sucking, often refuses to eat and pushes away the breast or bottle. In such cases, you should definitely clean the baby’s nasal passages.
- ARVI in a 2-month-old child can typically manifest itself as shortness of breath with prolonged wheezing exhalation - this sign is often called asthmatic syndrome. In this case, symptoms of intoxication are expressed: gray or cyanotic skin, lethargy, apathy, fever.
- ARVI in a 3-month-old child often occurs with damage to the respiratory system, which, with unqualified help, can be complicated by bronchitis or pneumonia. Therefore, it is very important to pay attention to the child’s difficulty in swallowing and nasal breathing and regularly measure the temperature. It is extremely undesirable to stop breastfeeding during this period, since mother’s milk in this case will be the best medicine for the baby.
- ARVI in a 4-month-old child is accompanied by damage to the mucous membrane of the nasopharynx and bronchi, which manifests itself in the form of a runny nose and cough. You can observe an increase in the submandibular or parotid lymph nodes and spleen. Conjunctivitis and keratoconjunctivitis often develop, which is expressed in redness of the eyes and continuous lacrimation.
- ARVI in children under one year of age can be complicated by croup - a condition when the larynx becomes inflamed and swollen, namely the area that is located directly under the vocal cords. This condition is explained by the fact that in small children this area contains a large amount of loose fiber, which swells easily. In this case, the laryngeal lumen is not large enough. Croup most often develops at night, so parents should pay attention to a sudden “barking” cough, heavy breathing, asthma attacks, anxiety, and bluish lips in the child. If such signs are observed, it is necessary to urgently call an ambulance.
- ARVI in a child of 6 months is the period when the baby has already been introduced or is being introduced to complementary foods. Often at six months of age, a viral infection is accompanied, in addition to damage to the respiratory system, by involving the digestive system in the process. This may manifest itself as signs of acute gastritis or enteritis: abdominal pain and stool upset.
- ARVI in a 1-year-old child can recur from 1 to 8 times a year, depending on immunity. Starting at this age, it is very important to begin hardening procedures and strengthen the baby’s immune defense so that his body can resist numerous viruses and bacteria. It is especially important to protect the baby in the autumn-winter and winter-spring periods.
- ARVI in a 2-year-old child is often accompanied by laryngitis (inflammation of the larynx), tracheitis (inflammation of the trachea - breathing tube), or a combination of these diseases. Signs of such a lesion are a hoarse voice, a dry, obsessive cough. Of course, a 2-year-old baby cannot yet coherently express his complaints. Therefore, parents should carefully monitor the child’s condition. If you experience difficulty breathing, retraction of the intercostal spaces, or swelling of the wings of the nose, you must urgently call an ambulance.
- ARVI in a 3-year-old child usually begins with a rise in temperature in the late afternoon. Pain in the head appears, the baby feels apathetic, tired, lethargic. Most often, the disease appears during the epidemic season, so making a diagnosis is not difficult. The severity of the condition determines the child’s well-being.
If you notice any uncharacteristic or suspicious symptoms in your child, be sure to call an ambulance. Don’t be afraid to bother the doctor again: the main thing is your baby’s health.
Rotavirus gastroenteritis
This is an acute viral disease affecting the gastrointestinal tract. Human rotavirus causes the majority of cases of gastroenteritis reported worldwide. During the first three years of life, most children manage to get sick from rotavirus infection, as evidenced by the frequent detection of specific antibodies in the blood of healthy children.
Causes of diarrhea
When it enters the gastrointestinal tract, rotavirus penetrates the cells of the small intestine, where it multiplies. This process ends with changes and partial destruction of the epithelium of the villi, which are responsible for digestion and especially for the absorption of nutrients from the intestines into the blood. These changes cause diarrhea.
Source of infection
Currently, several types of human rotaviruses are known. All of them remain viable for a long time in feces and are relatively resistant to traditional household disinfectants.
The source of infection is a sick person or a carrier of the virus. Patients in the acute period of the disease are especially dangerous. Isolation of the virus in feces begins from the moment the first clinical symptoms appear and reaches a maximum on days 3-5 from the onset of the disease.
Gradually, the concentration of the agent in feces quickly decreases and after the 7-10th day of illness, in most patients its excretion stops.
Most often, rotavirus is transmitted through household contact, that is, through infected toys, dishes, household items, clothing, underwear, etc. Interestingly, the virus can be released by apparently healthy people who have been in contact with a sick patient (asymptomatic infection).
Course of the disease
The latent (incubation) period is 1-5 days.
The disease begins acutely, with vomiting, abdominal pain, stool upset and a rise in body temperature to 37.5-38 °C, less often to 39 °C. At first, the vomit is copious, mixed with food, then becomes watery.
The child experiences nausea and a decrease in appetite. Bowel movements usually become more frequent up to 5-15 times a day. The stool is watery, profuse, yellow or yellow-green in color, foamy, with a pungent odor. Older children complain of abdominal pain, mainly in the upper part and around the navel.
The urge to defecate occurs suddenly, is accompanied by rumbling in the stomach, and ends with a loud discharge of gas and splashing stool. After defecation, patients experience relief.
The mucous membrane of the soft palate, uvula, palatine arches is partially red and slightly swollen. In severe cases, there is severe weakness, headache, dizziness, chills, convulsions and even loss of consciousness.
An increase in body temperature and symptoms of intoxication are observed during the first 2-3 days. The duration of diarrhea due to rotavirus infection is from 3 to 6 days. The total duration of the disease is about 7-10 days. Sometimes a longer course is possible.
Diagnostics
The diagnosis is confirmed by the detection of rotavirus antigen in feces by PCR, as well as antibodies in the blood, for example, by ELISA (enzyme-linked immunosorbent assay).
Prevention
Aimed at early identification of patients and their timely isolation from healthy people. It is also important to ensure compliance with the sanitary and hygienic regime in the family and child care institutions. To prevent infection within a large group, it is necessary to separate its members as much as possible, wear respiratory masks, use disinfectant solutions, etc.
Repeated ARVI in a child
Repeated ARVI in a child is not uncommon, since children are usually very susceptible to viral infection. Babies are prone to contracting the virus from the first weeks of life, but in the first three months they do not get sick as often as at an older age. The tendency to the disease is especially evident at the age of six months to 3 years, then the susceptibility decreases somewhat, although this may depend on the individual immunity of the body.
Why do repeated acute respiratory viral infections occur? The fact is that immunity has specificity in relation to certain types and even types of viral infection. Such immunity is not stable or durable. And in combination with a large number of varieties of the virus, it creates a high percentage of the likelihood of recurrent diseases.
ARVI in a child can occur as a single case, or as a result of a mass epidemic, which often happens in children's groups. That is why the child’s morbidity rate increases, as a rule, with the start of attending kindergarten or other preschool or school institutions.
Where does it hurt?
Chest pain
What's troubling?
Cough Shortness of breath
Complications of ARVI in children
According to statistics, at least 15% of all ARVI diseases in childhood leave behind complications for other organs and systems of the body. For this reason, we should not forget that in children, ARVI can occur with an elevated temperature for no more than five days. A longer increase in temperature above 38°C may indicate the appearance of complications or the addition of another disease. Sometimes the temperature seems to drop, but after 1-3 days it rises again: symptoms of intoxication appear, such as tearfulness, pallor, lethargy, and increased sweating. The child refuses to eat and drink and becomes indifferent to what is happening. What can be the complications of ARVI in children?
- A cough after an acute respiratory viral infection in a child in some cases can mean the disease progresses to bronchitis or even pneumonia - the viral infection gradually moves down the respiratory tract. First, there may be a clinical picture of laryngitis (dry cough, hoarse voice), then tracheitis (painful cough, vocal functions are restored), and subsequently bronchitis. The main sign of bronchitis is a cough. At first it is dry and rough, and gradually phlegm begins to form and cough up. Difficulty in breathing occurs, the temperature rises again, increased sweating, and fatigue. If a child has frequent and heavy breathing (sometimes the baby seems to “groan”), then bronchiolitis or pneumonia can be suspected. Consultation with a doctor is required.
- A rash in a child after an acute respiratory viral infection can be due to several reasons. For example, this may be the addition of diseases such as rubella, measles, herpes (infantile roseola), enterovirus infection, scarlet fever, etc. Or there may be an allergic reaction to drugs, for example, antibiotics. The exact cause of the rash must be determined by a doctor.
- Arthritis after ARVI in children may appear after a protracted illness. This type of arthritis is called “reactive” arthritis. Symptoms of reactive arthritis may appear several days or even weeks after recovery. Usually pain occurs in the joint (usually in the morning). This could be the hip joint, knee joint, ankle joint, etc. The child has difficulty getting out of bed, limps when walking, and complains of severe pain. A pediatric rheumatologist can diagnose the disease and begin treatment based on an examination and the results of some tests.
Also, complications of ARVI can be sinusitis (inflammatory process in the paranasal sinuses) or otitis media. Such diseases can be suspected by constant nasal congestion accompanied by a headache, or by shooting pain in the ear along with decreased hearing and a feeling of stuffiness.
What is low body temperature in a child?
It is widely believed that the normal body temperature of a healthy child is 36.6. In fact, it depends on a lot of factors: the sex and age of the child, the degree of his physical activity, the composition and amount of drink and food consumed, methods of measurement, time of day (morning, afternoon, evening), etc. On average, it is believed that in healthy children the temperature is normally in the range of 36.5-37.5 degrees. But pediatricians are more focused on the upper permissible temperature limits, which depend on age. Namely, if the measurement is carried out in the armpit (the most common method), then the limits are as follows: newborns - 36.8, from 6 months to 3 years - 37.7 and over 6 years - 37.0.
Then what is a low temperature in a child? Acceptable temperatures are in the range of 36.0-36.5 degrees. But the child’s body temperature should not be lower than 36 degrees, and the range from 35.4-35.6 is unacceptable for children. If, for example, a child has a low temperature of 36, then they usually speak of a low temperature. If a child has a very low body temperature (about or below 35 degrees), then they speak of hypothermia. Sometimes the term hypothermia combines the conditions of a child’s actual low temperature and very low temperature.
It is also important for how long the temperature is lowered. A short-term drop in temperature can be caused by simple hypothermia. And it’s a completely different matter if a child has a low temperature for a long time, which may be associated with hidden diseases. Constant very low body temperature in a child is extremely rare, but low body temperature in an infant is not uncommon.
Diagnosis of ARVI in children
The main task of tests performed to diagnose ARVI in children is to determine the type of pathogen. Depending on this, a further treatment regimen will be prescribed.
The most common tests for ARVI in children are a general blood test, a general urinalysis, and immunological studies to detect antibodies to a viral infection.
What indicators usually indicate ARVI?
General blood analysis:
- red blood cells - normal or increased due to a lack of fluid in the body;
- hematocrit - normal or increased (with fever);
- leukocytes - the lower limit of normal or decreased, which indicates a viral etiology of the disease;
- leukocyte formula - predominance of lymphocytes, slight increase in monocytes;
- eosinophils - decrease in number or complete disappearance;
- neutrophils - decreased number;
- ESR increases during ARVI in children, but this indicator is nonspecific for a viral infection.
General urine analysis:
- the changes are not specific, sometimes there is a small amount of protein in the urine, which disappears after recovery;
- possible, but not at all necessary - slight microhematuria.
In rare cases, ketone bodies—acetone and acetoacetic acid—chemical complexes that form in the liver when digesting food entering the digestive tract can be found in the blood or urine. Acetone during ARVI in children can appear in different concentrations, and since this substance is initially toxic, its presence in large quantities can cause signs of poisoning in a child (in particular, vomiting, as well as the smell of acetone from the mouth or from urinary secretions). The determination and treatment of acetone in the blood or urine should be carried out exclusively by a medical specialist.
Immunology is an analysis for immunoglobulins M (released already at the initial stages of the disease). This test is taken twice - at the first symptoms of ARVI and a week later. Such a study allows you to accurately determine the pathogen. However, the immunological method is not always used, but only in severe and protracted cases of the disease.
What needs to be examined?
Bronchi Trachea Larynx
How to examine?
X-ray of the lungs Examination of the respiratory organs (lungs) Bronchoscopy
What tests are needed?
Sputum analysis
Who to contact?
Infectious Diseases Pediatrician
Treatment of ARVI in children
Children with mild to moderate forms of ARVI can be treated at home. Hospitalization is required only in the following cases:
- in severe forms of the disease, or in the presence of complications (pneumonia, croup, etc.);
- for a child under 1 year old, or from 1 to 3 years old;
- under unsatisfactory epidemiological and material conditions.
The standard treatment for ARVI in children provides, first of all, for the removal of intoxication from the body. This is achieved by drinking large amounts of warm drinks, complex multivitamins, and in more severe cases, intravenous administration of glucose and blood substitutes. At high temperatures, antipyretic drugs can be used in the form of tablets or rectal suppositories, and in severe cases - in the form of intramuscular injections.
During the period of fever, the child is prescribed bed rest. In the absence of complications, antibiotics and sulfonamide drugs are usually not used, but in some cases they are still prescribed to small children, since it is very difficult to recognize a complication in an infant.
The protocol for the treatment of ARVI in children with complications includes the prescription of bronchodilators (for pneumonia or bronchitis). Antibiotics are used with caution, taking into account the child's allergic inclination. For laryngeal stenosis, sedatives and antispasmodics are used, and in severe cases, an injection of hydrocortisone is administered.
Modern treatment of ARVI in children involves the prescription of drugs aimed at eliminating the main symptoms of the disease. What drugs are these:
- antitussives in the form of syrups, chewable or regular tablets;
- warming creams or balms based on natural ingredients that are rubbed into the skin of the chest;
- other warming procedures (mustard plasters or compresses) as indicated;
- vitamin preparations to strengthen immune forces.
We will talk more about drugs for ARVI below.
Drugs for the treatment of ARVI in children
All antivirus products are divided into 4 categories:
- homeopathic antiviral remedies;
- purely antiviral medications;
- interferons and interferon stimulators;
- immune stimulating agents.
Let's look at all these categories separately.
- Homeopathy for ARVI in children. The most commonly prescribed suppositories from this category of medications are Viburkol, Oscilococcinum and Aflubin, slightly less common are EDAS-103 (903) or Gripp-Heel. Homeopathic specialists claim that the listed homeopathic remedies stimulate the protective function of the child’s body, and often this is true, although the pharmacodynamics of these drugs have been practically unstudied. As a rule, homeopathic remedies have an effect already at the first doses of the drug.
- Specific antiviral agents. In pediatrics, antiviral agents such as Arbidol, Rimantadine, Ribavirin and Tamiflu are more often used (in some cases also Acyclovir, according to indications). The listed drugs inhibit the entry of the virus into cellular structures, block the reproduction of the virus, however, they have a different spectrum of activity and are not intended for all children's age groups.
- Interferon drugs and their stimulants are perhaps the most popular group of antiviral drugs. For example, Viferon for ARVI in children suppresses the development of the virus and destroys it in 1-3 days. Interferons are able to rid the body of a viral infection, both during the incubation period and from any period of the disease. In addition to the injection of interferons, the most interesting are Viferon suppositories, Kipferon suppositories and Grippferon nasal drops. Perhaps the only contraindication to the use of these products may be the baby’s allergic tendency to the ingredients of medications, especially to the components of candles - cocoa butter or confectionery fat. By the way, medications that activate the production of interferons (Amiksin, Neovir, Cycloferon) are recommended to be used only for prevention, but not for the treatment of ARVI, due to the slow action of such drugs.
- Immunostimulating drugs - Isoprenosine, Riboxin, Immunal, Imudon, Methyluracil, Bronchomunal, IRS-19, Ribomunil, etc. One of the most popular medications listed, Isoprinosine for ARVI in children is used more as a prophylaxis, however, like other immunostimulants. The reason is that the effectiveness of the action of immunostimulants is observed only after 14-20 days from the start of immunostimulating treatment. These drugs can also be used to restore the body after recovery.
As is known, antibiotics are not prescribed for ARVI in children with the classic course of the disease, since they have nothing to do with a viral infection. Antibiotic therapy is used only in case of complications or when they are suspected: ampicillin derivatives are most often prescribed.
CHILD WITH FEVER
Fever is the most common symptom of illness in children: every child suffers from a febrile illness at least once a year. But they also represent the most common reason for the use of medications: almost all children with fever receive antipyretics even at a low temperature - below 38°. This is facilitated by the idea that parents still have about the extreme danger of high temperature. As, indeed, is the doctor’s desire to alleviate the discomfort associated with temperature, or at least prescribe treatment, the effect of which will be obvious.
Mass consumption of antipyretics imposes special requirements on their safety due to the possible development of complications in children. The fight against elevated temperature is an important element in the treatment of many diseases, but it cannot be considered an end in itself: after all, by lowering the temperature, in most cases we do not affect the course and severity of the disease. Therefore, those doctors and parents who strive at all costs, by any means, to reduce the temperature of a sick child and keep it at normal values are wrong: such behavior indicates their poor knowledge of the causes and role of fever.
First of all, about the normal body temperature of the child. It is not 36.6°, as many believe, but fluctuates during the day by 0.5°, in some children - by 1.0°, increasing in the evening. When measuring the temperature in the armpit, a value of 36.5–37.5° can be considered normal: the maximum temperature (rectal) averages 37.6°, exceeding 37.8° in half of the children [1]. Axillary temperature is 0.5–0.6° lower than rectal temperature, but there is no exact conversion formula; It is important to remember that a temperature above 38°, wherever it is measured, in most children (including the first months of life) corresponds to febrile temperature, and the difference in tenths of a degree does not matter much. But there is no reason to worry if a child’s temperature (in the absence of other symptoms) “jumps” to 37.3–37.5° in the evening; By the way, the temperature decreases somewhat if you let the child cool down before measuring.
Regulation of body temperature is achieved through the balance of heat production and heat transfer. The body generates heat by burning (oxidizing) carbohydrates and fats in tissues, especially when muscles work. Heat is lost as the skin cools; its losses increase with the dilation of skin vessels and evaporation of sweat. All these processes are regulated by the hypothalamic thermoregulatory center, which determines the amount of heat production and heat transfer.
Fever is a consequence of the action of endogenous pyrogens on the thermoregulatory center: cytokines, which are also involved in immunological reactions. These are interleukins IL-1 and IL-6, tumor necrosis factor (TNF), ciliary neurotropic factor (CNTF) and interferon-a (IF-a). Increased synthesis of cytokines occurs under the influence of products secreted by microorganisms, as well as by body cells when they are infected with viruses, during inflammation, and tissue breakdown. Cytokines stimulate the production of prostaglandin E2, which, as it were, moves the setting of the “central thermostat” to a higher level, so that normal body temperature is determined by it as lower. An increase in heat production due to increased muscle activity and trembling is accompanied by a decrease in heat transfer due to constriction of skin blood vessels. We perceive shivering and a feeling of cold (chills) as a “cold”; upon reaching a new temperature level, heat transfer increases (feeling of heat). Prostaglandin E2 can cause the muscle and joint pain we experience as aching during an acute infection, and IL-1 causes the drowsiness often seen in a child with a fever.
The biological significance of fever is protection against infection: animal models have shown an increase in infection mortality when fever is suppressed, and a similar effect has been described in humans [2]. Under the influence of moderate fever, the synthesis of interferons and TNF increases, the bactericidal capacity of polynuclear cells and the reaction of lymphocytes to mitogen increases, and the level of iron and zinc in the blood decreases. “Feverish” cytokines increase the synthesis of proteins in the acute phase of inflammation and stimulate leukocytosis. In general, the effect of temperature stimulates the type 1 T-helper immune response, which is necessary for adequate production of IgG antibodies and memory cells. Many microbes and viruses have a reduced ability to reproduce when the temperature rises.
Antipyretics lower the temperature without affecting the cause that caused it. In case of infections, they only transfer the setting of the “central thermostat” to a lower level, without reducing the total duration of the febrile period; but at the same time, the period of virus isolation is clearly prolonged, in particular in acute respiratory infections [3–5]. A direct inhibitory effect of these drugs on TNF-a production and anti-infective defense has been shown [6].
These and other similar data make us cautious about suppressing fever in infectious diseases; One should also take into account the fact that suppression of the production of interferon and IL-2 reduces the strength of the humoral immune response. This makes it plausible to assume that frequent acute respiratory viral infections in children are related to the widespread use of antipyretic drugs in our time; This may also be responsible for the upward trend in allergic diseases.
Another danger arises when using antipyretics. In most acute respiratory viral infections, the temperature lasts only 2–3 days, while in bacterial acute respiratory infections (otitis media, pneumonia) it lasts 3–4 days or more, which is often the only indication for prescribing antibiotics. The use of antipyretic drugs in such patients, especially the “course”, with suppression of temperature, creates the illusion of well-being, and by the end of the week it is necessary to take “heroic measures” to save the child’s life as a result of an advanced process. Therefore, to reduce the temperature you need to have sufficient reasons, and in any case you cannot try to prevent it from rising again.
Of course, closer to 40.0°, the protective functions of fever turn into the exact opposite: metabolism and O2 consumption increase, fluid loss increases, and additional stress is created on the heart and lungs. A normally developing child copes with this easily, experiencing only discomfort, but in patients with chronic pathology, fever can cause a deterioration in the condition. In particular, in children with damage to the central nervous system, fever contributes to the development of cerebral edema and seizures. Fever is more dangerous for children 0–3 months old. And yet, the dangers associated with an increase in temperature are largely exaggerated; in most infections, its maximum values do not reach 39.5–40.0°C, and there is no threat of developing persistent health disorders.
A study of the practice of using antipyretics showed that, for example, for ARVI, they are prescribed to 95% of sick children, even at temperatures below 38° (93%) [7]. Familiarizing pediatricians with modern approaches to this problem makes it possible to reduce the use of these drugs by 2–4 times.
The main febrile syndromes in children are associated with infection and are usually accompanied by quite distinct symptoms that allow at least a presumptive diagnosis to be made right at the patient’s bedside. The following list shows the main symptoms most often associated with high fever in children and the most common causes of their occurrence.
- Fever + rash in the early stages: scarlet fever, rubella, meningococcemia, allergic rash to an antipyretic drug.
- Fever + catarrhal syndrome from the respiratory system: ARVI - rhinitis, pharyngitis, bronchitis, possibly also bacterial inflammation of the middle ear, sinusitis, pneumonia.
- Fever + acute tonsillitis (tonsillitis): viral tonsillitis, infectious mononucleosis (Epstein-Barr virus infection), streptococcal tonsillitis or scarlet fever.
- Fever + difficulty breathing: laryngitis, croup (inspiratory shortness of breath), bronchiolitis, obstructive bronchitis, asthma attack due to ARVI (expiratory shortness of breath), severe, complicated pneumonia (groaning, groaning breathing, pain when breathing).
- Fever + cerebral symptoms: febrile convulsions (convulsive syndrome), meningitis (headache, vomiting, stiff neck), encephalitis (disorders of consciousness, focal symptoms).
- Fever + diarrhea: acute intestinal infection (usually rotavirus).
- Fever accompanied by abdominal pain and vomiting: appendicitis, urinary tract infection.
- Fever + dysuric symptoms: urinary tract infection (usually cystitis).
- Fever + joint damage: rheumatism, arthritis, urticaria.
- Fever + symptoms of very severe illness (“toxic” or “septic”); the condition requires immediate hospitalization and emergency intensive care, along with deciphering the diagnosis. These symptoms include:
- a sharp violation of the general condition;
- drowsiness (sleeping longer than usual or at unusual times);
- irritability (screaming even when touched);
- disturbance of consciousness;
- reluctance to take liquids;
- hypo- or hyperventilation;
- peripheral cyanosis.
With syndromes 1–9, diagnostic difficulties may, of course, occur, but the most important thing is to make an assumption about the most likely etiology of the process. Fever in a child 0–3 months of age may be a manifestation of a severe infection; in these cases, hospital observation is usually indicated. Long-term (more than 2 weeks) fever of unknown cause requires examination for long-term infection (sepsis, yersiniosis), connective tissue disease, immunodeficiency, and malignant pathology.
If a bacterial disease is suspected, an antibiotic should be prescribed, if possible without antipyretics, since they can mask the lack of effect of antibacterial treatment.
Fever without a visible source of infection (FWF) . Almost every child is examined for a febrile illness in the first 3 years of life. Of these, every fifth person does not reveal signs of a specific disease during examination [8]. Currently, such fever is considered as a separate diagnostic category. This refers to an acute illness manifested only by febrile fever in the absence of symptoms that would indicate a specific disease or source of infection. LBI criteria are a temperature above 39° in a child aged 3 months to 3 years and above 38° in a child 0–2 months of age in the absence of the above “toxic” or “septic” symptoms of a very serious disease at the time of the first examination.
Thus, the group of LBI includes children in whom febrile fever is detected against the background of a slightly disturbed general condition. The point of identifying the group of infectious diseases is that, along with non-life-threatening infections (enteroviral, herpetic types 6 and 7, etc.), it includes many cases of influenza, as well as latent (occult) bacteremia, i.e. e. the initial phase of a severe bacterial infection (SBI) - pneumonia, meningitis, pyelonephritis, osteomyelitis, sepsis, in which clinical symptoms may not occur at an early stage, providing a real opportunity to prescribe an antibiotic, preventing its progression.
The causative agent of occult bacteremia in 80% of cases is pneumococcus, less often - H. influenzae type b, meningococcus, salmonella. In children 0–2 months, Escherichia coli, Klebsiella, group B streptococci, Enterobacteriaceae, and Enterococci predominate. The frequency of occult bacteremia in children 3–36 months with LBI is 3–8% [9], at temperatures above 40°C - 11.6% [10]. In children 0–3 months of age with LBI, the probability of bacteremia or TBI is 5.4–22% [11, 12].
TBI does not develop in all cases of occult bacteremia; its frequency varies depending on the causative agent. Meningitis occurs in 3–6% of cases with pneumococcal bacteremia [13], but 12 times more often with hemophilus influenzae [14]. Urinary tract infection is detected in 6–8% of children, and in girls - up to 16% [15].
Neither the severity of clinical symptoms, nor high temperatures (above 40.0°), nor the lack of response to antipyretics allows for a reliable diagnosis of bacteremia, although they may indicate its increased likelihood. On the contrary, in the presence of leukocytosis above 15x109/l, as well as the absolute number of neutrophils above 10x109/l, the risk of bacteremia increases to 10–16%; less significant is the increase in the proportion of neutrophils above 60% [16–18]. But the absence of these signs does not exclude the presence of bacteremia, since every fifth child with bacteremia has a leukocytosis below 15x109/l [19].
The level of C-reactive protein (CRP) is more informative - 79% of children with bacteremia have numbers above 70 mg/l, while with viral infections only 9% [20], however, on days 1–2 of infection, CRP may still remain low . Blood culture to detect bacteremia is available only in the hospital; it takes about a day to obtain its results, so the influence of this method on the choice of treatment tactics is small. On the contrary, given the high incidence of urinary tract infections, urine cultures are highly advisable, especially since clinical urinalysis results are often negative.
In children without respiratory symptoms, bacterial pneumonia is rarely diagnosed, but with leukocytosis above 15x109/l, the presence of shortness of breath (>60 per minute in children 0–2 months, >50 in children 3–12 months and >40 in children over 1 year) and fever for more than 3 days, a chest x-ray often reveals pneumonia [21].
Febrile seizures - observed in 2-4% of children, most often between 12 and 18 months, usually with a rapid rise in temperature to 38° and above, but can also occur when it decreases. Their criteria are:
- age up to 6 years;
- absence of central nervous system disease or acute metabolic disorder that can cause seizures;
- no history of afebrile seizures.
Simple (benign) febrile convulsions do not last more than 15 minutes in duration (if they are serial, then 30 minutes) and are not focal. Complex seizures last more than 15 minutes (serial - more than 30 minutes - febrile status epilepticus), or are characterized by focality, or end in paresis.
Seizures occur more frequently with viral than with bacterial infections, and the most common cause is herpesvirus type 6, which accounts for 13–33% of initial episodes. The risk of developing febrile seizures after administration of DPT (on day 1) and viral vaccines (measles-rubella-mumps - on days 8-15) is increased, but the prognosis for children with these seizures did not differ from that for children with febrile seizures during infection.
The tendency to febrile seizures is associated with several loci (8q13-21, 19p, 2q23-24, 5q14-15), the nature of heredity is autosomal dominant. Most often, simple - generalized tonic and clonic-tonic convulsions lasting 2 - 5 minutes are observed, but atonic and tonic seizures can also occur. The facial and respiratory muscles are usually involved. Prolonged seizures are observed in 10% of children, focal seizures are observed in less than 5%; Although complex seizures may follow simple seizures, most children with complex seizures develop them on the first episode. Most often, seizures appear at the very beginning of the disease at a temperature of 38–39°, but repeated seizures can develop at other temperatures.
In a child with febrile seizures, meningitis should be ruled out first, and lumbar puncture is indicated if appropriate signs are present. Calcium testing is indicated in infants with signs of rickets to exclude spasmophilia. Electroencephalography is indicated after the first episode only for prolonged (>15 minutes), repeated or focal seizures, in which signs characteristic of epilepsy are sometimes revealed.
Rules for reducing temperature
Fever itself is not an absolute indication for lowering the temperature; in most infections, the maximum temperature rarely exceeds 39.5°, which does not pose any threat to a child older than 2–3 months. In cases where a decrease in temperature is necessary, it is not necessary to achieve normal values; it is usually enough to lower it by 1–1.5°, which is accompanied by an improvement in the child’s well-being. A child with a high fever should be given enough fluids, uncovered, and wiped with water at room temperature, which is often sufficient to reduce the temperature.
Consensus indications for reducing fever with antipyretics are [22]:
- In previously healthy children over 3 months of age: - temperature >39.0°, and/or - muscle aches, headache, - shock.
- In children with a history of febrile seizures - >38–38.5°.
- In children with severe diseases of the heart, lungs, and central nervous system - >38.5°.
- In children during the first 3 months of life - >38°.
Antipyretics are required, along with other measures (rubbing the skin, administering antiplatelet agents into a vein), in case of the development of malignant hyperthermia associated with impaired microcirculation.
Antipyretics should not be prescribed for a regular “course” of taking several times a day, regardless of the temperature level, since this sharply changes the temperature curve, which can make it difficult to diagnose a bacterial infection. The next dose of antipyretic should be given only after the child’s body temperature has returned to its previous level.
Selection of antipyretics
Antipyretics are the most widely used drugs in children, and they should be chosen primarily based on safety considerations rather than effectiveness. Numerous advertising publications emphasize the more pronounced antipyretic effect of this or that drug compared to paracetamol. This formulation of the question is inappropriate - we should be talking about the equivalence of doses and the ratio of the effectiveness and safety of the drug, and quickly reducing the temperature with the help of modern means to any level is not difficult. It is important to remember that drugs with a strong effect are more toxic, moreover, they often cause hypothermia with a temperature below 34.5–35.5 ° and a state close to collapse.
When choosing an antipyretic drug for a child, one should, along with the safety of the drug, take into account the convenience of its use, i.e., the availability of children's dosage forms and fractional dosages for different age groups. The cost of the drug also plays an important role.
The drug of first choice is paracetamol (acetaminophen, Tylenol, Panadol, Prodol, Calpol, etc.) in a single dose of 10–15 mg/kg (up to 60 mg/kg/day) [22]. It has only a central antipyretic and moderate analgesic effect, does not affect the hemocoagulation system and, unlike nonsteroidal anti-inflammatory drugs (NSAIDs), does not cause adverse reactions from the stomach. Taking into account the possible insufficient reduction in temperature at a dose of 10 mg/kg (which can lead to an overdose with repeated doses), it is recommended to use a single dose of 15 mg/kg when administered orally. Of the dosage forms of paracetamol in children, solutions are preferred - syrups, effervescent powders and tablets for preparing solutions, the effect of which occurs within 30 - 60 minutes and lasts 2-4 hours. Paracetamol in suppositories has a longer effect, but its effect occurs later. A single dose of paracetamol in suppositories can be up to 20 mg/kg, since the peak concentration of the drug in the blood reaches only the lower limit of the therapeutic range. Its effect occurs after approximately 3 hours [23, 24]. Paracetamol (Tylenol, Panadol, Prodol, Calpol, etc.) in children's forms is produced by many manufacturers; it is part of Cefekon-P suppositories. All these forms, and in dosages for children of any age, are available in the drug Efferalgan UPSA; they do not contain allergenic additives, and the solutions can be added to infant formulas and juices. Efferalgan syrup is equipped with a measuring spoon for precise dosing and is intended for children 1 month–12 years old weighing 4–32 kg (dosage is indicated taking into account differences of 2 kg).
Ibuprofen is a drug from the NSAID group, which, in addition to the central one, also has a peripheral anti-inflammatory effect; it is used in a dose of 6–10 mg/kg (daily dose, according to various sources, 20–40 mg/kg), which is comparable in effect to the above doses of paracetamol. Given this fact, WHO did not include ibuprofen in the list of essential medications. Moreover, ibuprofen produces more side effects (dyspeptic, gastric bleeding, decreased renal blood flow, etc.) than paracetamol - 20% versus 6% in large series of observations [25 - 27]. A number of national pediatric societies recommend the use of ibuprofen as a second-choice antipyretic in the following situations:
- for infections with a pronounced inflammatory component;
- in cases where fever in children is accompanied by pain reactions.
Ibuprofen is also available for children (ibufen, nurofen for children - syrup 100 mg in 5 ml); the tablet form of the drug (200–600 mg) is not suitable for this purpose.
In children during the first 3 months of life, both drugs are used in smaller doses and with a smaller frequency of administration.
Rubbing with water at room temperature provides an antipyretic effect during febrile conditions, although less pronounced than during heat shock (overheating) [28]. It is especially indicated for overly wrapped children, in whom decreased heat transfer aggravates the febrile state.
Drugs that are not recommended for use in children as antipyretics
Amidopyrine, antipyrine, and phenacetin were excluded from the list of antipyretics. However, in Russia, unfortunately, suppositories cefekon with phenacetin and cefekon M with amidopyrine continue to be used in children.
Acetylsalicylic acid in children with influenza, ARVI and chickenpox can cause Reye's syndrome - a severe encephalopathy with liver failure and a mortality rate above 50% [29, 30]. This served as the basis for a ban on the use of acetylsalicylic acid in children under 15 years of age with acute illnesses in most countries of the world (this ban has been in effect since the early 80s), as well as for mandatory appropriate labeling of drugs containing acetylsalicylic acid. Unfortunately, these rules are not followed in Russia. And Cefekon M and Cefekon suppositories containing salicylamide (a derivative of acetylsalicylic acid) in Moscow were included in the list of free prescription drugs.
Metamizole (analgin) can cause anaphylactic shock; it also causes agranulocytosis (with a frequency of 1:500,000) with a fatal outcome. Another unpleasant reaction to this drug is a prolonged collaptoid state with hypothermia (34.5–35.0°), which we observed more than once. All this was the reason for its ban or strict restriction of use in many countries of the world; it is not recommended by WHO in a special letter dated October 18, 1991. Analgin is used only in emergency situations parenterally (50% solution 0.1 ml per year of life) .
It is unacceptable to use nimesulide, an NSAID from the group of COX-2 inhibitors, as an antipyretic in children. Unfortunately, in Russia, the list of indications for its use, along with rheumatoid diseases, pain and inflammatory processes (trauma, dysmenorrhea, etc.), includes the item “fever of various origins (including infectious and inflammatory diseases)” without age restrictions . Of all NSAIDs, nimesulide is the most toxic: according to Swiss researchers [31], a cause-and-effect relationship has been established between taking nimesulide and hepatotoxic effects (jaundice - 90%). In Italy, cases of renal failure have been described in newborns whose mothers took nimesulide. The literature is replete with reports of the toxicity of this drug.
Nimesulide has never been registered in the USA (where it was synthesized), nor in Australia, Canada and most European countries. In Italy and Switzerland, the drug is licensed for adults and is used for strictly defined indications. Spain, Finland and Türkiye, which previously registered nimesulide, have withdrawn their licenses. In those few countries where nimesulide is registered (there are less than 40 of them, the drug is not registered in more than 150 countries), its use is permitted from 12 years of age, only in Brazil it is allowed to be prescribed from 3 years of age.
Sri Lanka and Bangladesh revoked the license for the use of nimesulide in children; in India, a massive campaign to ban this drug in children due to cases of fatal hepatotoxicity ended in victory: the ban was imposed by the country's Supreme Court [32, 33].
Unfortunately, both parents and pediatricians are not yet sufficiently aware of the dangers associated with the use of the “most popular” antipyretics, and therefore the use of analgin, acetylsalicylic acid, and cefekon suppositories in children in our country is not at all uncommon. The “humanitarian action” of manufacturing companies to distribute free nimesulide and the advertising of this strictly prescription drug addressed to parents increase its popularity, although at least one fatal outcome of fulminant hepatitis in a child receiving nimesulide is already known.
The toxicity of paracetamol is mainly associated with an overdose of the drug during the “course” method of its use [34, 35] in daily doses from 120 to 420 mg/kg/day, with more than half of the children receiving drugs in dosages for adults. The indicated single and daily doses of paracetamol are not toxic. The danger of this side effect of paracetamol increases with liver disease, taking hepatic oxidase activators, and in adults, alcohol [36]. With long-term use, cases of nephrotoxicity have been described. Paracetamol taken by pregnant women does not affect the development of the child, while acetylsalicylic acid has a similar effect on the level of attention and IQ of children aged 4 years.
The treatment strategy for a patient with fever involves first of all assessing the likelihood of a bacterial disease. When fever is combined with clear symptoms of the latter, antibiotics are prescribed, and the simultaneous use of antipyretics is less desirable. However, when the above temperature levels are exceeded, muscle pain, headaches, and especially in the presence of convulsions, antipyretics are administered, and it is advisable to prescribe them once, so as not to mask, if possible, the lack of effect of antibiotics, as evidenced by a new increase in temperature after a few hours. But even if a patient with fever has symptoms of only a viral infection, a course of antipyretics is not advisable.
In children with SBI, the main goal of treatment is to prevent the development of SBI, which can be achieved, for example, by administering ceftriaxone (Rocephin, Terzef, Lendacin) (50 mg/kg intramuscularly) [36]. Oral antibiotics reduce the incidence of pneumonia but not meningitis [37]. The point of view according to which antibiotics should be prescribed to all children with SBI is not shared by many authors, believing that in cases where it is possible to monitor the child, antibiotic therapy should be used only in those children who are more likely to develop SBI [38]:
- children 3 months–3 years old with a temperature above 40°, children 0–3 months — above 39°;
- with leukocytosis above 15x109/l and neutrophilia (absolute number of neutrophils above 10x109/l);
- with increased CRP - more than 70 g/l;
- if there are changes in urine analysis or culture;
- if there are changes in the chest x-ray, it should be performed in the presence of shortness of breath (>60 per 1 min in children 0–2 months, >50 in children 3–12 months and >40 in children over 1 year) and/or persistent fever above 3 days;
- upon receipt of positive blood or urine culture data (checking the adequacy of the selected starting antibiotic).
Treatment strategy for febrile seizures
A doctor is rarely present for simple febrile convulsions; doctors usually only catch prolonged or repeated convulsions. For most parents, seizures seem like a disaster, so the doctor’s task is to convince parents of their benign nature.
A child with a generalized attack should be placed on his side, with his head gently pulled back to facilitate breathing; The jaws should not be forcibly opened due to the risk of damaging the teeth; if necessary, the airways should be cleared. If the temperature persists, an antipyretic is administered: paracetamol (Tylenol, Panadol, Prodol, Calpol, Efferalgan UPSA) (15 mg/kg, if it is impossible to administer it orally, a lytic mixture is administered intramuscularly (0.5–1.0 ml of 2.5% solutions of aminazine and diprazine) or metamizole (baralgin M, spazdolzin) (50% solution 0.1 ml per year of life). Rubbing with water at room temperature also helps. For ongoing convulsions, the following is administered sequentially:
- Diazepam (Relanium, Seduxen) 0.5% solution intramuscularly or intravenously at 0.2–0.4 mg/kg per administration (not faster than 2 mg/min) or rectally - 0.5 mg/kg, but not more than 10 mg; or •lorazepam (Merlit, Lorafen) intravenously 0.05 - 0.1 mg/kg (over 2 - 5 minutes); or •midazolam (fulsed, dormicum) 0.2 mg/kg intravenously or as nasal drops.
- For children under 2 years of age, it is recommended to then administer 100 mg of pyridoxine. If convulsions continue after 5 minutes, administer: •a repeat dose of diazepam intravenously or rectally (maximum 0.6 mg/kg over 8 hours); or •phenytoin intravenously (in saline, as it precipitates in glucose solution) at a saturation dose of 20 mg/kg no faster than 25 mg/min.
- If there is no effect, you can administer: •sodium valproate intravenously (apilepsin, depakine) (2 mg/kg immediately, then 6 mg/kg/hour dropwise; dissolved every 400 mg in 500 ml of saline or 5 - 30% glucose solution); or • clonazepam (Clonotril, Rivotril) intravenously (0.25–0.5 mg/kg; this dose can be repeated up to 4 times).
- If these measures are ineffective, sodium hydroxybutyrate (GHB) 20% solution (in 5% glucose solution) 100 mg/kg is administered intravenously or anesthesia is given.
Prophylactic anticonvulsant therapy (diazepam, phenobarbital or valproic acid), although it reduces the risk of recurrent febrile seizures, is not justified and not recommended due to the side effects of these drugs [39]. Single repeated seizures develop in 17%, two repetitions in 9% and three repetitions in 6%; the recurrence rate is higher (50–65%) in children with a first episode before 1 year of age, with a family history of febrile seizures, seizures with low fever, and a short interval between the onset of fever and seizures. 50–75% of recurrent seizures occur within 1 year and all within 2 years [40–45].
Febrile seizures extremely rarely have neurological consequences, including in relation to psychomotor development, academic performance and behavior of children [44, 46]. The developmental prognosis of children who have had febrile seizures, at least at the age of 1–3 years, is, contrary to previously held belief, even better than that of other children due to better memory. In children with simple febrile seizures, the risk of developing epilepsy at age 7 years is only slightly higher (1.1%) than in children without febrile seizures (0.5%), but it increases sharply (9.2%) if developmental disorders are present. a child with complex, especially prolonged seizures and epilepsy in family members [47].
Parent training
It is very important to convey the above data on the rational use of antipyretics to parents. Recommendations for parents can be briefly summarized as follows:
- temperature is a protective reaction, it should be reduced only according to the indications indicated above;
- with regard to antipyretics, it is not “strength” that is important, but safety; to improve the patient’s condition, it is enough to reduce the temperature by 1–1.5°;
- paracetamol is the safest drug, but it is important to strictly adhere to the recommended single and daily dosages;
- paracetamol and other antipyretics should not be prescribed as a “course” in order to prevent a rise in temperature: taking an antipyretic 3-4 times a day is unacceptable due to the risk of preventing the development of a bacterial infection;
- for the same reason, you should not use antipyretics without consulting a doctor for more than 3 days;
- If possible, you should avoid using antipyretic drugs in a child receiving an antibiotic, as this makes it difficult to assess the effectiveness of the latter;
- with the development of malignant hyperthermia with spasm of skin vessels, the administration of an antipyretic drug should be combined with vigorous rubbing of the child’s skin until it turns red; you need to urgently call a doctor.
For questions regarding literature, please contact the editor.
V. K. Tatochenko , Doctor of Medical Sciences, Professor of the Research Institute of Pediatrics of the Scientific Center for Children of Children of the Russian Academy of Medical Sciences, Moscow
Nutrition for ARVI in children
Nutrition for ARVI in children is approximately the same as for a common cold. The main condition is that the baby should be offered food only if he has an appetite. There is no need to force feed your child.
You should also not give your child unhealthy foods: chips, soda. Plenty of warm drinks and easily digestible foods rich in vitamins, such as vegetables, fruits, berry purees and jellies, are recommended.
Young children are advised to offer sugar-free apple compote and dried fruit decoctions. If you are not allergic to berries, you can prepare fruit drinks or berry jelly, or simply give warm mineral water without gas.
Apricots, cherry plums, and pears can be used as a drink for children aged 3-4 years to prepare compotes (if there are no allergies). You can offer weak green tea - it contains antioxidants that help remove toxins from the body.
It is advisable to avoid decoctions and infusions of strawberries and currants - such berries are more allergenic. Replace them with bananas, grapes or kiwi.
The diet for ARVI in children should contain easily digestible and healthy foods:
- It is advisable to puree and chop products for cooking; food should be light and soft;
- during periods of illness, try to avoid purchased baby food; it is better to prepare porridge, purees, and pureed soups yourself from fresh ingredients;
- during the recovery stage, it is important to enrich the diet with proteins, so use white meat, minced meat or boiled egg whites as food additives;
- children from 3-4 years old can be offered low-fat fish such as pike perch, cod, etc.;
- Don’t forget about fermented milk products - they will maintain the balance of microflora in the intestines. Fresh kefir, natural yogurt, low-fat cottage cheese, and acidophilus mixture are suitable. You can add a spoonful of honey to such products (if you are not allergic);
- As your child recovers, return to a normal diet, but do it gradually so as not to burden the body.
Be wise when choosing food for a child with ARVI: food should be nutritious, fortified, varied, but overeating and eating harmful foods should not be allowed.
Prevention of ARVI in children
Prevention of ARVI in children is aimed mainly at increasing resistance and strengthening the immunity of the child’s body. What measures are preventative:
- hardening (playing in the fresh air, taking air baths, cool showers, walking on the grass without shoes, resting at night in a cool room, swimming in pools and open reservoirs);
- stabilization of digestive processes (consumption of vegetables and fruits, adherence to diet and drinking regime, support of intestinal microflora);
- regulation of stool, normalization of nutrition;
- ensuring proper sleep (rest not on a full stomach, ventilated air in the room, enough sleep).
Preventive measures should be carried out systematically, not forcing the child, but explaining to him the need for a particular procedure to maintain health.
If necessary and the immune system is in poor condition, sometimes it is necessary to resort to the use of drugs that stimulate immune defense.
Drugs for the prevention of ARVI in children
The special multivitamin complex Vetoron has immunomodulatory, anti-inflammatory and adaptogenic properties. It is prescribed orally from the age of 5, 3-4 drops, and from the age of 7 - 5-7 drops per day, or in capsules from the age of 6 from 5 to 80 mg once a day.
It is recommended to take ascorbic acid, retinol and B vitamins in a dose according to age. The best proportion of the above vitamins is presented in the preparations “Undevit”, “Complevit”, “Hexavit”. Dragees are taken 2 to 3 times a day for a month. In the autumn-winter period, it is useful to give your child rosehip syrup in the amount of 1 tsp. per day.
Recently, adaptogen drugs have become very popular, which stimulate the body to resist infection. We bring to your attention the dosage regimens for the most popular drugs in this category:
- Immunal - oral administration from 1 to 3 years - 5-10 drops, from 7 years - 10-15 drops. three times a day;
- Dr. Theiss drops - 10-20 drops orally from one year of age. three times a day;
- Hexal drops - 6 drops orally from the age of 12 twice a day;
- Aralia tincture - 1 to 2 drops per year of life, once a day half an hour before meals, for 14-20 days.
As emergency preventive measures, you can take drugs based on medicinal plants (chamomile, sage, calendula, colanchoe, garlic or onion), or local immunocorrective agents (Immudon, IRS-19).
ARVI in children is prone to relapses, so it is necessary to find your own recipe for prevention, which will allow you to forget about the disease for many years.