Medical editor: Zemereva N.Yu., physiotherapist June, 2021.
Inflammation of the pancreas, or pancreatitis, is a complete disaster for the entire digestive tract. The pancreas produces hormones (insulin, glucagon, lipocaine), enzymes that are necessary for normal digestion and digestion of proteins, fats and carbohydrates, and bicarbonate ions that neutralize the acidic secretions of the stomach. Pancreatitis is divided into acute and chronic, and adherence to a diet is necessary both in the acute stage and in the remission stage.
Diet rules
The goal of the diet for pancreatitis is mechanical, chemical and thermal sparing of the gastrointestinal tract. That is, by following the treatment table for inflammation of the pancreas, its normal functioning is achieved, the stomach and intestines are protected from aggressive foods, the activation of the gallbladder is reduced and liver diseases are prevented.
The treatment table for pancreatitis in the Pevzner classification is table No. 5p. Table No. 5p is somewhat different from table No. 5, which is prescribed for liver diseases, but also has a number of similar dietary restrictions. According to modern standards, a diet for exacerbation of pancreatitis is a variant of a standard diet with normal (in the acute stage) and increased (in remission) content of proteins, fats and carbohydrates, with a limitation of chemical and mechanical irritants of the gastrointestinal tract.
General principles of diet for pancreatitis
For pancreatitis, the diet is divided into two options - nutrition during exacerbation and nutrition during remission. For both options, the nutritional rules are identical.
Mechanical food processing.
- During an exacerbation of the chronic form, all food should be pureed, boiled or steamed, which ensures maximum sparing of the stomach.
- During the remission stage, oven-baked and stewed dishes are added.
Temperature regime . Food should be served neither hot nor cold. The optimal food temperature is 15-65°C.
Knowing of limits . With pancreatitis, it is very important to observe moderation while eating. Overeating is not allowed, because... this creates not only an increased load on the pancreas, but also on the entire digestive tract as a whole.
Number of meals . Meals during the day should be small, 4-6 times a day. You should not try to satisfy your hunger with a large portion of food at once; you must follow the principle: “little is better, but often.” This will facilitate the work of the pancreas, food will be better absorbed, and pain after eating will practically disappear.
Rejection of bad habits . Drinking alcohol is dangerous not only for the development of alcoholism, but with pancreatitis, alcoholic drinks provoke the formation of protein “growths” - plaques in the pancreatic ducts, clogging them, disrupting the outflow of gland secretions into the duodenum, thereby exacerbating the inflammatory process in the organ and provoking the gland to increase self-digestion .
Nicotine, in turn, interferes with the production of enzymes that neutralize acetaldehyde (this substance is formed during the breakdown of alcohol in the body, it provokes inflammation of the pancreas).
What should you know about the disease?
The causes of chronic pancreatitis are inextricably linked with the pathology of the biliary system, liver, and duodenum. These organs are united by anatomical proximity and functional dependence of the secretion produced.
Bile and pancreatic juice are secreted in portions in response to the quality and quantity of food received. Overload with frequent consumption of alcohol, fatty and spicy foods leads to hyperfunction, then depletion of cells. Under such conditions, the infection does not meet with adequate local resistance.
Stressful situations disrupt the mechanism for “controlling” the production and removal of secretions and cause a spasm of the supplying vessels and ducts. The parenchyma of the pancreas does not receive enough nutrients, oxygen, and energy, so it gradually dies. At the site of necrosis, dense scar tissue forms.
The pancreas decreases in volume and loses its lobular structure
Untreated acute pancreatitis can become chronic. Secretory deficiency affects digestion as a whole. In addition to pain, patients develop such unpleasant symptoms as frequent loose, oily stools, bloating, heartburn, and weight loss.
Exacerbation of pancreatitis: nutrition rules
In the first days of the disease, when the pain syndrome is pronounced, it is necessary to adhere to the principle: “hunger, cold and rest.” That is, all foods are excluded, a heating pad with ice is placed on the stomach, the patient must maintain physical and emotional rest.
In the first or second days from the onset of an exacerbation, fasting is indicated. You should only drink 1-1.5 liters of liquid (a glass 5-6 times a day).
Recommended:
- alkaline mineral waters (sodium bicarbonate) without gas. The most popular of them are Narzan and Borjomi.
- Rosehip decoction (no more than 400 ml per day)
- weak tea.
From 3-4 days, mucous decoctions and liquid, boiled porridge are introduced into the menu. On days 5-6, a protein omelet, pureed buckwheat or oatmeal, some crackers, boiled vegetables, and meals up to 6 times a day in small portions are allowed. Puddings, mousses, casseroles, and diluted juices are gradually being introduced into the menu. As the acute period subsides, they switch to the main diet.
The daily amount of necessary nutritional elements of the dietary table during exacerbation of pancreatitis:
- whites: 85-90 gr. (half of them are of animal origin);
- fats: 70-80 gr. (of which a third are plant-based);
- carbohydrates: 300-350 gr.
- table salt 6-8 gr. (food should be under-salted);
- free liquid 1.5-2 liters.
The energy value of the diet is 2170 - 2480 kcal.
Cereal recipes
Now let's look at several recipes for porridges that are useful for pancreatitis.
Semolina
You need to take the following ingredients:
- ¼ cup semolina;
- 1.5 glasses of water;
- a glass of milk.
Milk must be diluted in equal proportions with water. Pour the remaining water over the semolina and stir thoroughly. Let the mixture of water and milk boil, then remove the pan from the heat and pour semolina diluted with water into it, stirring it. Return the pan to the heat and cook for at least two minutes, reducing heat and stirring. Then turn off the gas, cover the porridge with a lid and leave to infuse.
Buckwheat porridge with kefir
You can introduce kefir into the diet of patients quite early - already from the second week from the onset of an attack of pancreatitis. For this therapeutic recipe, the following components are needed:
- a glass of whole grain buckwheat;
- 500 ml low-fat or one percent kefir.
Sort and peel the buckwheat, pour in kefir, and leave to steep overnight. Divide the finished porridge into two parts. One should be eaten in the morning on an empty stomach, the second in the evening a couple of hours before bedtime.
The porridge is consumed in a course of 10 days, then you need to take a break of the same duration and repeat the course. For chronic pancreatitis, it is recommended to repeat this treatment at least twice a year.
Viscous milky rice porridge
The following ingredients are taken:
- ¾ cup rice cereal;
- a glass of milk;
- glass of water.
Rice needs to be washed with warm and then hot water until it becomes clear. Boil water and add washed rice to it. Cook until half cooked. Then boil the milk, pour it hot into the porridge, stir and cook until the rice becomes soft. The finished porridge is passed through a sieve.
About 10 days after the exacerbation, you can add a small amount of sugar, salt and butter to the porridge.
A similar recipe can be used to cook porridge in a slow cooker. You need to pour the ingredients into it and set the “Milk porridge” mode.
Remission: softer diet
After the period of exacerbation has passed, patients are transferred to a less restrictive diet. Stewed and oven-baked dishes are added.
This diet includes a high protein content, a normal amount of fats and complex carbohydrates, but “fast”, easily digestible carbohydrates (sugar, honey, flour products) are severely limited. Dietary supplements containing methionine, vitamins B1, B12, choline, lecithin, etc. are recommended. The diet is enriched with dietary fiber, ascorbic acid, and calcium.
Chemical composition:
- proteins: 110-120 g, including animals 45-50 g;
- fats: 80-90 g, including vegetable fats 30 g;
- carbohydrates: 300-350 g,
- dietary fiber (fiber): 25-30 g.
Energy value 2080–2690 kcal.
The principles of dietary nutrition during the remission stage should be followed for as long as possible, ideally throughout life.
Products allowed and prohibited
Products that are recommended to be eaten during pancreatitis should facilitate the work of the pancreas as much as possible, reduce the amount of enzymes it synthesizes, quickly evacuate from the stomach and small intestine, and not cause flatulence, which provokes already existing abdominal pain.
In addition, to facilitate the synthesis of enzymes in the pancreas, which contain proteins, food should be easily digestible and rich in proteins.
If you have pancreatitis, you should avoid foods that stimulate the production of gastric juice and, accordingly, pancreatic secretions. That is, the production of pancreatic enzymes significantly exceeds the required need for them for the digestive tract as a whole, and therefore, with pancreatitis, the excess enzymes are spent on digesting the own pancreas. To reduce the amount of synthesized enzymes and relieve inflammation of the organ, it is necessary to give up a number of foods.
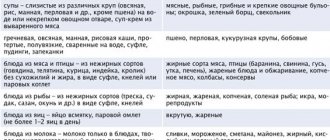
| Prohibited foods for pancreatitis | Authorized Products | |
| Soups | in meat, mushroom and fish broths, complex (cabbage soup, borscht, rassolnik), dairy, cold (okroshka, beetroot soup). | Soups should be vegetarian, with pureed vegetables (carrots, pumpkin, zucchini, potatoes), with noodles, semolina or oatmeal. |
| Bread | Fresh wheat or rye, puff pastry and pastry products, flatbreads, fried pies. | Day-old or dried white bread, dry unsweetened cookies, crackers. |
| Meat | Fatty meats (pork, lamb) and poultry (duck, goose), sausages, liver, kidneys and brains, smoked meats and canned food. | Low-fat varieties (beef without films and tendons, veal), white meat chicken, turkey, rabbit. The meat should be boiled and preferably pureed (soufflé, steamed cutlets, dumplings), beef stroganoff. |
| Fish | Fatty fish, salted and smoked, fried, canned. | Low-fat varieties (cod, pollock) boiled or chopped, aspic. |
| Dairy | Among lactic acid products, you should avoid those that have a high percentage of fat content - sour cream, fatty, salty and spicy types of cheese. | Low-fat milk, non-sour and low-fat cottage cheese, yoghurts, kefir, curdled milk no more than 2% fat, unsalted and low-fat cheeses. |
| Cereals | A ban on pearl barley, millet, corn and wheat cereals, as they remain in the stomach and intestines for a long time, stimulating the production of pancreatic juice. | Buckwheat (mashed), oatmeal, semolina, rice porridge in water with milk 50/50, puddings and casseroles with cereals, cottage cheese. |
| Eggs | Fried and hard-boiled. | Omelettes steamed from whites, it is allowed to add 1 yolk no more than once a week |
| Vegetables | Cabbage, eggplant, radish, turnip, radish, garlic and spinach, bell pepper. | Potatoes, carrots, zucchini, beets, cauliflower, pumpkin, green peas. |
| Dessert | Chocolate, raw unprocessed fruits and berries (dates, grapes, figs, bananas), ice cream, jam. | It is better to replace sugar with xylitol, use only ripe and non-acidic varieties of fruits and berries, prepare mousses, jellies, puddings, compotes (all pureed), baked apples from them. |
| Spices and sauces | Black and red pepper, coriander, horseradish, hot tomato sauce, vinegar | Dairy or sauces based on diluted vegetable broth; do not sauté when adding flour. |
| Fats | All refractory fats (pork, beef, lamb fat), tail fat. | Butter (no more than 30 grams per day), refined vegetable oil (10 - 15 grams), add oils to ready-made dishes without heating them. |
| Beverages | Coffee, cocoa, strong tea, sweet carbonated drinks, grape juice. | Lightly brewed tea with lemon, still mineral water, rosehip infusion, juices half diluted with water. |
Mineral deficiency
In case of intestinal diseases, the body receives insufficient minerals, but this deficiency can be replenished with the help of dairy products
. Not only do they contain a lot of minerals, but they are also easily absorbed by the body. Dairy products can provide the body with a sufficient amount of phosphorus and calcium, but one must keep in mind that not all dairy products can be well tolerated by the body in case of intestinal diseases. For example, fresh milk may be too “heavy”, and fermented milk products, due to their increased acidity, can irritate the walls of the stomach.
The most neutral and useful product for intestinal diseases is unleavened cottage cheese.
, as well as unsalted and low-fat
cheese
. These products can be an alternative to kefir and yogurt. It is only important that the products are fresh and natural, without additional spices or flavor enhancers.
Consequences of dieting
Following a diet for pancreatitis is aimed at maximizing sparing of the pancreas, reducing the inflammatory process in the gland, relieving a painful attack and preventing the development of possible complications.
In addition, the diet normalizes the production of digestive enzymes, blocks the pancreas from “eating” itself, maintains the integrity of the intestinal mucosa, limits the entry of toxic substances into the body, and normalizes the functioning of the gastrointestinal tract as a whole.
In case of non-compliance with the diet during acute pancreatitis or exacerbation of chronic pancreatitis, the following complications arise:
- jaundice (due to impaired outflow of bile);
- bleeding in the digestive tract (stomach ulcers, varicose veins of the esophagus, Mallory-Weiss syndrome);
- pleurisy;
- damage to the duodenum (obstruction);
- diabetes.
Sources:
- Ministry of Health of the Russian Federation. Medical nutrition standards. Methodological manual, 2022.
- Order of the Ministry of Health of the Russian Federation of September 23, 2022 N 1008n “On approval of the procedure for providing patients with therapeutic nutrition”
Diagnostics
The identification and treatment of pancreatitis is carried out by a general practitioner and gastroenterologist together with an endocrinologist, surgeon and other specialists.
Often, patients with an acute form of the disease are taken by emergency medical care to a surgical hospital, where a differential diagnosis of pancreatic damage with acute appendicitis, cholecystitis and other pathologies is carried out. After clarifying the complaints, collecting an anamnesis, including dietary patterns, bad habits, frequency of relapses, concomitant diseases of the biliary system, and examination, the doctor refers the patient for tests, as well as instrumental studies.
As part of the laboratory examination of the patient, the following is carried out:
- General clinical blood test. There are signs of inflammation: acceleration of ESR, leukocytosis.
- Biochemistry of blood. Damage to the pancreas during pancreatitis is characterized by increased activity of enzymes (amylase, lipase), possible hyperglycemia, hypoalbuminemia and hypocalcemia, bilirubinemia, as well as increased activity of liver enzymes (ALT, AST, transaminases), CRP.
- Biochemical examination of urine. It is carried out to determine amylase activity in urine.
- Coprogram. Steatorrhea is characteristic.
- Determination of pancreatic elastase in feces.
Instrumental diagnosis of pancreatitis includes:
- Ultrasound of the abdominal organs is a method of visualizing the gland itself and surrounding organs;
- SCT and MRI of internal organs to obtain more detailed information about anatomical changes in them;
- endoscopic retrograde cholangiopancreatography for the purpose of visualizing the lumen of the ducts, taking pancreatic secretions, removing stones;
- endoscopic elastography of the pancreas - allows you to determine the rigidity and rigidity of the tissue, assess the degree of its connective tissue replacement and the secretory function of the organ;
- esophagogastroduodenoscopy to assess the condition of the hollow digestive organs.