Diseases of the pancreas, primarily chronic pancreatitis, represent damage to the pancreas by various etiological (causal) factors, but having a progressive relapsing course with disruption of the intrasecretory (hormonal) and exocrine (enzymatic) functions of the pancreas, its gradual atrophy and replacement of pancreatic cells with connective ( fibrous) tissue.
Chronic pancreatitis refers to diseases that are characterized by a variety of nonspecific manifestations that depend on the phase of the disease, the cause, and the condition of other digestive organs.
Chronic pancreatitis. Reasons for development
Alcohol intoxication - alcoholic pancreatitis
Chronic alcohol intoxication plays a major role in the development of chronic pancreatitis (25-70% of cases).
- Alcohol has a direct toxic effect on pancreatic cells, causing inflammation and death of organ cells with their replacement by connective tissue (fibrosis and fatty degeneration of pancreatic tissue).
- Alcohol increases the pressure in the pancreatic ducts, the mucous membranes of the ducts become permeable to enzymes and damage to pancreatic cells begins.
- Alcohol changes the composition of pancreatic juice, which disrupts the patency of the pancreatic ductal system and can lead to the formation of calcifications (plugs of protein and Ca salts).
When you stop drinking alcohol, the prognosis is favorable in most cases!
Condition of the biliary system - biliary pancreatitis
In 25-40% of cases, the cause of chronic pancreatitis may be the condition of the human biliary system (see the section of the site dedicated to diseases of the biliary tract) - biliary pancreatitis.
In the development of chronic pancreatitis, an important role is played by an increase in pressure in the pancreatic duct due to an obstruction in the final section of the common bile duct (spasm of the sphincter of Oddi, congestion in the duodenum (duodenostasis), inflammation of the duodenal papilla (papillitis), stones in the ducts.
The pancreatic duct and the common bile duct are in anatomical proximity and connect in the area of the papilla of Vater (sphincter of Oddi), which opens into the duodenum.
Trouble in this area in the form of inflammation (papillitis), spasm, with ulcerative disease of the duodenum due to swelling of the papilla of Vater, difficulty in the outflow of pancreatic secretions develops, increased pressure in its ducts, and this in turn leads to activation of enzymes, exacerbation of chronic pancreatitis .
Due to its anatomical features, it is important that bile (bile reflux), “thick” bile (sludge) can be refluxed from the common bile duct into the pancreatic duct, which causes an increase in pressure in the ducts of the gland and activation of enzymes in the gland itself.
High acidity of gastric juice also contributes to an increase in pressure in the ducts in conditions of obstructed outflow.
Timely treatment of disorders of the duodenum, biliary system and gallbladder preserves the pancreas.
Taking medications - drug-induced pancreatitis
Some medications also play a significant role in the occurrence of chronic pancreatitis through their side effects on pancreatic function. The following drugs have been noted in clinical practice: hypothiazide, furosemide, tetracycline, paracetamol, estrogens, sulfonamides, metronidazole, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, etc.
Trauma, birth defects
The causes of chronic pancreatitis can be: trauma to the abdominal cavity, congenital malformations of the pancreas.
Hereditary pancreatitis
A hereditary predisposition to the development of chronic pancreatitis is known, but is extremely rare and manifests itself in adolescence (10-12 years). These patients have an increased risk of developing pancreatic cancer.
Some infections (viral hepatitis, acute intestinal infections, tuberculosis and others), and parasitic infections (opisthorchiasis, giardiasis) may be important in the development of chronic pancreatitis.
Other reasons
Chronic pancreatitis can be caused by:
- disorders of the blood supply to the pancreas (pancreatic ischemia - ischemic pancreatitis),
- dysmetabolic chronic pancreatitis,
- carbohydrate metabolism disorder (diabetes mellitus),
- disorders of fat metabolism (hypercholesterolemia),
- hypercalcemia (increased calcium in the blood).
What diseases contribute to the occurrence of biliary pancreatitis?
The given pathogenesis options are typical for many diseases of the hepatobiliary system. Therefore, biliary-dependent pancreatitis occurs as an addition and complication:
- cholelithiasis (in 2/3 of cases);
- congenital anomalies of the bile and pancreatic ducts;
- disturbances of motor function (dyskinesia) of the gallbladder and pathways;
- chronic cholecystitis;
- hepatitis and cirrhosis of the liver;
- local pathology of the nipple of Vater due to inflammation, spastic contraction, stone blockage, cicatricial changes;
- parasitic lesions of the liver and gall bladder.
Provoking factors may be:
- malnutrition, consumption of foods that stimulate bile secretion;
- treatment with medications with choleretic properties;
- sudden weight loss.
Biliary-dependent pancreatitis occurs in acute or, more often, chronic form. Acute - occurs against the background of an attack of cholelithiasis, sharply aggravates the patient’s condition, and causes death. Chronic - lasts up to six months or more. Exacerbations are replaced by remissions. The outcome depends on the results of treatment of the biliary tract and diet.
Chronic pancreatitis. Clinical manifestations
Chronic pancreatitis in a quarter of patients is asymptomatic, especially in the initial period.
Stomach ache
Subsequently, in 80-90%, the main characteristic symptom is abdominal pain syndrome (abdominal pain).
The pain is of the nature of recurrent (repeating) attacks - “pancreatic colic” and often becomes permanently debilitating.
The localization of pain depends on the damage to different parts of the pancreas, so when the head is affected - pain in the right hypochondrium, the body - pain in the epigastric region, when the tail of the pancreas is damaged - pain in the left hypochondrium. When the entire gland is affected, “girdling” pain is observed, which occurs in 30-35% of patients.
Often there is irradiation of pain to the left shoulder blade, to the left half of the chest, to the heart area.
Pain usually occurs 30-40 minutes after eating a large, fatty meal, drinking alcohol, cold fizzy drinks, spicy seasonings, large amounts of raw vegetables, citrus fruits.
Pain can last from 30 minutes to 3 or more hours.
Pain can be provoked by psycho-emotional stress, heavy physical work, and hypothermia.
Hunger pains that occur 4-6 hours after eating are often observed.
In case of pain, patients take a forced position, they cannot lie on their backs, relief is found only in the knee-elbow position or on the stomach, patients switch to fasting and drinking alkaline waters.
The first years in the initial stage of the disease are intense. frequent, requiring intensive therapy, after 5-10 years the pain is aching, dull, without clear localization and irradiation. This is a sign of disease progression with the development of pancreatic enzymatic insufficiency. During the period of development of complications, after 7-15 years (but can happen at any stage of the disease), pain becomes rare and not pronounced and in clinical manifestations, manifestations of enzymatic deficiency (exocrine pancreatic insufficiency) and disturbances of intrasecretory function - carbohydrate disorders metabolism, may be diabetes.
Dyspeptic disorders
Dyspeptic disorders (dysmotor gastroduodenal dyspepsia syndrome) are observed 3-5 years from the onset of the disease and include:
- dry mouth, nausea,
- vomiting, often at the height of pain, repeated, not bringing relief to the patient,
- heartburn, belching,
- flatulence, feeling of fullness in the stomach.
Exocrine insufficiency syndrome
The pancreas produces few digestive enzymes, the processes of food digestion and absorption of food components are disrupted, and as a result of this the following appear:
- diarrhea, which may alternate with constipation,
- increase in stool volume up to 500 g or more,
- stool up to 2-6 times a day, often after meals, the stool is gray, oily, difficult to wash away, foul-smelling, unformed (steatorrhea is observed in 5-15% of cases),
- dryness and flaking of the skin,
- stomatitis, glossitis (inflammation of the tongue, swelling with teeth marks),
- bone pain,
- decreased or complete loss of appetite (anorexia),
- weakness.
Intrasecretory pancreatic insufficiency syndrome
They manifest themselves in the form of diabetes mellitus (thirst, dry mouth, increased urination) in 3-10% of patients with chronic pancreatitis.
Signs of pancreatogenic diabetes usually appear late - 15 or more years from the onset of chronic pancreatitis. Sometimes this may be the only manifestation of painless pancreatitis.
Syndrome of vegetative and mental disorders
- emotional lability,
- irritability,
- sleep disorders,
- depressive state.
Prognosis and prevention
Timely treatment of calculous cholecystitis and cholangitis can prevent damage to the pancreas. It is especially important to decide on surgery to remove the stone. Planned minimal intervention is less difficult for patients to tolerate than surgery in the presence of biliary pancreatitis.
The patient's compliance with the conditions of the postoperative period and diet helps eliminate signs of inflammation and achieve complete recovery. An unfavorable prognosis awaits a person with a long course of cholelithiasis and repeated exacerbations of pancreatitis. The gland gradually becomes sclerotic, which affects other digestive organs.
Disturbances in the biliary system can lead to severe damage to the pancreas and digestion in general. In treatment, surgical removal of stones in the bile ducts should be used in a timely manner.
Chronic pancreatitis and its complications
During any period of the course of chronic pancreatitis, complications of chronic pancreatitis may occur. If the clinical picture of the disease changes, new complaints and manifestations of the disease appear, this is a signal to actively search for complications of chronic pancreatitis.
The most common complications of chronic pancreatitis are divided into local and general.
Local complications of chronic pancreatitis include jaundice, which can occur due to compression of the common bile duct by the pancreas at the site where it passes through the dense tissue of the pancreas or concomitant liver diseases, such as toxic (alcoholic) or viral hepatitis.
Chronic pancreatitis threatens 25% of all patients with the formation of false cysts of the pancreas. These fluid-filled cystic formations do not have a wall and are lined with epithelial cells, which constitute a fibrous membrane. It is believed that they are usually localized inside the pancreatic tissue and arise as a result of blockage of the gland duct with connective tissue, protein plugs and stones (calcifications); they can form during exacerbation of chronic pancreatitis.
Pancreatic cysts are dangerous on the one hand, because they can compress the common bile duct, which leads to obstructive jaundice, and on the other hand, secondary infection of the contents of the pancreatic cyst may occur. Clinically, suppurating cysts are manifested by a wide variety of symptoms characteristic of abscesses (ulcers) of the abdominal cavity (abdominal pain, fever). The tactics of medical care in these cases are determined by surgeons.
Sometimes pancreatic cysts involve large blood vessels in the pathological process, a false aneurysm (dilation) of the vessel occurs, and if the cyst communicates with the pancreatic duct and damages a blood vessel, gastrointestinal bleeding may develop.
A serious complication of pancreatic cysts in chronic pancreatitis is the occurrence of pancreatic ascites (inflammation of the abdominal cavity), which occurs when the cyst wall or pancreatic duct ruptures, or when fluid constantly leaks from the cyst cavity. In these cases, it is necessary to establish the source of fluid in the abdominal cavity. Treatment is carried out in a surgical hospital; surgical intervention is not excluded.
Chronic pancreatitis threatens 5% of patients with the development of thrombosis (blockage) of the splenic vein, which runs in the parapancreatic tissue (in the tissue near the pancreas). As a result of inflammation of the tissues near the pancreas, thrombosis of the splenic vein occurs, which leads to the reverse flow of blood into the veins of the stomach and dilation of these veins, and as a result, severe bleeding can occur.
Common complications of chronic pancreatitis include the consequences of impaired digestion of food and absorption of nutrients (see section “Clinical manifestations”, paragraph 2. Dyspeptic disorders) and disorders of carbohydrate metabolism (diabetes mellitus).
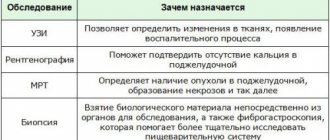
Basic diagnostic methods
An ultrasound will help make the correct diagnosis.
Only after undergoing a medical examination can a doctor make a final and correct diagnosis. To do this, you need to undergo the following types of examination:
- Ultrasound examination
- Biochemical blood test (transaminase levels increase)
- Cholangiopancreatography (with reverse contrast injection)
- MRI
- General clinical blood test (relevant only in the presence of acute inflammation, because then the number of leukocytes increases)
These types of studies help to obtain maximum expanded information to establish an accurate diagnosis.
Diagnosis of chronic pancreatitis and its complications
- Clinical examination, anamnesis.
- Clinical blood test.
- Pancreatic tests to determine the active process in the pancreas:
- blood amylase and lipase,
- urine amylase - these indicators depend on the time of blood and urine sampling in relation to the onset of an exacerbation, therefore, blood and urine amylase is determined already in the first hours of an exacerbation of the disease, and blood lipase is determined on days 4 - 12 from the onset of an exacerbation.
- blood glucose.
- Determination of structural changes in the pancreas.
4.1. Ultrasound examination of the pancreas is the main diagnostic method for studying the pancreas and biliary system:
- determination of the size, degree of fibrosis, size of the Wirsung duct of the pancreas,
- complications of chronic pancreatitis (cysts, stones in the pancreatic duct, tumors),
- condition of the liver, biliary tract and gallbladder function (pathology of the biliary system is excluded).
4.2. Survey X-ray of the abdominal cavity (calcifications in the pancreatic ducts, duodenography in conditions of hypotension (determination of the location of the duodenum).
4.3. Esophagogastroduodenoscopy with examination of the duodenum, the area of the papilla of Vater to exclude inflammation, stricture (scar narrowings) or tumor.
4.4. Computed tomography of the abdominal cavity (if indicated).
4.5. Study of exocrine pancreatic function:
- scatological examination of stool (detection of steatorrhea),
- Elastase 1 pancreatic in feces.
Elastase 1 as a marker of exocrine pancreatic function. Elastase 1 is a proteolytic enzyme synthesized exclusively by the pancreas. This test allows you to evaluate not only pancreatic enzyme deficiency, but also evaluate the dynamics of the exocrine function of the pancreas and more accurately prescribe enzyme preparations and make a prognosis of the disease. The method has high specificity and sensitivity and is based on the use of highly specific antibodies to Elactase 1.
Determination of Elastase 1 is indicated for all diseases of the gastrointestinal tract to determine the involvement of the pancreas in the pathological process, in case of any abdominal pain and digestive disorders.
Characteristics of determination of Elastase 1 in feces:
- absolute specificity for the pancreas,
- full correlation with more labor-intensive tests (secretin-pancreozymin test),
- test results are not affected by enzyme replacement therapy,
- high specificity (93%), high sensitivity (93%),
- one stool sample is sufficient to make a diagnosis,
- high stability of pancreatic Elastase-1 allows not to limit the time of delivery of the analysis to the diagnostic laboratory,
- has no contraindications, is safe and not burdensome for the patient.
5. Identification of bacteria, viruses, parasites that are associated with chronic pancreatic diseases.
6. Determination of tumor markers of the pancreas: CA-19-9, CEA, with an increase in these indicators, which may reflect the inflammatory process, but are an indirect sign of possible transformation into a tumor form of pancreatic damage.
- Determination of gastric juice secretion (pH-metry, see Gastropanel for blood tests).
14.06.2018
Author of the article: Gerlakh Alexander Alexandrovich, gastroenterologist of the highest category.
Chronic pancreatitis is characterized by a progressive irreversible decrease in the exocrine and endocrine function of the pancreas. There are many different classifications of chronic pancreatitis.
In the practical work of a general practitioner and gastroenterologist, the most acceptable and used is the clinical and morphological classification according to V.T. Ivashkin.
- I. According to morphological characteristics: interstitial edematous, parenchymatous, fibrinous sclerotic (indurative), hyperplastic (pseudotumorous), cystic.
- II. According to clinical manifestations: pain variant, hyposecretory, astheno-neuratic, latent, combined.
- III. According to the nature of the clinical course: rarely recurrent, often recurrent.
- IV.According to etiology: biliary-dependent, alcoholic, dysmetabolic (diabetes mellitus, hyperparathyroidism), infectious, drug-induced, idiopathic.
Based on this classification. Let us dwell on biliary-dependent pancreatitis. Recently, the number of patients with cholelithiasis has increased. As a result, there are more patients with biliary-dependent pancreatitis.
Etiology and pathogenesis . The cause-and-effect relationship between cholelithiasis (GSD) and pancreatitis is well known. Stones from the common bile duct, entering the ampulla of the papilla of Vater, can cause the development of acute pancreatitis. If the stone passes into the duodenum, the inflammatory phenomena in the pancreas subside quickly enough. When a calculus is strangulated in the ampulla of the major duodenal papilla, the signs of exacerbation of pancreatitis increase. In recent years, biliary sludge has been given an increasingly important role in the development of chronic pancreatitis [1]. As a result of destabilization of the physicochemical state of bile, precipitation of its main components occurs and the formation of biliary sludge (BS) in the gallbladder. An important factor contributing to the persistence of BS is dysfunction of the gallbladder and sphincter apparatus of the biliary tract. The constant passage of BS through the biliary tract leads to damage to the mucous membrane, mainly in the area of the sphincter of Oddi. Traumatization of the mucous membrane occurs by microlites, which make up the main part of the BS. As a result of this, secondary dysfunction of the sphincter of Oddi first develops, and subsequently stenotic papillitis forms. Functional and organic changes in the area of the major duodenal papilla disrupt bile outflow and contribute to the development of biliopancreatic reflux. It is bile refluxate that is the main pathogenetic factor in the occurrence of acute or exacerbation of chronic pancreatitis. In this regard, such pancreatitis is usually referred to as biliary pancreatitis (BP). Considering the close connection between BS and the development of acute pancreatitis, it is currently generally accepted that the diagnosis of idiopathic pancreatitis can be made only after excluding microlithiasis in the patient.
Clinic. The leading symptom in the clinical picture of PD is abdominal pain. They are usually localized in the epigastrium and radiate to the back. Pain is usually associated with overeating, eating spicy, fatty, fried foods, or occurs spontaneously at night. The cause of the development of pain syndrome is mixed. On the one hand, they are caused by the presence of biliary pathology and arise, as a rule, as a result of dysfunction of the sphincter apparatus of the biliary tract. On the other hand, they are associated with exocrine pancreatic insufficiency.
The main causes of abdominal pain in PD may be the following:
1. Inflammatory process in the pancreatic parenchyma (stretching of the capsule, compression of nerve endings).
2. Complications of chronic pancreatitis
intrapancreatic: duct obstruction; pseudocysts; pancreatic neuritis (scar changes in the area of intrapancreatic nerve endings).
extrapancreatic: stenosis of the intrapancreatic portion of the common bile duct with the development of biliary hypertension; stenosing papillitis; stenosis of the descending duodenum.
3. Exocrine insufficiency syndrome (flatulence with increased intraintestinal pressure, impaired motor function of the small and large intestine, excessive bacterial growth in the intestine).
4. Concomitant diseases of the digestive system (chronic gastritis, duodenitis, erosive and ulcerative lesions of the gastroduodenal region).
The causes of abdominal pain vary depending on the stage of the disease. In the acute period, the leading cause is the inflammatory process in the pancreatic parenchyma. Subsequently, as acute phenomena subside, various complications and exocrine pancreatic insufficiency take first place as the causes of pain. The mechanism of pain formation in chronic PD is due to the peculiarities of duodenal digestion. The nutrients supplied from the stomach to the duodenum are a mixture of long-chain polypeptides that stimulate pancreatic secretion to a greater extent than their monomers. It should be noted that the intestinal (duodenal) phase of pancreatic secretion is the main one, since it accounts for 70–80% of the volume of postprandial secretion. This phase of intestinal secretion is regulated by reflex and humoral mechanisms.
The most important is hormonal regulation through cholecystokinin-producing cells. Nutrients release cholecystokinin-pancreozymin from I-cells, the most important stimulator of pancreatic secretion of enzymes in its intestinal phase [3].
Various strictures and deformations of the ductal system, both from the pancreas and the terminal sections of the bile ducts, make it difficult for an adequate outflow of pancreatic juice at the height of digestion. In this regard, hypertension in the ductal system increases, which leads to the occurrence or intensification of pain. The main clinical symptoms of exocrine pancreatic insufficiency are: a feeling of heaviness in the epigastrium that occurs immediately after eating, belching, bloating, stool disorders (usually diarrhea, an increase in the mass of stool and a change in its color, a foul odor and a greasy appearance), weight loss. However, such a clear clinical picture is observed only in a small number of patients with severe disorders of pancreatic function (with exocrine deficiency of more than 90%) [4].
During the attack, moderate fever is possible. A pronounced clinical picture of acute PD develops when a calculus is strangulated in the ampulla of the major duodenal papilla with disruption of the outflow of bile and pancreatic secretions. In this situation, the clinical picture of obstructive jaundice with partial or complete disruption of bile outflow and pancreatic juice is added.
Diagnostics. Laboratory signs include moderate leukocytosis, changes in liver function tests (increased activity of aminotransferases, alkaline phosphatase, GGTP), as well as increased levels of serum amylase and lipase. It should be noted that changes in liver function tests in PD are more pronounced than in pancreatitis of alcoholic or other etiology. To diagnose exacerbation of biliary pancreatitis, it is important to study the levels of serum amylase and lipase. It should be taken into account that the level of amylase increase depends on the time of taking the material for research. Thus, the level of amylase increases already in the first hours of exacerbation of pancreatitis, reaches a maximum by the end of the first day, remaining at elevated levels for another 2–3 days, and by the 4th day it decreases to normal levels. At the same time, the dynamics of changes in the level of lipase differs from amylase. The level of lipase increases from the end of the 4th day, reaches a maximum on the 5th–6th day and remains at elevated levels for up to 12 days. Naturally, with complicated pancreatitis, the dynamics of amylase and lipase levels may differ significantly.
Methods by which pancreatic enzyme deficiency is detected can be divided into 2 groups.
1. Direct methods - based on determining the activity of pancreatic enzymes in various biological media - pancreatic juice, blood plasma, duodenal contents, feces, urine.
2. Indirect methods - based on assessing the digestive ability of its enzymes (scatological study with determination of the amount of neutral fat or the presence of slightly changed muscle fibers).
In practice, fecal diagnostic tests are most often used to detect exocrine pancreatic insufficiency:
- quantitative study of neutral fat in the volume of feces excreted within 72 hours. An increase in fat content of more than 6 g/day is a pathology;
- determination of pancreatic elastase-1 in feces. A level of less than 200 mcg of elastase in 1 g of feces indicates pancreatic insufficiency.
The main instrumental diagnostic method is ultrasound examination (US). Stones or various forms of biliary sludge are detected in the gallbladder and/or common bile duct (Fig. 2, 3, 4). If it is difficult to visualize the common bile or pancreatic duct using transabdominal ultrasonography, endoscopic ultrasound is used (Fig. 5). The common bile duct can be of normal size; its expansion occurs when a stone is pinched in the terminal section or ampulla of the major duodenal papilla. The Wirsung duct is of normal size or moderately dilated. It should be noted that the normal size of the common bile duct according to ultrasound is not a convincing sign of the absence of pathology in it. According to our data (Fig. 6), with a common bile duct width of up to 6 mm, accepted by most researchers as the norm, the frequency of detection of stones in the common bile duct with cholecystolithiasis is 20.6%, and with the gallbladder removed for cholelithiasis - 43.4%. Changes in the pancreatic parenchyma depend on the stage of the process. In the early stages, changes in the pancreas cannot be detected. Subsequently, the heterogeneity of the structure and the unevenness of its contours are revealed. During exacerbation of PD, ultrasound signs of edema of pancreatic tissue are detected. Dynamic cholescintigraphy (DCSG) is indicated to determine the patency of the bile ducts. The ability to trace the entire process of bile redistribution with analysis of its accumulation and evacuation into the duodenum is a valuable advantage of DHSG [6], especially in PD, when ERCP is associated with a high risk of exacerbation of the pathological process in the pancreas. At the same time, ERCP is the most common method for diagnosing pathology of both the biliary system and the pancreas. If necessary, papillotomy or papillosphincterotomy is simultaneously performed during the examination. Violation of the functional state of the pancreas, as mentioned above, is not always accompanied by changes in its parenchyma, therefore methods such as computed tomography, nuclear magnetic resonance and transabdominal ultrasound may be uninformative. An alternative method for diagnosing PD in these cases is EUS. Recently, in clinical practice, magnetic resonance cholangiopancreaticography has been increasingly used to diagnose PD, which allows simultaneous assessment of the condition of the bile and pancreatic ducts. Various criteria have been proposed for predicting the severity of pancreatitis. The most widely used system is based on the Renson criteria [5], which can also be applied to PD.
Treatment. Drug treatment of PD does not differ from the treatment of other forms of pancreatitis, however, it has its own characteristics associated with the pathogenesis of the disease and should primarily be aimed at eliminating the cause that caused the development of biliary pancreatitis. Fasting for 3-5 days is recommended. The volume of fluid taken should meet the body's needs (1.5–2.0 l). To suppress pancreatic secretion and create its maximum functional rest, ranitidine 150 mg 2 times, famotidine 20-40 mg 1-2 times a day, omeprazole 40 mg 1-2 times a day, sandostatin 0.1-0, 2 mg - 1-2 times/day s.c. Antacids are indicated - Maalox, Remagel, phosphalugel - 10-15 ml every 2-3 hours. According to indications - polyglucin (dextran) 400 ml/day, hemodez (pavidon) 300 ml/day, 10% albumin solution 100 ml/day, 5-10% glucose solution 500 ml/day - intravenously. For pain relief - baralgin 5 ml , papaverine 2 ml of a 2% solution 1–2 times a day, platiphylline 1–2 ml of a 0.2% solution 1–2 times a day, drotaverine 2–4 ml of a 2% solution 1–2 times a day and others. For severe and resistant pain - non-narcotic analgesics (tramadol 1 capsule (0.05 g) 2-3 times a day or 1-2 ampoules (0.05-0.1 g) slowly intravenously or intramuscularly). It should be noted that that myotropic antispasmodics used to relieve abdominal pain have a number of side effects that limit their use. Thus, the antispasmodic effect can simultaneously be accompanied by a decrease in motility of the stomach, duodenum, intestines and the secretion of saliva, gastric and intestinal juice (atropine, metacin, belladonna), a bronchodilator effect (papaverine, aminophylline), impaired atrioventricular conduction (papaverine), hypotension ( drotaverine, aminophylline), dizziness, sleep disturbance (halidor) and other disorders. These drugs are contraindicated for glaucoma, prostate adenoma (atropine, metacin, platifillin), organic diseases of the liver, kidneys (platifillin), hypotension (halidor, nitroglycerin, no-spa, aminophylline, platifillin). In this regard, to relieve abdominal pain in PD, the use of Duspatalin (mebeverine) 200 mg 2 times a day is indicated. Clinical experience of using the drug abroad is quite convincing and amounts to about 40 years. Duspatalin appeared on the Russian pharmaceutical market relatively recently and is used mainly for irritable bowel syndrome. Recent studies have shown that the antispasmodic effect of duspatalin is accompanied by relief of pain and dyspeptic disorders in cholelithiasis (Table 1).
Dynamics of clinical symptoms during 7–14 days of therapy with Duspatalin for cholelithiasis
| Symptoms | N | Treatment effectiveness, % | |
| in 7 days | in 14 days | ||
| Pain in the right hypochondrium | 20 | 70 | 85 |
| Bitterness in the mouth | 13 | 30 | 45 |
| Belching | 9 | 20,5 | 32 |
| Nausea | 15 | 14,6 | 20,5 |
As can be seen from table. 1 after 7 days of treatment with Duspatalin, pain in the right hypochondrium decreased in 14 of 20 patients with cholelithiasis (70%), and after 14 days completely disappeared in 17 (85%) patients and significantly decreased in duration and intensity in 3 patients ( 15%) [7].
Similar data were obtained with the use of Duspatalin in patients with postcholecystectomy syndrome [8]. This fact served as the basis for its use in PD. It should be noted that the antispasmodic effect of Duspatalin is higher compared to other known drugs and, for example, is 30 times higher than that of platyphylline. The drug is practically not absorbed into the general bloodstream and, therefore, has no side effects, which allows it to be used for a long time (one month or more).
Pancreatic enzyme inhibitors are used - contrical, gordox. When expanding the diet, enzyme preparations are prescribed - Creon, pancitrate, mezim, festal, pancreatin and others.
It should be noted that digestion is a normally quite stressful process. In healthy people, about 300–600 thousand IU of lipase are released during the digestion phase (within 6 hours), which corresponds to 87–171 Mezim tablets, 50–100 Festal tablets or 30–60 Creon 10,000 capsules).
This places serious demands on enzyme replacement therapy for exocrine pancreatic insufficiency, which can be formulated as follows:
- the active principle (pancreatin) must reach the site of application (duodenum) without being destroyed in the stomach and be active only in the intestine;
- the effect of the drug should develop with the beginning of food entering the duodenum.
- In this regard, the ideal enzyme preparation must meet the following requirements:
- have an optimal composition of enzymes in physiological proportions;
- be acid-resistant against gastric juice;
- mix evenly and quickly with food;
- simultaneously with food enter through the pylorus into the duodenum;
- have an optimal effect in the pH range 4–7;
- quickly and completely release enzymes in the duodenum;
- have no side effects.
Experimental studies have established that particles with a diameter of 1–1.5 mm are better mixed with food in the stomach and at the same time leave it. Thus, the effectiveness of an enzyme preparation is determined not so much by the content of enzymes in one tablet or capsule, but by its dosage form. When using tablet forms of enzyme preparations, only about 10% of the administered dose reaches the site of action in the duodenum, the remaining 90% of the drug is destroyed in the stomach. In this regard, to obtain the maximum effect, it is necessary to take a dose of the drug 10–20 times larger, since a significant part of the enzyme acts as ballast. If we analyze in accordance with the stated requirements the entire range of enzyme preparations used in practice for replacement therapy for exocrine insufficiency pancreas, it can be noted that only two of them - Creon and pancitrate - meet these conditions. However, they differ significantly in the number of particles (minimicrospheres, microtablets) in the capsule (Fig. 7). The largest number of them is contained in the capsule of Creon 10000 and Creon 25000. It is also important that the minimicrospheres are enclosed in a capsule, which is a container that quickly breaks down in an acidic gastric environment. A large number of microspheres are easily mixed in the stomach and simultaneously enter the duodenum with food. Thus, Creon, thanks to its special dosage form, creates the most optimal conditions for cavity digestion.
Number of particles per capsule in various enzyme preparations
| A drug | Lipase content | Number of particles per capsule | |
| Creon | 8 000 | 130–150 | |
| Creon | 10 000 | 10 000 | 285–303 |
| Creon | 25 000 | 25 000 | 488–501 |
| Pancitrate | 25 000 | 25 000 | 59–63 |
Comparative characteristics of enzyme preparations depending on the dosage form and the content of enzymes in them are shown in table. 2. As can be seen from the table, the dosage form of Creon is presented in the most optimal physiological ratio of enzymes, which makes it the drug of choice for the correction of exocrine pancreatic insufficiency.
Comparative characteristics of enzyme preparations
| A drug | Components | |||
| lipase | amylase | protease | other | |
| Mezim (tablets) | 3.5 thousand ed ph eur | 4.2 thousand ed ph eur | 250 edph eur | |
| Panzinorm (dragée) | 6.0 ed fip | 7.5 ed fip | 450 ed fip | chemotrypsin 1500 ed fip cholic acid 13.5 mg |
| Creon 10000 microspheres in gelatin. capsule | 10.0 thousand ed ph eur | 8.0 thousand ed ph eur | 600 edph eur | |
| Creon 25000 microspheres in gelatin. capsule | 25.0 thousand ed ph eur | 18.0 thousand ed ph eur | 1.0 thousand ed ph eur | |
| Pancitrate capsules containing microtablets | 10.0 thousand 25.0 thousand ed ph eur | 9.0 thousand 22.5 thousand ed ph eur | 500 ed ph eur 1250 ed ph eur | |
| Festal (dragée) | 6.0 thousand ed ph eur | 4.5 thousand ed ph eur | ox bile extract | |
Clinical experience suggests that, depending on the degree of exocrine pancreatic insufficiency and the composition of the diet, the effective daily dose of Creon 10,000 for PD can range from 4 to 15 capsules. In this case, the dose of the drug should not be determined by clinical criteria, but based on data from objective tests.
To prevent cholangitis and pancreatic abscesses, broad-spectrum antibiotics are used, with preference given to those that are excreted primarily in the bile, for example, Klacid (clarithromycin) 500 mg 2 times a day.
In the presence of biliary sludge, litholytic therapy with ursodeoxycholic acid (ursosan, ursofalk) or in combination with chenodeoxycholic acid is indicated. The dose of UDCA is selected depending on the patient’s weight (on average 10–15 mg/kg); the course of treatment usually does not exceed 3 months, but can be longer if necessary. For dysfunction of the sphincter of Oddi, other drugs are also used - hepabene 1-2 capsules 3 times a day for 2-4 weeks, Odeston 200-400 mg (1-2 tablets) 3 times a day for 2-3 weeks.
In the presence of biliary hypertension, choledocholithiasis, stenotic papillitis, depending on the indications, balloon dilatation or papillosphincterotomy with removal of stones from the common bile duct is used
Chronic pancreatitis. Treatment
The basis for successful treatment of chronic pancreatitis is:
- complete exclusion of the causative factor of the disease,
- treatment of concomitant diseases of the digestive system,
- individual construction of conservative treatment.
- All patients should avoid alcoholic beverages and smoking!
Basic principles
- relief of pain, prevention of the development of complications of the disease (surgical) and creation of functional rest for the pancreas, reduction and removal of intoxication,
- correction of enzymatic insufficiency of the pancreas, disorders of digestion and absorption of food (fats, proteins, vitamins and minerals),
- correction of the intrasecretory function of the pancreas (pancreatogenic diabetes mellitus).
Relief and relief of pain with antispasmodics
Relief of pancreatic pain is a difficult task of conservative therapy. Approaches to the combination of various drugs are decided individually, based on the characteristics of the course and nature of pancreatic disorders in each patient.
It is important for patients to stop drinking alcohol!
To relieve pancreatic pain, medications of various pharmacological groups are used:
- analgesics (eg paracetamol) or non-steroidal anti-inflammatory drugs,
- antispasmodics (No-spa, Duspatalin, etc.), which normalize the outflow of bile and pancreatic juice (which reduces the pressure inside the pancreas),
- antisecretory drugs that reduce the acidity of gastric juice and thereby reduce the stimulated secretion of pancreatic juice (for example, Omez, Nexium, Kvamatel, etc.),
- in order to increase pain relief, treatment includes antidepressants and tranquilizers, which themselves have an analgesic effect and also enhance the effect of analgesics,
- pancreatic enzyme preparations (pancreatin groups), which cause a decrease in pancreatic secretion, reduce pressure inside the pancreatic ducts and reduce pain (Pancreatin, Mezim-forte, Creon, etc.)
If pain relief in chronic pancreatitis is ineffective, narcotic analgesics can be used or serve as an indication for surgical treatment.
Possible complications
The most common complication of untreated biliary pancreatitis is the parenchymal variant, when inflammation is localized in the cells of the gland tissue.
Early complications are the consequences of intoxication:
- shock;
- acute renal and hepatic failure;
- gastrointestinal bleeding;
- encephalopathy;
- pancreatic necrosis;
- development of an abscess in the pancreas;
- intestinal obstruction;
- obstructive jaundice;
- diabetic coma.
Late ones include: the formation of pseudocysts and fistulas, ascites, narrowing of the intestinal lumen
Symptoms
The main symptom of biliary pancreatitis is pain. Localization of pain can occur in the left or right hypochondrium. The attacks resemble short-term spasms or are regular. A provoking factor for pain syndrome is the consumption of certain categories of food (for example, salty, spicy, fatty or fried foods).
Other symptoms of PD may vary depending on the stage of the disease and the overall health of the digestive system.
Main symptoms:
A risk factor for the development of the biliary form of the disease is overeating. jaundice of the skin and sclera;- attacks of vomiting combined with attacks of pain localized in the digestive organs;
- frequent urge to defecate (loose stools, particles of undigested food may be present in the stool);
- heaviness in the stomach (with regular pain);
- lack of appetite (an inevitable consequence of the symptom is weight loss);
- regular attacks of nausea and uncontrollable vomiting;
- depressive disorders;
- increased body temperature;
- pain in the joints;
- general weakness of the body and excessive fatigue.
Distinctive features of PD are a feeling of bitterness in the mouth (or bitter belching) and regular constipation. Against the background of regular difficulties in the process of bowel movement, the patient may develop intestinal obstruction. Painful attacks with biliary-dependent pancreatitis last longer than other forms of this disease.
The pain is most often localized in the right hypochondrium (rather than in the left) and can move to the right arm, lower back or right shoulder blade.
Menu for a week for a diet for pancreatitis
Advice A prerequisite for a diet for pancreatitis is to divide the total daily portion into small equal parts. There should be at least 5-6 meals per day. Foods can be swapped and combined, but it is best to avoid eating two types of proteins at the same time, such as meat and cheese.
Day 1
Breakfast: curd pudding with sour cream, tea Snack: baked apple, glass of curdled Lunch: pureed potato and pumpkin soup, seasoned with sour cream Afternoon snack: 2 egg whites omelet with milk, rosehip broth Dinner: boiled beet salad, steamed tilapia
Day 2
Breakfast: boiled noodles, steamed chicken meatballs Snack: fruit jelly Lunch: mashed potatoes, boiled turkey breast Afternoon snack: applesauce, a glass of fermented baked milk Dinner: curd pudding with sour cream, tea
Day 3
Breakfast: boiled rice porridge with milk, tea Snack: 2 egg white omelette with milk, rosehip infusion Lunch: beef meatloaf, zucchini stew snack: dry biscuits with low-fat cheese, rosehip infusion, kefir Dinner: cottage cheese casserole
Day 4
Breakfast: oatmeal with diluted milk, lightly brewed tea without sugar Snack: pumpkin porridge Lunch: boiled vermicelli, steamed chicken meatballs Afternoon snack: fruit jelly Dinner: omelette of 3 eggs with milk, rosehip decoction
Day 5
Breakfast: curd pudding with sour cream, tea Snack: fruit jelly, rosehip decoction Lunch: pureed potato and pumpkin soup, seasoned with sour cream, boiled fish or beef Afternoon snack: baked apple, glass of kefir Dinner : boiled beet salad, steamed tilapia
Day 6
Breakfast: dry biscuits with low-fat cheese, rosehip broth Snack: low-fat cottage cheese 150 g, tea Lunch: steamed beef meatballs, stewed zucchini with carrots snack fruit jelly Dinner : puree pumpkin-carrot soup, steamed cod
Day 7
Breakfast: steamed chicken breast, unsweetened rosehip Snack: a jar of vegetable baby food Lunch: zucchini and potato stew, boiled lean beef, dried fruit compote Afternoon snack : a glass of low-fat kefir Dinner: omelet of 3 eggs with milk, rosehip infusion
How is a diagnosis made for problems with the sphincter of Oddi?
CT scans are used to diagnose problems with the sphincter of Oddi.
Sometimes establishing an accurate diagnosis is a rather labor-intensive process that requires several studies; this is done in the gastroenterology department. The thing is that the disease can have different forms and each of them requires careful examination and attention. In some cases, cholangiopancreatography should be performed.
But this procedure can lead to complications, so it is not used often, mainly in extreme cases. In order for a doctor to make a final verdict on identifying a disease associated with the sphincter of Oddi, the results of the following studies are needed:
- Clinical
- Laboratory
- Imaging (ultrasound, CT)
- Gauge
- Endosonographic
Patients with sphincter of Oddi problems almost always experience narrowing, which occurs as a result of chronic inflammation and fibrosis.
When starting a diagnosis, the first thing you need is liver tests and signs of amylase activity in the blood serum. This is followed by procedures such as ultrasound and computed tomography in the abdominal area. You may also need to undergo endosonography. This is necessary in order to make sure that there are no other diseases, especially the presence of stones in the bile ducts.
Enzymes in the blood serum are usually examined during the painful attacks themselves, since during this period their activity, as a rule, increases. But sometimes it can indicate other diseases, such as cancer, urolithiasis or liver problems. And if the disease causes dilatation of the bile ducts. The results of an ultrasound or computed tomography can tell you this.
Spasms and other problems of the sphincter of Oddi can be determined using manometry. The essence of this method is to measure the contractility of the sphincter of Oddi. But this method is not practiced in all clinics and its disadvantage is that it can lead to complications. Therefore, they often resort to non-invasive methods. There are several of them, for example, it is common to measure the diameter of the bile duct after its stimulation. Deposits can be avoided by performing cholangiography, which is a magnetic resonance imaging method.
Treatment prices
The cost of therapy for PD depends on many factors - the general clinical picture of the patient’s health, the degree of progression of the secondary disease, and the set of procedures necessary for treatment. If the patient is examined in a public institution, then the main costs will involve drug therapy.
When observed in paid clinics, the price of diagnosis and treatment of PD will be several times higher. The average cost of therapy is 8,000 rubles.
Causes of sphincter of Oddi dysfunction
Today there are many known reasons that can disrupt the functioning of the sphincter of Oddi, but the most famous include the following:
- Changes in the composition of bile
- Passage violations
- Increased bacterial growth in the intestines
- Previous surgical interventions
- Passage violations
- Dyskinesia (spasms)
- Structural abnormalities or changes associated with stenosis
How to treat
Treatment of PD is carried out comprehensively. The main goal of therapy is to eliminate the factor that provoked the pathological reflux of bile. At this stage, medication or surgical techniques may be used. Eliminating the root cause of the disease significantly reduces the risk of re-development of pancreatitis and the pathology becoming chronic. The second part of the therapy is aimed at pain relief and maximum improvement of the functional state of the liver, gallbladder and pancreas.
Stages of treatment for PD:
- relief of pain and relief of the patient’s condition;
- detoxification therapy;
- restoration of the secretion process of the pancreas;
- prevention of infectious pathological processes;
- removal of stones (if any);
- restorative therapy.
Conservative treatment
In the absence of complications that pose a threat to the patient’s life, treatment of PD is carried out using a conservative method. Therapy includes taking certain groups of drugs, following a diet and replenishing the supply of vitamins in the body.
The treatment regimen is drawn up individually. Medicines for the treatment of acute and chronic pancreatitis are different.
Examples of drugs for the treatment of PD:
- antispasmodics for pain relief (No-Shpa, Duspatalin);
- enzyme preparations to improve the functional state of the pancreas (Pancreatin, Creon, Mezim);
- ursodeoxycholic acid preparations for dissolving small stones (Ursosan, Ursofalk);
- medications from the prokinetic category (Motilium, Cerucal, Domperidone);
- combined agents (Hepatofalk, Odeston);
- proton pump blockers (Emanera, Omeprazole).
Surgery for biliary pancreatitis
In recent years, the number of patients with biliary pancreatitis has approximately doubled. The need for surgical intervention arises in the presence of complications. Indications for surgery are cicatricial narrowing or obstruction of the bile ducts, cholelithiasis or tumors of the papilla of Vater. When choosing surgical methods, specialists give preference to low-traumatic procedures (endoscopic options using micro-instruments and a camera). If it is not possible to use such methods, open laparotomy operations are performed.
Types of surgical intervention:
- laparoscopy (the operation is performed through small incisions in the abdominal wall);
- lithotripsy (a procedure for crushing stones using special equipment);
- laparotomy (the procedure is aimed at removing the gallbladder and stones; the operation is performed by opening the anterior abdominal wall).
Folk ways to combat the disease
Herbal medicine is a good addition to traditional therapy. Some medicinal herbs contain components that not only improve the general condition of the digestive system, but also accelerate the tendency to recovery, have a beneficial effect on the composition of bile and to some extent stop the inflammatory process. Decoctions from such plants are prepared according to the standard procedure (a teaspoon of herb or a mixture of herbs is poured with boiling water, infused and consumed in small portions).
Medicinal plants for the treatment of PD:
- celandine;
- tansy;
- fennel;
- white birch leaves;
- dandelion;
- immortelle;
- corn silk;
- calendula;
- peppermint.