Chest pain is considered very dangerous, because these sensations occur in the most complex diseases. Among them are coronary heart disease and esophageal ulcer. Each of these diseases can be fatal.
But if the first requires emergency measures, then esophageal diseases are much easier to correct. Therefore, when pain occurs in the chest, it is necessary to differentiate between cardiac pathology and esophageal lesions.
Features of peptic ulcer of the esophagus
Antibiotics can cause ulcers.
To cure this disease, you need to identify the cause of its occurrence.
Therefore, it is so important to understand its features and know the main symptoms of each stage of development.
Then a properly selected diet and adequate therapy will help avoid the development of adverse consequences.
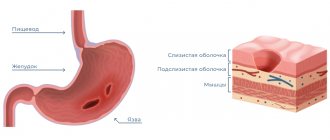
A peptic ulcer is a disease of the esophageal mucosa, manifested in a deep defect in this lining.
Appears when a combination of weakening the body’s protective abilities and destructive external influences occurs.
The destructive effect can come from both food and other chemically aggressive substances entering the body. The following substances may cause ulcers:
What causes peptic ulcers?
Most peptic ulcers are caused by:
- Helicobacter pylori (H. pylori) - bacteria that cause infection
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen
H. pylori is the most common cause of peptic ulcers. Doctors believe H. pylori can be spread through dirty food or water, or from mouth to mouth, such as by kissing. Although many people are infected with H. pylori, most never develop an ulcer. NSAID use is the second most common cause of peptic ulcers. But not all people taking NSAIDs get peptic ulcers. Ulcers caused by NSAIDs are most often found in people
- over 60 years old
- female
- long-term users of NSAIDs
- who have previously had an ulcer
Other causes of peptic ulcers are rare. One rare cause is Zollinger-Ellison syndrome, a condition in which the body produces too much stomach acid, which damages the lining of the stomach or duodenum.
Stress or spicy foods do not cause peptic ulcers, but they can make the ulcers worse or prevent them from healing.
Signs of an esophageal ulcer
Acid belching is a sign of an esophageal ulcer.
This disease can be recognized by several common signs:
- Burning pain behind the chest, which intensifies after eating, especially after physical exertion after eating. Such pain can be very disturbing at night. After all, pain on an empty stomach is another sign of an ulcer. This is due to inflammation of the affected area, which is caused by gastric juices left idle due to lack of food.
- Dyspepsia.
- Sour belching, possible regurgitation.
Specific signs are largely determined by the nature of the ulcer and the reasons that provoked it. For example, with GERD, heartburn is felt before the pain. If liberties are taken in nutrition, the diet is disrupted, then heartburn becomes very severe, and only then does pain occur.
Heartburn is a consequence of an imbalance in the acid-base balance. The environment of the esophagus is normally alkaline, therefore, when acid enters there, malfunctions occur in the functioning of the protective mechanism.
There are cases when an esophageal ulcer is not felt at all. This is the so-called silent form. The presence of such an ulcer may be indirectly indicated by minor signs of heartburn after playing sports.
When a person makes sharp bends and turns, gastric juice is thrown into an unusual place, which is why heartburn is felt. A similar situation can arise when the patient is lying down.
Etiology, pathogenesis.
Of primary importance is the violation of the trophism of the esophageal wall and the constant impact of active gastric juice on it due to cardia insufficiency and gastroesophageal reflux. It is most often observed in axial hiatal hernias, after operations on the esophagogastric junction, and in systemic scleroderma. Impaired gastric motility and increased tone of the pylorus, which constantly accompany peptic ulcer disease (which contributes to the reflux of gastric juice into the esophagus), are also one of the pathological factors in the occurrence of peptic ulcer of the esophagus.
Treatment of esophageal ulcers
An ECG will not give a complete picture of a person’s condition.
If the lesion is not complicated and is small in size, then it can be treated on an outpatient basis. But multiple ulcers and extensive lesions are treated exclusively in a hospital.
They use medications selected according to the cause of the disease. GERD requires medications that can stop the increased production of hydrochloric acid.
For pathologies of the stomach, gallbladder, pancreas, and duodenum, those remedies are used that help cure the underlying disease. In addition to remedies aimed at eliminating the underlying disease, symptomatic therapy is used:
- antacids (reducing acidity);
- bismuth;
- prokinetics (restoration of sphincter functionality);
- proton pump blockers (reducing inflammation, restoring the functionality of the glands);
- painkillers.
Of course, the success of treatment depends, first of all, on diet. To make healing possible, you should not eat spicy or fried foods, and you should not indulge in smoked or fatty foods.
Food must be boiled, stewed, even raw vegetables and fruits should not be eaten. After all, they can also irritate the mucous membranes. If the patient suffers from severe chest pain, he must be examined in depth. After all, ECG, CBC, OAM cannot give a complete picture of a person’s condition.
A comprehensive examination allows you to timely diagnose an esophageal ulcer, prescribe the correct treatment and neutralize the manifestations of this unpleasant disease.
Symptoms, course.
The main symptom is pain behind the sternum or in the epigastric region, which occurs or worsens during or immediately after eating, when swallowing food, sometimes while lying down (due to reflux of gastric juice into the esophagus). Often the pain resembles coronary pain in nature. Dysphagia, heartburn, belching, and regurgitation of acidic gastric contents are common. Heartburn and regurgitation usually worsen when bending over or lying down. An X-ray examination reveals a peptic ulcer as a niche on the contour or relief of the mucous membrane, but it is difficult to identify. The most reliable diagnostic method is esophagoscopy. Stool examination often reveals positive reactions to occult bleeding.
Complications: profuse or occult esophageal bleeding, ulcer perforation, development of esophageal stricture during scarring of the ulcer, cicatricial shortening of the esophagus, which causes the formation or gradual increase of an existing axial hiatal hernia.
Differential diagnosis is carried out with ulcers of the esophagus of a different nature: cancerous, tuberculous, syphilic, decubital; Of primary importance is esophagoscopy, the study of gastric juice (which should be carried out carefully); reliably established achlorhydria rejects the peptic nature of the ulcer.
Prevention comes down to measures to prevent the formation of a hiatal hernia and to prevent the occurrence of gastroesophageal reflux in diseases accompanied by the development of cardia insufficiency: high head of the bed while sleeping and lying down, early dinner (2.5–3 hours before bedtime), avoidance of all types of work associated with bending the body.
Treatment is carried out in a hospital. An anti-ulcer diet is prescribed. It is recommended to lie in bed with the upper half of the body elevated (to prevent gastroesophageal reflux). Treatment is usually long-term (1.5–2 months or more). Surgical treatment is indicated in the absence of effect from conservative treatment, as well as in the presence of complications of the disease. Patients with peptic ulcer of the esophagus need clinical observation and systematic (2-4 times a year) anti-relapse treatment with astringents and antacids.
Features of the diet during exacerbation
Broccoli - has healing properties.
To ensure that dishes do not cause harm during an exacerbation of peptic ulcer disease, you must adhere to the recommendations for their preparation given below:
- The meat is stewed, boiled, steamed. It is advisable to pre-twist it (cutlets). Broth is made from chicken and drunk.
- Dairy with less than 2.5% fat content, thermally gentle (not cold). Milk, yogurt, cottage cheese are acceptable.
- Eggs in the form of an omelet or soft-boiled.
- Milk porridge, ground.
- Vegetable puree, vegetables are boiled, baked.
It is important that the patient eats broccoli. This cabbage has healing properties. It can be cooked in the microwave with nuts and cheese.
First, place only the broccoli, covered with a paper towel, after a minute and a half, sprinkle with grated nuts and cheese. Cook for another minute. It turns out tasty and healthy.
What are the symptoms of peptic ulcers?
Dull or burning pain in the stomach area is the most common symptom of peptic ulcers. You may feel pain in any area, from the navel to the sternum. Pain often
- appears between meals or at night
- stops quickly with food or antacids
- lasts from several minutes to several hours
- appears and lasts for several days or weeks
Other symptoms of peptic ulcers may include
- weight loss
- poor appetite
- bloating
- belching
- vomit
- discomfort in the stomach
If you experience even mild symptoms, you may have a peptic ulcer. You should visit your doctor to discuss your symptoms. Without treatment, peptic ulcers worsen.
Call your doctor right now if you experience
- sudden sharp pain in the stomach that does not go away
- black or bloody stools
- bloody vomit or vomit that looks like coffee grounds
How to diagnose peptic ulcers?
Tell your doctor about your symptoms and what medications you are taking. Be sure to tell us about the medications you are taking without a prescription, for example, if these medications are NSAIDs.
To find out if you are infected with H. Pylori, your doctor will do a blood, breath, and stool test. About half of all people who develop ulcers from taking NSAIDs are also infected with H. Pylori.
Your doctor may also decide to examine the lining of your stomach and duodenum using endoscopy or by taking a series of pictures of the upper gastrointestinal (GI) tract, the latter of which is a type of x-ray. Both procedures are painless.
During the endoscopy, you will be given a relaxant medication. The doctor will then insert an endoscope—a thin, light-equipped tube with a miniature camera—through your mouth and into your stomach and duodenum. Also during the procedure, your doctor may remove a small piece of tissue—no larger than the head of a match—to examine it under a microscope. This process is called a biopsy.
For upper gastrointestinal series, you will drink a liquid called barium. Barium will make your stomach and duodenum clearly visible on x-rays.
How to treat peptic ulcers?
If you have peptic ulcers, they need to be treated. Depending on the cause of the ulcers, your doctor may prescribe one or more of the following medications:
- a proton pump inhibitor (PPI) or a histamine receptor blocker (H2 blocker) to reduce stomach acid production and protect the lining of the stomach and duodenum
- one or more antibiotics to kill H. Pylori
- a drug containing bismuth subsalicylate to coat ulcers and protect them from stomach acid. These drugs will relieve pain and promote healing of ulcers.
If your peptic ulcers are caused by taking NSAIDs, your doctor may advise you
- stop taking NSAIDs
- reduce the dose of NSAIDs you take
- taking a PPI or H2 blocker along with an NSAID
- switch to using another drug that will not cause ulcers
You must accept
- only medications prescribed by a doctor
- all medications, strictly following your doctor's instructions, even if the pain has passed
Tell your doctor if your medications cause nausea, dizziness, diarrhea, or headaches. Your doctor may prescribe other medications for you. And if you smoke, then stop smoking. You should also avoid drinking alcohol. Smoking and drinking alcohol slow down the healing of ulcers and can worsen their course.
Can antacids or milk help peptic ulcers heal?
Neither antacids nor milk can heal peptic ulcers, although either remedy may provide short-term relief. Talk to your doctor before taking antacids or drinking milk while your ulcers are healing.
Some antibiotics used to eradicate H. Pylori may not work as well when taken with antacids. Although antacids can temporarily relieve ulcer pain, they cannot kill H. Pylori bacteria. Only antibiotics can do this.
Many people tend to think that drinking milk helps peptic ulcers heal. But doctors now know that while milk may temporarily make ulcers feel better, it also increases stomach acid production. Excess stomach acid worsens the ulcer.
What to do if peptic ulcers do not heal?
In most cases, the drugs cure the ulcers. If the occurrence of your ulcers is associated with infection with H. Pylori, then you must complete the course of treatment with all antibiotics and take all other medications prescribed by your doctor. Getting rid of the infection and healing of the ulcers will only happen if you take all medications as prescribed.
When you finish taking the medications, your doctor will test your breath or stool to make sure the H. Pylori infection has been eradicated. Sometimes H. Pylori bacteria continue to remain in the body even after the patient has taken all medications correctly. If this happens, your doctor will prescribe other antibiotics to clear up the infection and treat the ulcers.
In rare cases, surgery is necessary to heal the ulcers. Surgery may be required if your ulcers
- don't heal
- relapse
- are bleeding
- perforate the wall of the stomach or duodenum
- interfere with the passage of food from the stomach
During surgery it is possible
- removal of ulcers
- reducing the amount of acid produced in your stomach
Can peptic ulcers recur?
Yes. If you smoke or take NSAIDs, your ulcers may recur. If you need to take NSAIDs, your doctor may prescribe another drug or additional medications to prevent ulcers.
What can I do to prevent peptic ulcers?
To prevent ulcers caused by H. Pylori
- wash your hands with soap after using the toilet and before eating
- eat only clean and properly prepared foods
- drink only clean water from safe sources
To prevent ulcers caused by NSAIDs
- stop taking NSAIDs if possible
- If you are advised to take NSAIDs, take the NSAID with food.
- take lower doses of NSAIDs
- Talk to your doctor about medications that may protect your stomach and duodenum when you take NSAIDs.
- Talk to your doctor about switching you to a drug that does not cause ulcers.