Hemorrhoids are a disease that develops over many years. Initially, it may not cause a person any noticeable discomfort. The pain may be temporary and pass quickly.
Most people prefer not to attach importance to temporary discomfort and do not rush to visit a doctor, thereby allowing the disease to develop and complicating the treatment process. Hemorrhoids cannot go away on their own and will only progress, causing a person more and more discomfort and harm to health.
Over time, patients begin to notice blood on toilet paper and underwear, and the pain intensifies and does not go away as quickly as before. Additionally, burning and itching occur. The more advanced the disease, the more difficult it is to treat. Therefore, it is important to make an appointment with a doctor at the first symptoms in order to receive effective treatment and prevent the development of the disease. In the early stages, the disease can be successfully treated by modern medicine using conservative methods.
What are external hemorrhoids? A little anatomy
External hemorrhoids (plexuses) are formations located under the skin on the border of the anal canal and perianal (around the anus) skin. They are venous plexuses (Fig. 3). Usually they do not manifest themselves in any way, are not visible and cannot be detected by touch. As the condition worsens chronically
changes occur in internal hemorrhoids and in external hemorrhoids, leading to their enlargement and loss of connection with the muscular ring of the anal canal. However, the most significant changes in the external nodes occur when a blood clot occurs in them.
Rice. 3. Diagram of the anal canal, at the exit of which the external hemorrhoids are located (number 7 in the diagram).
Can a hemorrhoid go away on its own?
Hemorrhoids and the formation of nodes are pathological changes in tissues that arise as a result of various reasons. This disease cannot go away on its own without professional treatment. In the early stages of the disease, the doctor prescribes complex therapy to successfully combat the pathology. If you do nothing or self-medicate, deterioration cannot be avoided.
There is no point in waiting for a hemorrhoid to go away on its own. Any person who cares about his own health and is interested in preventing the development of diseases, that timely consultation with a doctor is the key to a speedy recovery. You should treat your own health responsibly, then you can maintain it until old age.
How does acute thrombosis of the external hemorrhoid manifest?
Patients with acute thrombosis of the external hemorrhoid complain of a protrusion, “bump” (neoplasm) and/or pain of varying intensity in the anus. The size of the “bump” can range from several millimeters to several centimeters and is often accompanied by swelling of the surrounding tissues (up to the entire circumference of the anal canal). In some patients, the disease proceeds without pain, but most assess the pain as significant or unbearable.
To assess the degree of pain, a special visual analogue scale is used, in which you can independently determine the severity of pain. After all, this is the key point when choosing a treatment method. Surgical treatment will be most effective when the severity of pain is 7 or more points, while for pain up to 4 points, a conservative method of treatment can be considered optimal.
Rice. Visual analogue scale for pain assessment.
Pain usually worsens during bowel movements and/or sitting. The pain and swelling can be severe, even unbearable for several days. The intensity of pain depends on the size of the blood clot and its location in relation to the anal sphincter muscles. In general, manifestations of the disease can persist for several weeks, in exceptional cases longer. Sometimes spontaneous evacuation of a blood clot from a hemorrhoid occurs. This is preceded by necrosis (destruction) of the skin over the thrombus, and the thrombus seems to “fall out” of the node. Externally, this is accompanied by the sensation of a “bursting” ball and the release of a small amount of blood. Usually, after evacuation of the blood clot, the pain and discomfort in the anus gradually decrease. However, necrosis of the mucous membrane above the thrombus does not always end only with the evacuation of the thrombus; necrosis can continue to spread to the hemorrhoid itself and surrounding tissues, which is why this condition requires consultation with a specialist. After acute thrombosis subsides, the patient is most often left with so-called “skin fringes” - excess skin where the thrombosis was. They do not require medical treatment, but may cause cosmetic discomfort.
What to do if hemorrhoids prolapse?
If the disease has developed so much, there is only one way out - an immediate visit to the doctor. If you have been self-medicating before, the prolapse of the node is a natural stage in the development of the disease. It’s time to put aside the embarrassment and feeling of discomfort, since the disease has reached a dangerous stage.
If a prolapse occurs, and you feel it, but the node is set on its own, there is hope that the doctor will be able to correct the situation without surgical intervention. The proctologist decides whether to use conservative treatment methods or not in each case individually. The clinical picture may vary significantly between patients. Therefore, only a comprehensive diagnostic study will allow the proctologist to make the only correct decision.
If a node falls out, but then it returns to its place on its own, this does not mean that it will not happen again. The patient must be aware that without comprehensive professional treatment, the disease will only progress.
If nodes fall out in a situation where they have to be set manually, treatment is carried out only surgically. After this, the patient is prescribed complex therapy and given recommendations on the nutritional system. Since serious pathological changes have occurred in the tissues of the anal canal and rectum, the likelihood of relapse is high. Therefore, it is important to strictly follow medical recommendations.
The occurrence of hemorrhoids is a problem that many people face. Do not hesitate to visit a proctologist at the first feeling of discomfort during bowel movements. This will help you avoid more serious problems and quickly restore your health.
What causes acute thrombosis of the external hemorrhoid?
The occurrence of thrombosis is often caused by overflow of the veins of the external hemorrhoidal plexus with blood, followed by a slowdown in blood flow in these vessels and the occurrence of blood clots. Thrombosis against the background of venous congestion most often develops after sudden or prolonged stress. Classic examples of such overexertion are heavy lifting, straining during constipation or diarrhea, and childbirth. Chronic stagnation of blood in the pelvic organs (which includes the anal canal) occurs with prolonged sitting, excess body weight, and insufficient physical activity.
Minimally invasive methods for treating external hemorrhoids
Minimally invasive methods of treating external hemorrhoids are used when there is no effect from the use of medications. In this case, preference is given to two methods, which in case of combined hemorrhoids are applied to internal nodes, which helps to stabilize the process:
- Infrared coagulation - for hemorrhoids at stages 1 and 2.
- Ligation with latex rings - at stages 2 and 3.
They are used only if there are contraindications, which are purulent or acute paraproctitis, thrombosis or the presence of anal fissures.
Sclerotherapy for external hemorrhoids is not used due to ineffectiveness and high risk of complications.
How to distinguish acute thrombosis of the external hemorrhoid from other diseases?
Usually, to diagnose acute thrombosis, it is enough to examine the patient and find out how the disease developed and what complaints are of concern. Upon examination, you can see an enlarged (sometimes up to several centimeters) node, often dark red in color, located outside the anus, possibly with a focus of necrosis in the center. When palpating (feeling) in the first few days, you can clearly identify a blood clot in the node; when examined at a later date, the blood clot is no longer so easy to determine; it begins to gradually “dissolve” and is partially replaced by scar tissue. Thrombosis of the external hemorrhoid must be distinguished from
strangulation of a prolapsed internal hemorrhoid. In this situation, prolapse of the internal hemorrhoidal node, normally located inside the anal canal, compression of its pedicle, in which the vessels feeding it pass, and disruption of the blood supply (ischemia) with death of the tissue of the node (Fig. 4 and 5). It is not difficult for a specialist to distinguish between these conditions, but it is quite difficult for a patient to independently understand which node is causing him discomfort. It is important to distinguish between these diseases, as their treatment varies significantly. When an internal hemorrhoid is strangulated, urgent surgical treatment is usually required.
Rice. 4. A strangulated prolapsed internal hemorrhoid with signs of tissue necrosis of the node.
Fig.5. Schematic representation of a strangulated internal prolapsed hemorrhoid.
Acute (exacerbation of chronic) anal fissure - accompanied by the same pain syndrome as with thrombosis, but much more pronounced at the time of bowel movement. With this disease, a rupture of the anal canal mucosa occurs. The appearance of an acute fissure is often associated with a reflex “protective” spasm of the sphincter apparatus, which complicates wound healing. Conservative and surgical treatment of diseases are different.
Acute paraproctitis - similarity with acute thrombosis lies in the appearance of a space-occupying formation in the anus, severe pain. Paraproctitis is an infectious and inflammatory disease with the formation of an abscess (abscess) in the pararectal area. The disease is accompanied by an increase in body temperature and general symptoms of intoxication. A mass formation in the anal canal area is much larger and more painful than with thrombosis. There is often discharge of pus onto the skin or into the lumen of the rectum. Ultrasound examination is used for accurate diagnosis. The disease is extremely dangerous due to the development of chronic purulent fistulas of the perianal area in the absence of adequate and timely treatment.
What is external hemorrhoids
External hemorrhoids are a form of disease in which the venous plexuses undergo pathological changes characteristic of this disease. They expand, acquire a heterogeneous structure and cannot perform their functions normally due to weakening of the valves.
Nodes in external hemorrhoids are localized not under the mucous membrane of the rectum, but in the subcutaneous layer near the anal sphincter. The main difference between this form of the disease and the internal one is the extremely low likelihood of bleeding and more pronounced pain during exacerbations of the disease.
Is it always necessary to treat acute thrombosis of the external hemorrhoid?
The choice of treatment method for this disease is one of the most controversial issues in general proctology. Like hemorrhoids, acute thrombosis does not turn into cancer, does not cause deadly complications, but can significantly affect the patient’s quality of life; the pain syndrome is often described as “unbearable”, with which it is “simply impossible to live.”
Our Clinic has adopted a patient-centered approach to choosing a treatment method for acute thrombosis of external hemorrhoids: the doctor, together with the patient, determine how severe the symptoms are, how much the patient’s quality of life suffers, taking into account his employment, and choose a treatment method.
Acute thrombosis of the external hemorrhoid can be treated promptly (perform surgery), conservatively (take pills and use topical ointments and/or suppositories) or not treat at all, but choose a wait-and-see approach. Research and practical experience show that surgical treatment allows you to get rid of the manifestations of the disease in a shorter time; conservative treatment also allows you to get rid of the manifestations of the disease, but over a much longer time. The absence of any treatment also ends with recovery, the timing of which differs only slightly from the timing of intensive conservative treatment. The determining factor in the choice of treatment method is the patient’s choice and his assessment of the severity of the pain syndrome, therefore, the patient’s opinion is crucial for the choice of tactics. If the patient assesses the pain as unbearable, or he urgently needs to return to work, fly to another city or country, it is more reasonable to choose surgical treatment in the scope of removing the hemorrhoidal node or evacuating the blood clot from the node. Surgical treatment usually leads to faster relief of unpleasant symptoms. If the pain syndrome allows the patient to live fully in this condition or the patient is not ready for surgical intervention, it is possible to carry out conservative treatment aimed at reducing the pain syndrome and accelerating the process of organizing and resolving the blood clot.
How many hemorrhoids can there be?
There can be no exact answer to this question. Each person is individual, so everything depends on the degree of neglect of the disease and the characteristics of the tissues of the rectum and anal canal. There may be one such node, but most often there is a situation where there are several formations.
It should also be noted that simply surgical treatment cannot completely eliminate the problem. Since pathological changes have occurred in the tissues, the likelihood of relapse is high. After surgery, it is important to take medications prescribed by your doctor that increase blood flow, and introduce physical exercises recommended by your doctor to prevent blood stagnation. Patients are also prescribed medications that strengthen blood vessels and prevent their abnormal enlargement.
Special attention should be paid to diet. It is important to ensure a balanced diet, consume the amount of fiber recommended by your doctor and drink enough water to ensure normal bowel function. You will also need to exclude alcohol and spicy foods from food, so as not to artificially create conditions for increasing pressure in the hemorrhoidal veins. After surgical treatment, complex therapy is important, which only the attending physician can prescribe. Under no circumstances should you self-medicate, as this is a recipe for relapse.
How to treat acute thrombosis of external hemorrhoids?
Possibilities of surgical treatment
There are two main operations for the treatment of acute thrombosis of an external hemorrhoid: removal of the entire node or just the thrombus from it. The first operation is called economical (partial) hemorrhoidectomy (removal of only the external hemorrhoid), the second is thrombectomy. Both operations are effective in terms of eliminating pain within 2-3 days after their implementation, however, after an operation to evacuate a blood clot, a relapse (reoccurrence of a blood clot) is more common.
Economical (partial) hemorrhoidectomy of a thrombosed node involves incision of the skin around the node, its isolation and removal along with the thrombus. The operation can be performed under local anesthesia.
After removal of a hemorrhoid, a small wound surface is formed, which can cause pain, especially during bowel movements. But usually the pain is much less pronounced than in the presence of a thrombosed node, and only sometimes requires taking tablet painkillers.
Thrombectomy is performed through a skin incision over the thrombus, after which the thrombus is removed and 1-2 sutures may be placed at the incision site. This intervention is almost always performed under local anesthesia.
Conservative treatment
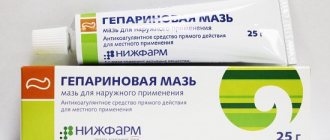
Conservative treatment (tablets and local remedies - ointments and suppositories) is mainly aimed at relieving pain caused by a blood clot, reducing swelling and inflammation of the hemorrhoid, and normalizing the frequency and quality of stool. Pharmacies offer a large number of drugs for the treatment of hemorrhoidal disease, but they are all approximately equal in effectiveness and can be used to treat acute thrombosis of the external hemorrhoid. Local remedies (ointments and suppositories) mainly have an analgesic and anti-inflammatory effect. Topical agents with an anticoagulant effect in the treatment of acute thrombosis are effective only for the temporary prevention of new blood clots or, if the drug contains an analgesic component, for pain relief. Tablets are also used for pain relief (non-steroidal anti-inflammatory drugs, paracetamol) and normalization of venous blood flow in the pelvis (in the rectal area), for example, flavonoids. In addition, conservative treatment is also carried out after surgery to eliminate possible postoperative symptoms. A conservative treatment regimen can only be determined by a specialist, and it is better to select a combination of drugs in each specific case, depending on the characteristics of each patient.
Treatment methods for hemorrhoids
Hemorrhoids in the initial stages are treated with conservative methods. Patients are prescribed oral medications, as well as topical ointments and suppositories. Modern medications, if you consult a doctor in a timely manner, help get rid of this problem. In advanced cases, surgical treatment is used. There are four stages of disease development. Depending on the clinical picture, specialists prescribe a treatment regimen. It is important, despite the intimate side of the problem, to contact a proctologist in a timely manner, who, after a thorough diagnosis, will develop an appropriate treatment regimen. Under no circumstances should you put off visiting a proctologist. Another common mistake is trying to self-treat. Many do not consider this disease dangerous and try to combat the problem with the help of traditional medicine or medications purchased without a prescription at the pharmacy. This should not be done under any circumstances, since self-medication will not only not solve the problem, but can also aggravate the situation and bring the disease to a more complex stage. Only an experienced specialist can offer comprehensive treatment, as a result of which the patient can recover.
What will happen after the operation?
Typically, patients feel dramatic relief after surgery and note a decrease in pain (Fig. 6). Sometimes continued minimal pain therapy is required. The main task of the patient in the postoperative period is to normalize stool: soft stool causes much less pain during bowel movements than dense stool. As a rule, patients return to their normal lives 2-3 days after surgery, sometimes the very next day.
a) b)
Rice. 6. View of the anus before (a) and immediately after removal of the external hemorrhoid (b). Before the operation, the patient rated the pain level as 8 out of 10, immediately after the operation it was 4 out of 10.
Conservative method - medications for external hemorrhoids
The conservative or medicinal method is used mainly in the stage of exacerbation of external hemorrhoids, and is a set of measures designed to reduce symptoms, relieve inflammation and prevent the formation of blood clots. A number of dosage forms are used:
- tablets for oral administration with antithrombotic (phlebotropic), analgesic and anti-inflammatory effects;
- external and local agents in the form of creams and ointments with analgesic and anti-inflammatory effects;
- rectal suppositories (used mainly in the presence of anal fissures).
All medications for external hemorrhoids are prescribed by a doctor in accordance with the existing symptoms and taking into account the characteristics of the patient’s body. The most effective are gels and ointments with heparin, antibiotics, anesthetics and glucocorticosteroids - Proctosedyl, Posterisan, Aurobin and Hepatrombin. Applications with Heparin ointment and Vishnevsky ointment are also used.
Oral drugs with venoprotective and venotonic properties have also proven themselves: Detralex, Phlebodia 600, Venarus, Ginkor Forte, Axlezan A and Pilex. In case of exacerbation of hemorrhoids, it is possible to take non-steroidal anti-inflammatory drugs: Ibuprofen, Diclofenac, Indomethacin.
Are there ways to prevent relapses/recurrences of the disease?
Prevention of relapse of the disease is based on excluding possible causes of thrombosis. These include hard stools, constipation or diarrhea, “reading on the toilet,” insufficient or, conversely, excessive physical activity (weightlifting, fitness), and prolonged sedentary work. Unfortunately, there are no unambiguous methods for preventing the occurrence of acute thrombosis of the external hemorrhoid; we can only reduce the likelihood of its occurrence, but not completely eliminate it. However, it should be noted that with conservative treatment the likelihood of recurrence of the disease is higher than after operations.
Do I need to remove a hemorrhoid?
After a comprehensive diagnosis, every proctologist will be able to answer this question unequivocally. It all depends on the individual clinical picture. In the initial stages of the disease, conservative complex treatment is successfully used and helps patients get rid of the disease. You should not self-medicate so that the disease does not develop before the nodes fall out, because then there is no other way other than surgery
Prolapse of hemorrhoids not only brings significant discomfort, but also causes pain. It is important to understand that hemorrhoids are injured, become inflamed and can degenerate from benign to malignant. Therefore, they must be removed immediately.
It is important that if you experience any uncomfortable sensations in the rectum or anal canal, discard false shame and consult a proctologist.
Responsibility for the health of an adult lies entirely with him. Doctors, using modern treatment methods, are always ready to help. It is important that seeking qualified help is timely. The sooner a disease such as hemorrhoids is diagnosed, the easier it will be to get rid of it and prevent the situation from worsening. Only an experienced proctologist can help with this.
What should pregnant women and postpartum women/mothers with acute thrombosis do?
According to statistics, about a quarter of pregnant women and almost half of postpartum women experience various manifestations of hemorrhoidal disease, the most painful of which is acute thrombosis. Usually, postpartum women and especially pregnant women, in response to their complaints to the doctor, hear an offer to be patient. This approach is dictated by the fact that there are many contraindications to the use of the vast majority of medications in pregnant women, and surgical intervention is regarded by the medical community as a factor that can provoke childbirth or stop the process of breastfeeding. In practice, this means that regardless of the severity of the pain syndrome, sometimes very significant, women are forced to remain without any effective treatment. Pain due to thrombosis, in turn, can worsen the psychological state of pregnant or postpartum women and lead to undesirable consequences during childbirth (premature birth) or during breastfeeding (refusal to breastfeeding). Our clinic is a supporter of a personalized approach to the treatment of acute thrombosis in such women. If acute thrombosis categorically prevents the patient from living, it should be actively treated using the entire arsenal of means used in ordinary patients, but taking into account contraindications for medications. In pregnant women in the second and third trimesters, it is possible to perform an operation to remove a thrombosed node (Fig. 7), as well as in postpartum women and women in labor (Fig. 8). During pregnancy, there are some restrictions on the local and general anesthetic drugs that can be used. Specific medications should be selected jointly by both the coloproctologist and the obstetrician so as not to harm the fetus or newborn. The specialists of our Clinic have experience in treating both pregnant and postpartum women with manifestations of acute thrombosis of the hemorrhoid with very good results, reviews of which our patients leave on our website, among other things.
a) b)
Rice. 7. Acute thrombosis of the external hemorrhoid in a 38-week pregnant woman.
Before surgery, pain was rated 8 out of 10, immediately after surgery 3 out of 10.
a) appearance of a thrombosed external hemorrhoid with necrosis, b) appearance after removal of the thrombosed node.
a) b)
Rice. 8. a) acute thrombosis of the external hemorrhoid with severe swelling in the patient on the 5th day after birth, b) the patient’s condition on the 7th day after surgery. On the first day after surgery, pain decreased from 9 to 4 out of 10.
You can read about the treatment of other manifestations of hemorrhoidal disease in pregnant women and postpartum women in the section Hemorrhoids in pregnant women .
What are the dangers of external hemorrhoids - complications
The external form of hemorrhoids is not dangerous in terms of the sudden occurrence of rectal bleeding, but if the disease is not treated, it can have a number of unpleasant consequences. Most often, the lack of treatment for external hemorrhoids is complicated by inflammation of the tissues surrounding the node changed by the disease. This complication can be recognized by redness of the skin near the anus, swelling and increased body temperature. In the absence of therapy, inflammation is complicated by tissue necrosis and suppuration - purulent paraproctitis is diagnosed.
The second dangerous complication of external hemorrhoids is thrombosis of the hemorrhoid. Symptoms of this complication are bursting pain in the anus at rest and acute pain with straining and defecation. When thrombosis occurs, the node becomes bluish and swells. Often the swelling spreads to the buttocks and perineum.
What to do if you have undergone a course of conservative treatment for thrombosis
The abundance of means for the conservative treatment of thrombosis and often the doctor’s disposition to use this technique leads to the fact that most thromboses are treated conservatively. Patients come to our Clinic at different stages of the course of conservative therapy. Often this is a situation where, immediately after the occurrence of a blood clot, conservative therapy was started, some relief of the condition occurred, the pain syndrome decreased, but a “bump” remains in the anus and some pain. Sometimes completely healthy people come in who experienced an episode of acute thrombosis several months or years ago and are now concerned about the presence of skin “fringes,” excess skin in the anus that remain after the acute condition has resolved. They can interfere with the proper hygiene of this area and affect intimate life. What to do in this situation? And again, the main thing for the doctors of our Clinic will be the patient’s opinion. If you want to get rid of the manifestation of acute thrombosis, even if conservative treatment has already been carried out, a lot of time has passed - this can be done surgically.
What to consider when choosing a doctor and medical institution
If you are looking for a medical institution where to go for consultation and treatment of acute perianal thrombosis, then you need to pay attention to several factors.
- The institution has a proctological, and not just a general surgical or oncocoloproctological specialization.
- Knowledge of the Clinic staff about all possible methods of treating acute perianal thrombosis
- Possibility of performing minor coloproctological operations in a hospital setting at the Clinic
- Possibility of performing surgical treatment in the Clinic for “special” groups of patients - pregnant women, patients of the older age group